The document serves as a checklist and guideline for reviewing doctoral project charters, emphasizing the importance of addressing feedback for proposal approval. It details various components required in the project charter, including participant descriptions, project aims, stakeholder impacts, and ethical considerations. Additionally, it underscores the necessity of synthesizing scholarly evidence throughout the proposal to ensure academic rigor.
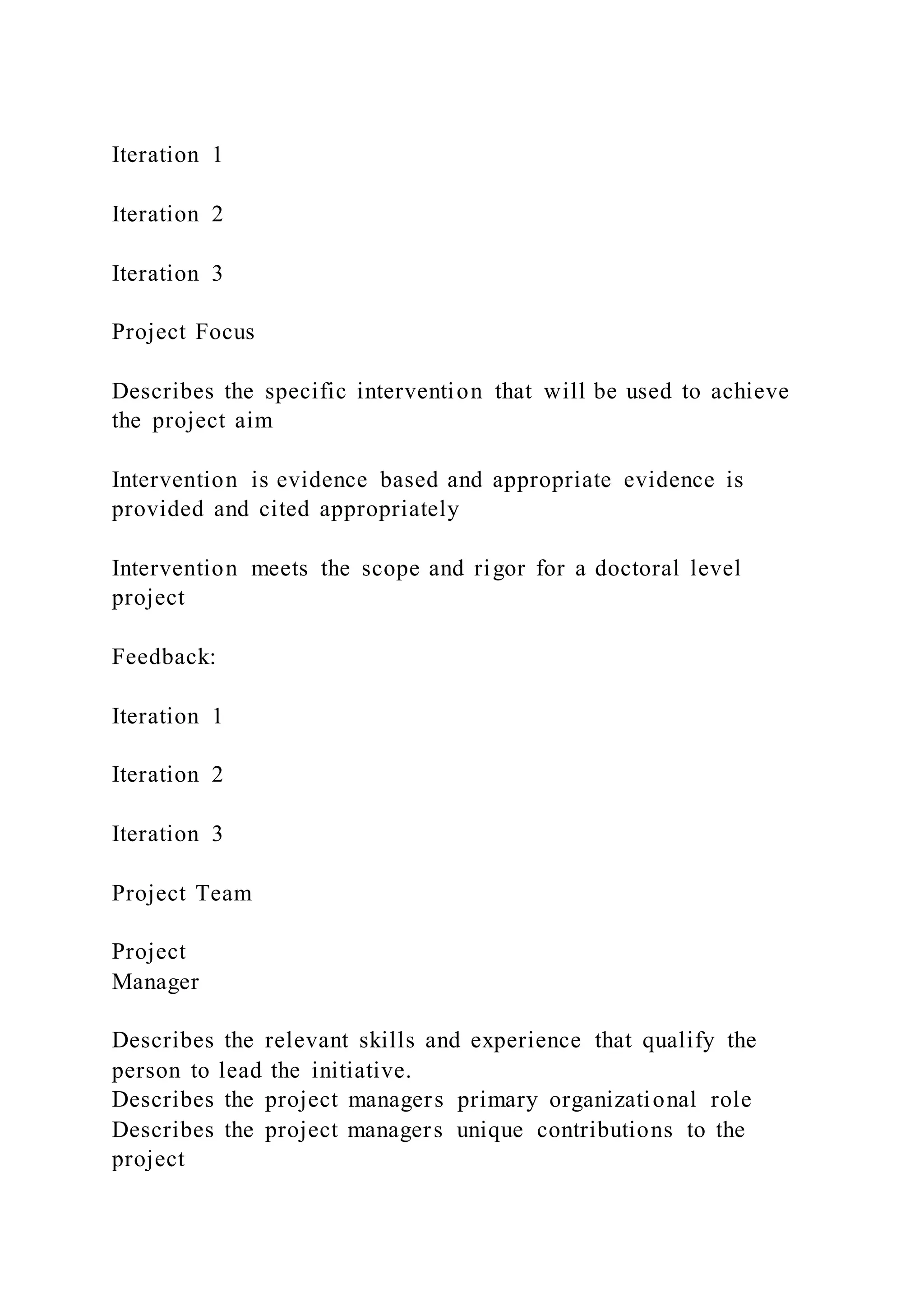
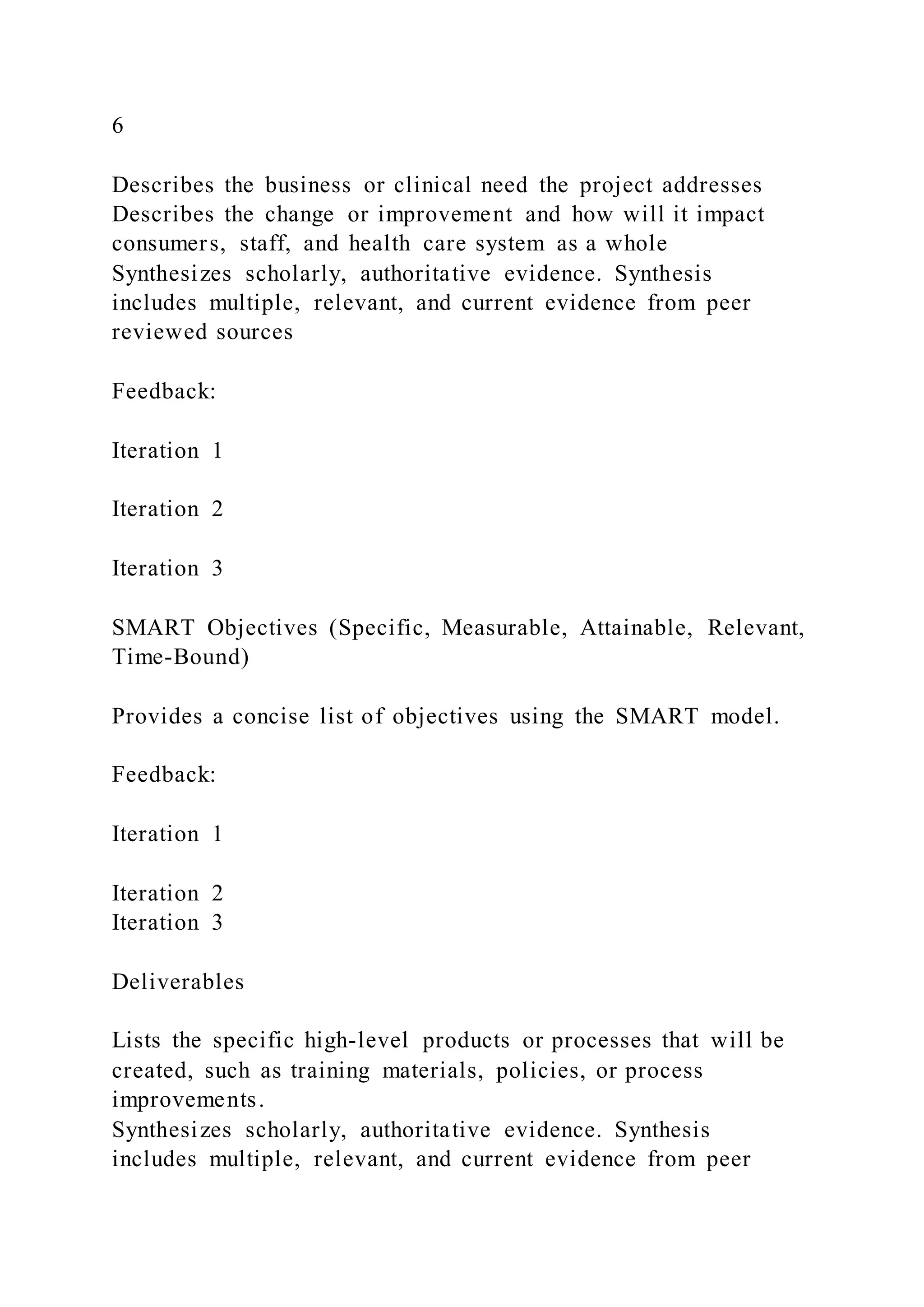
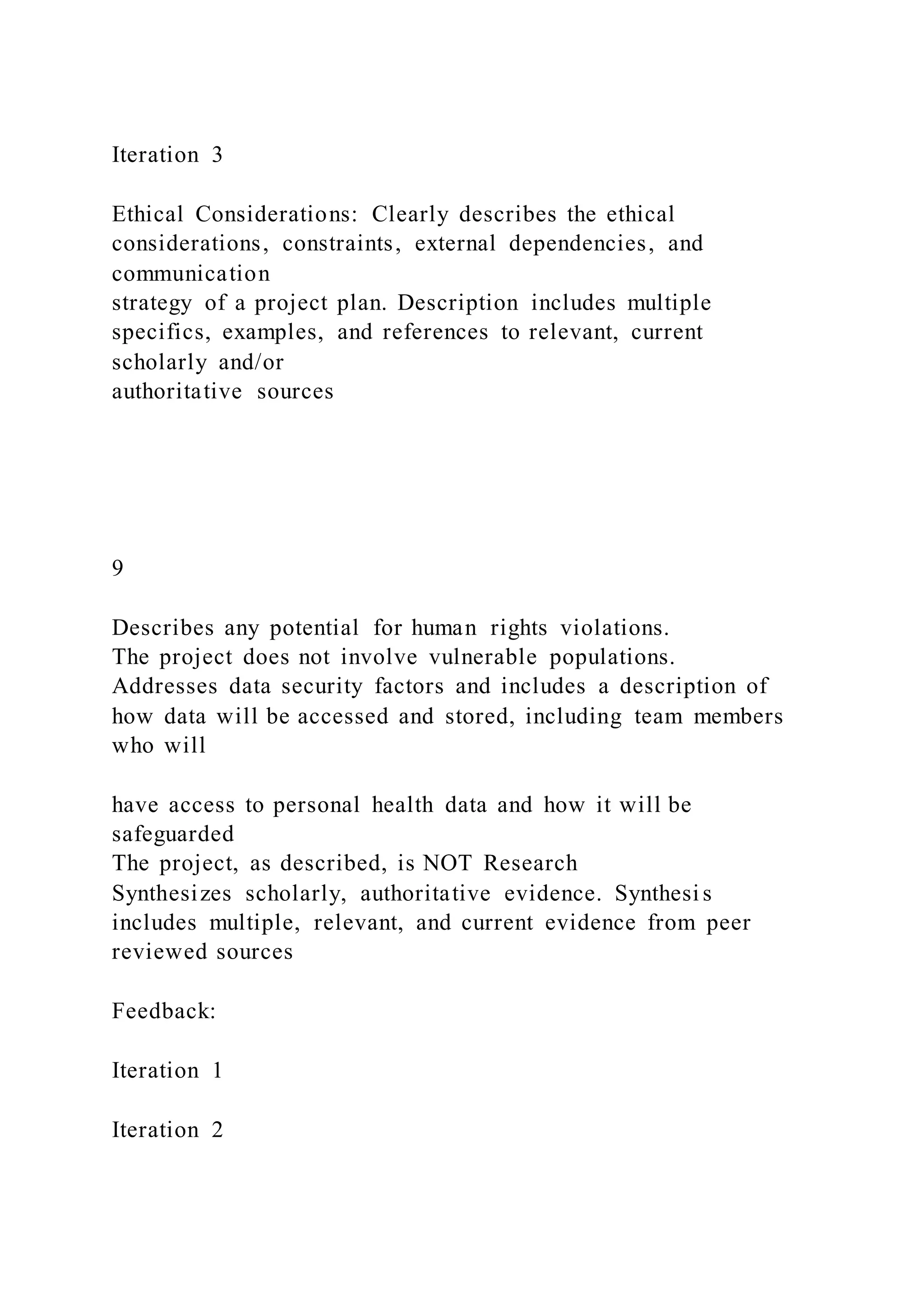
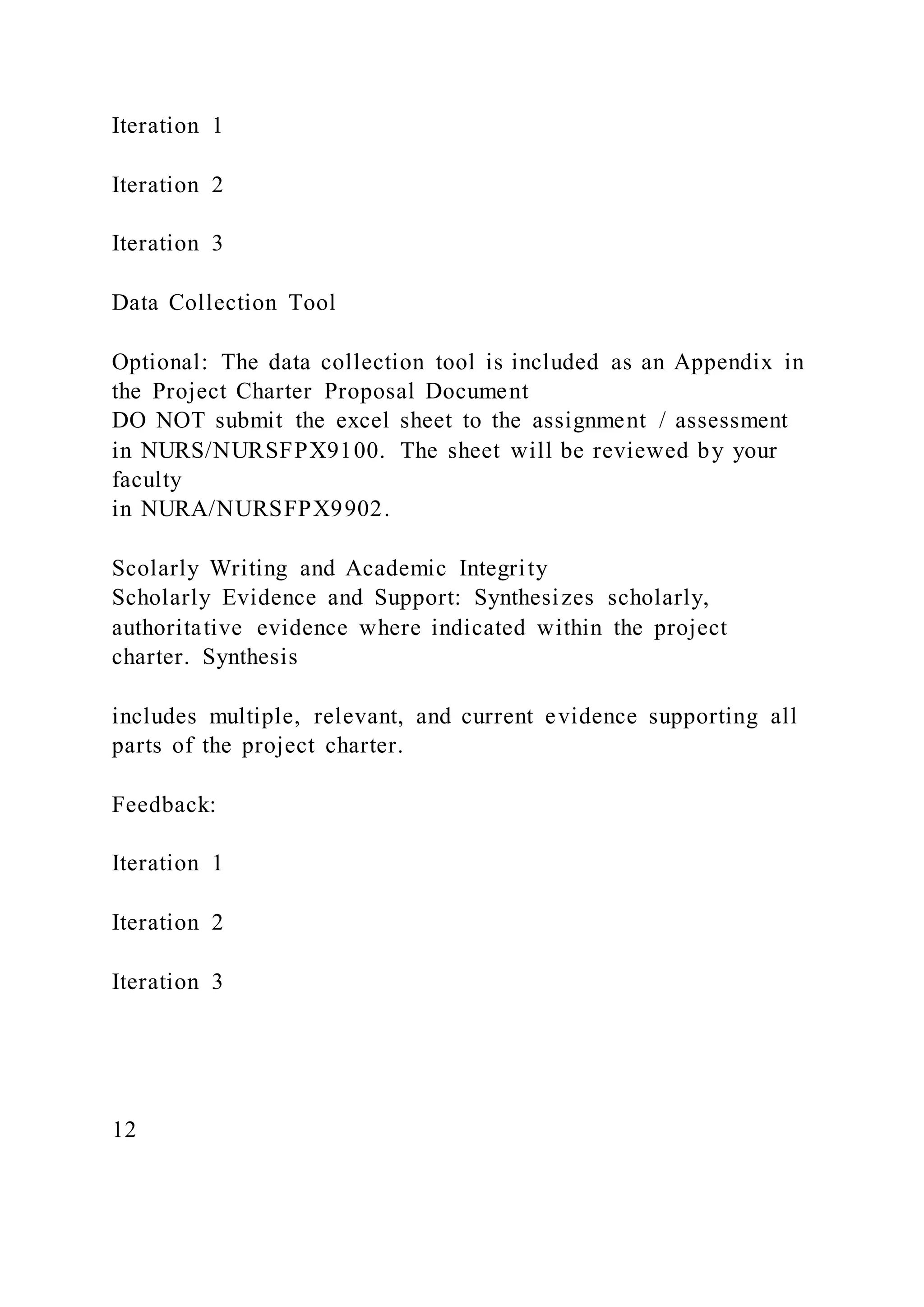
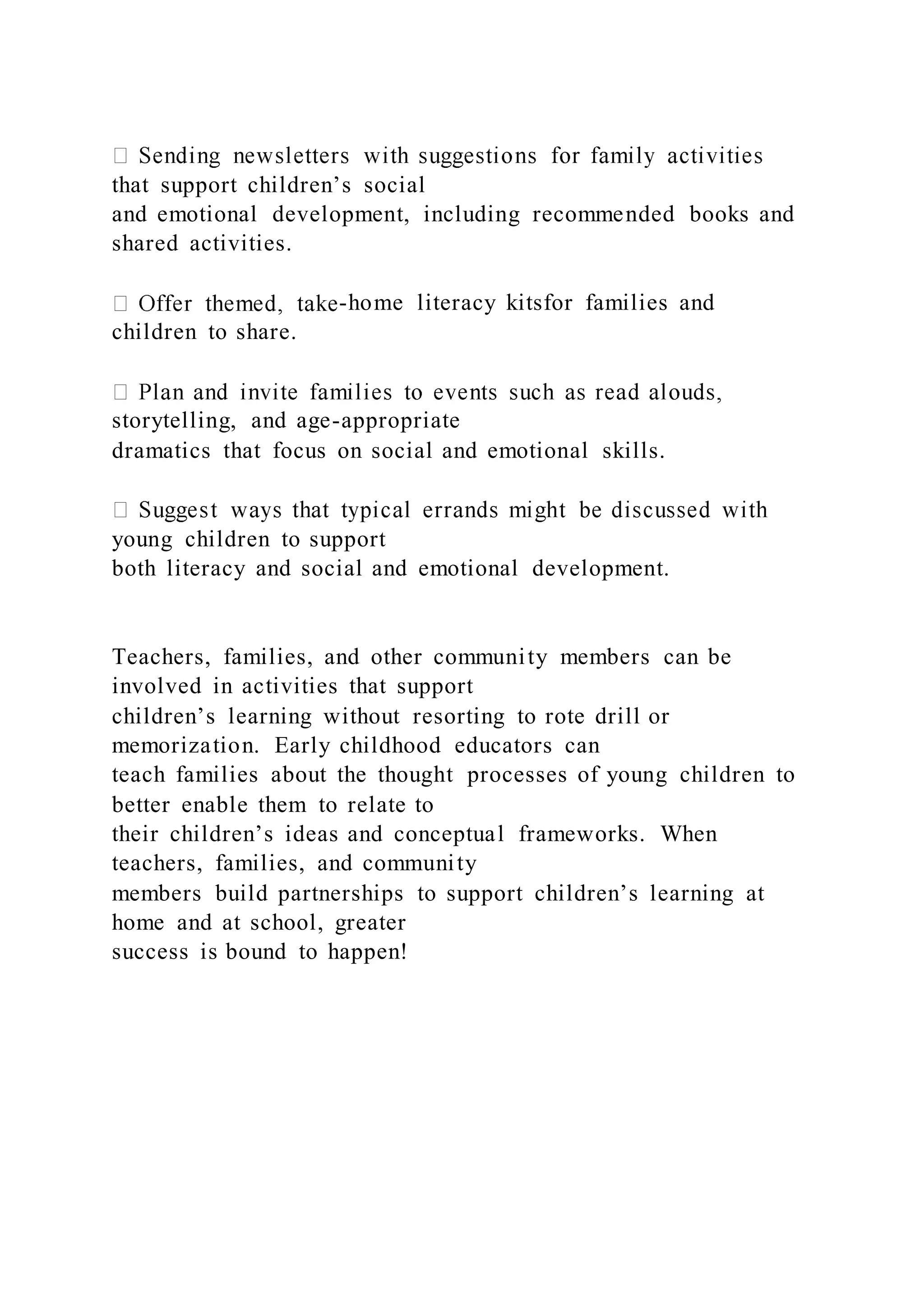
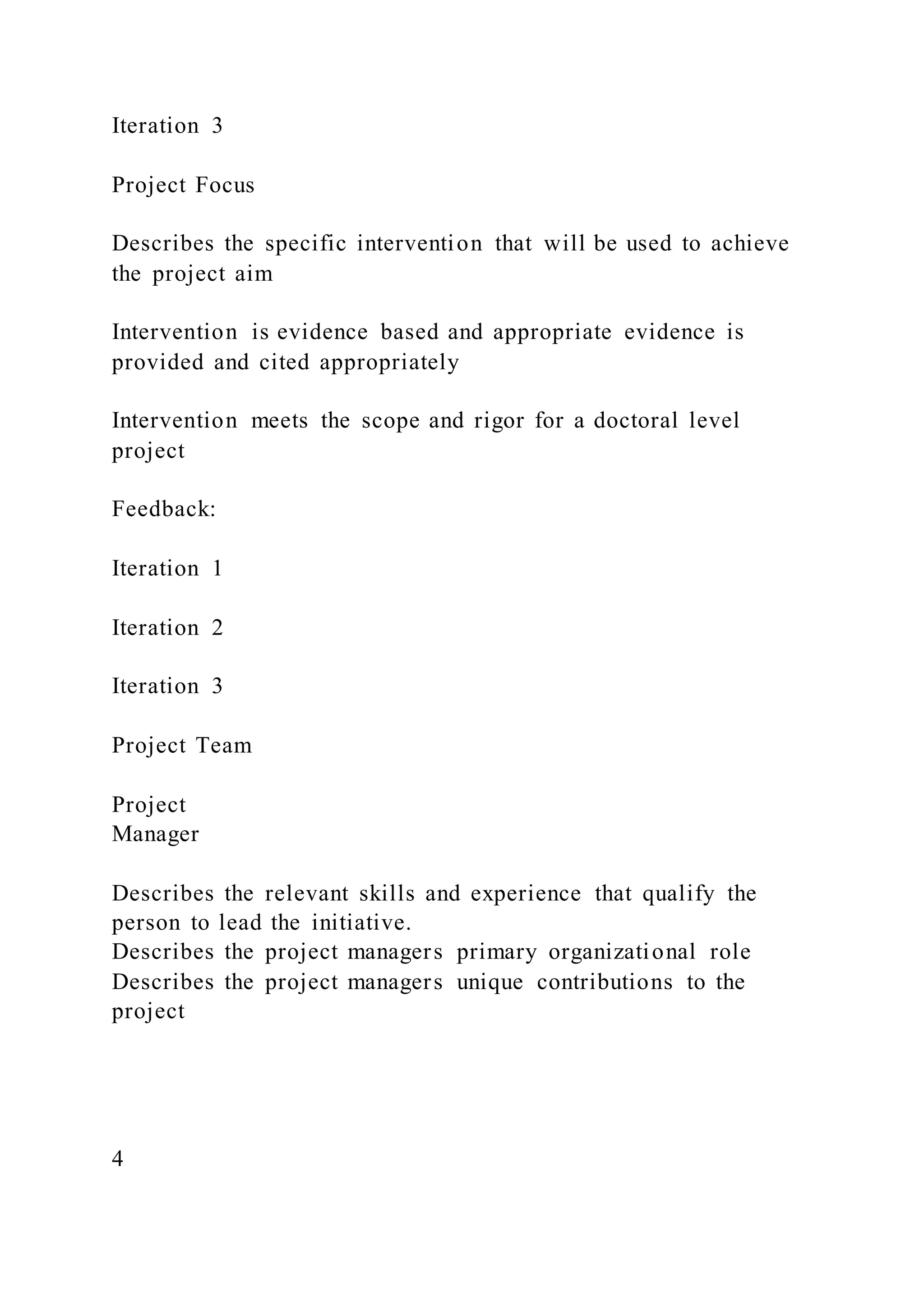
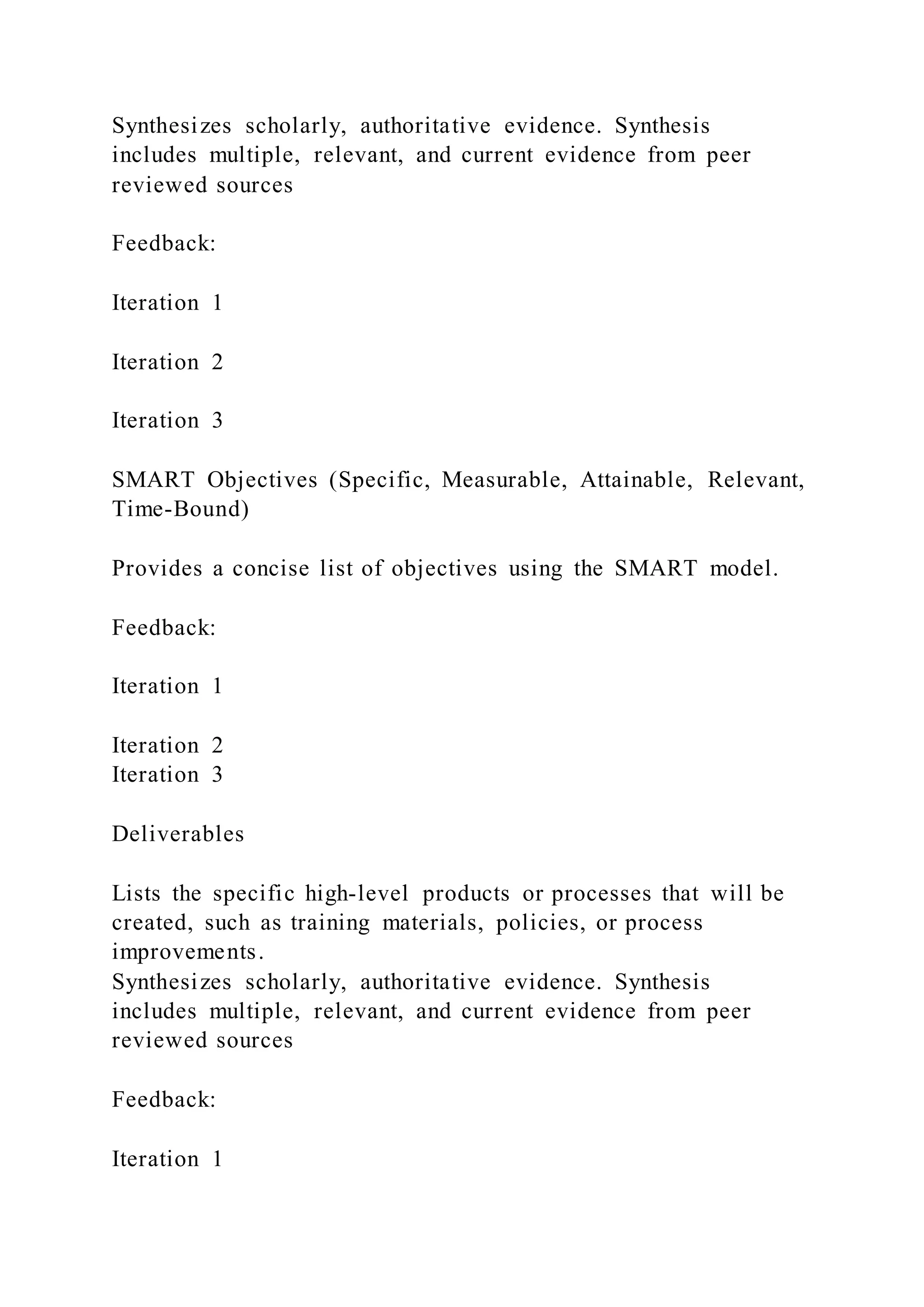
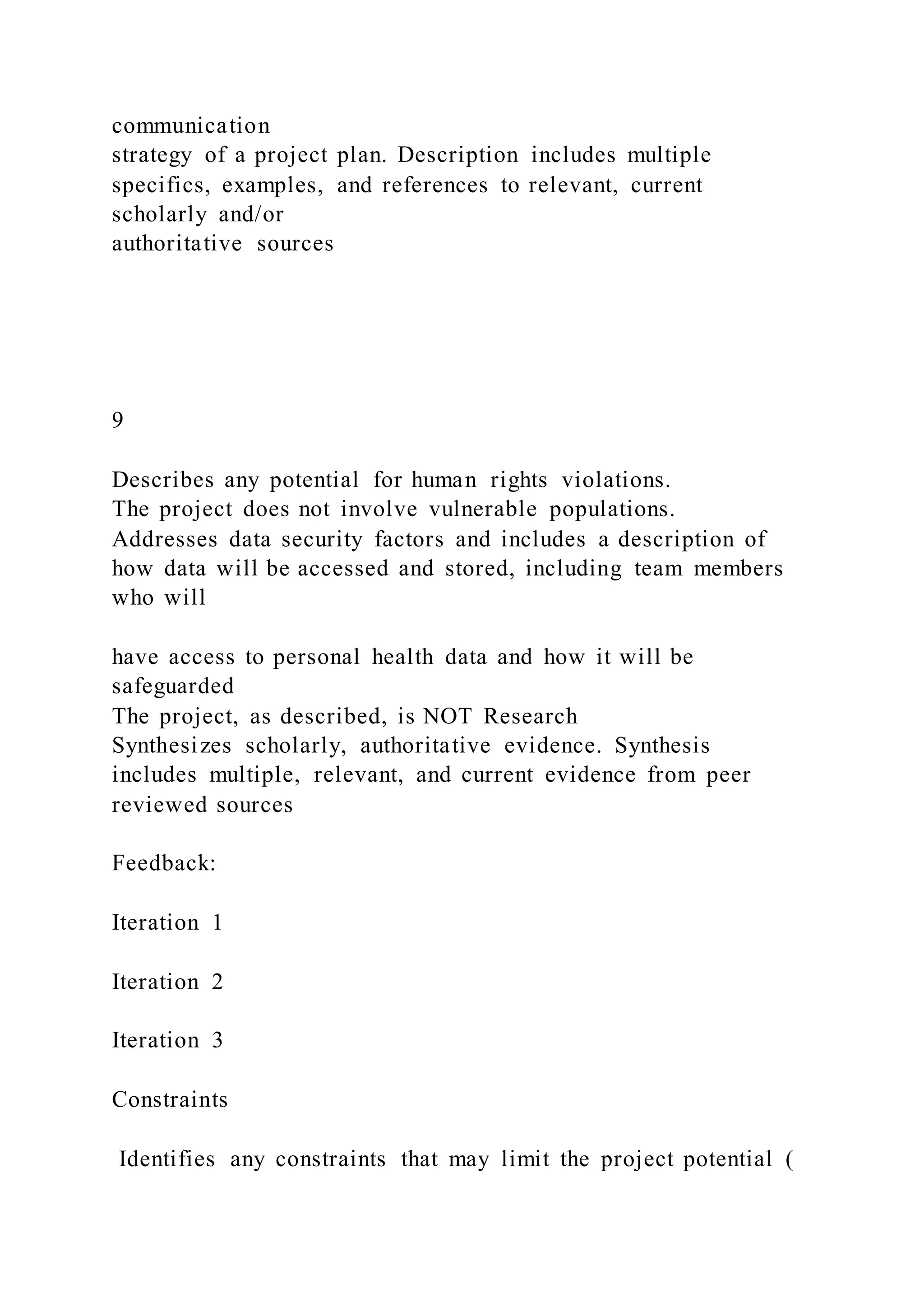
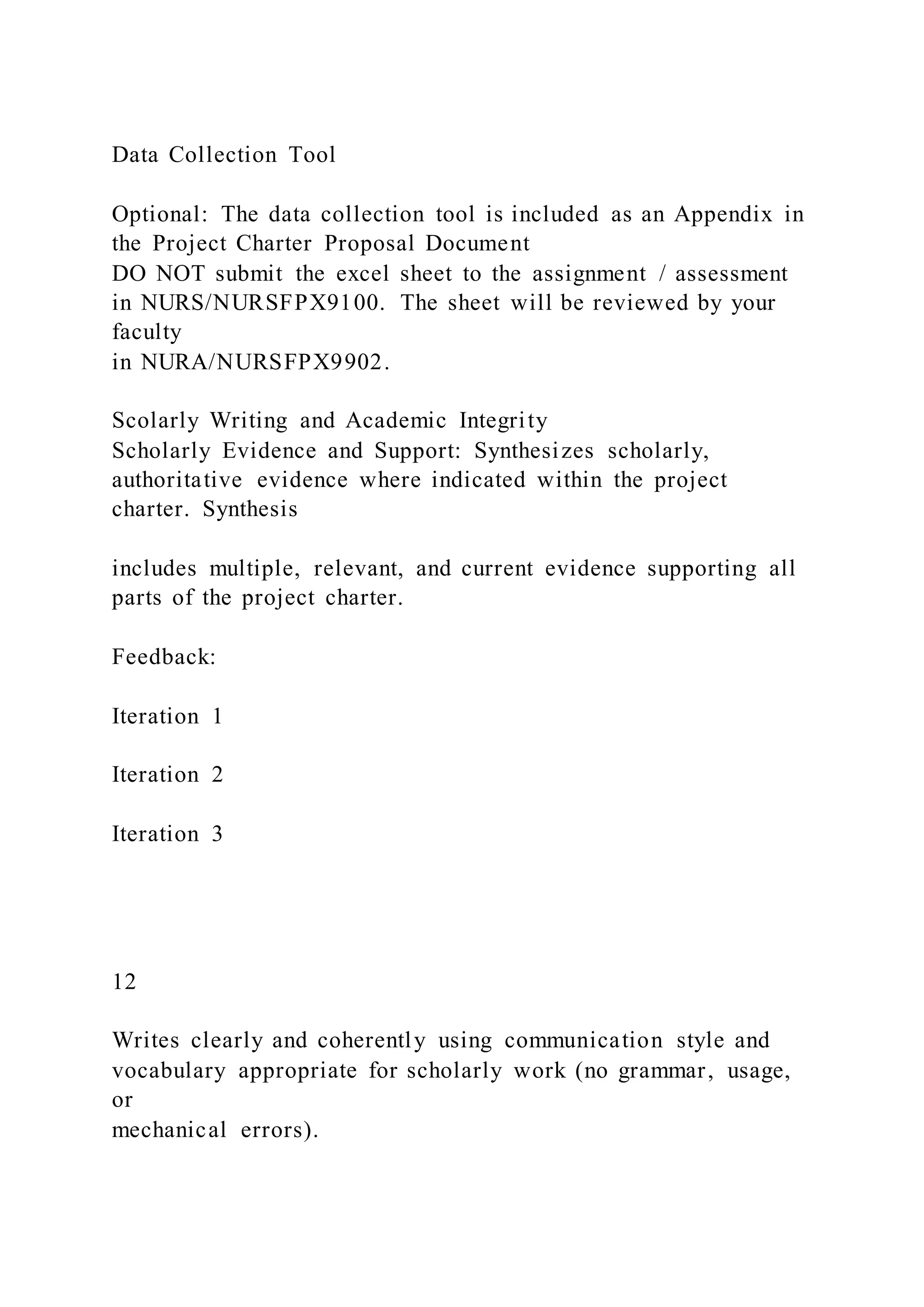
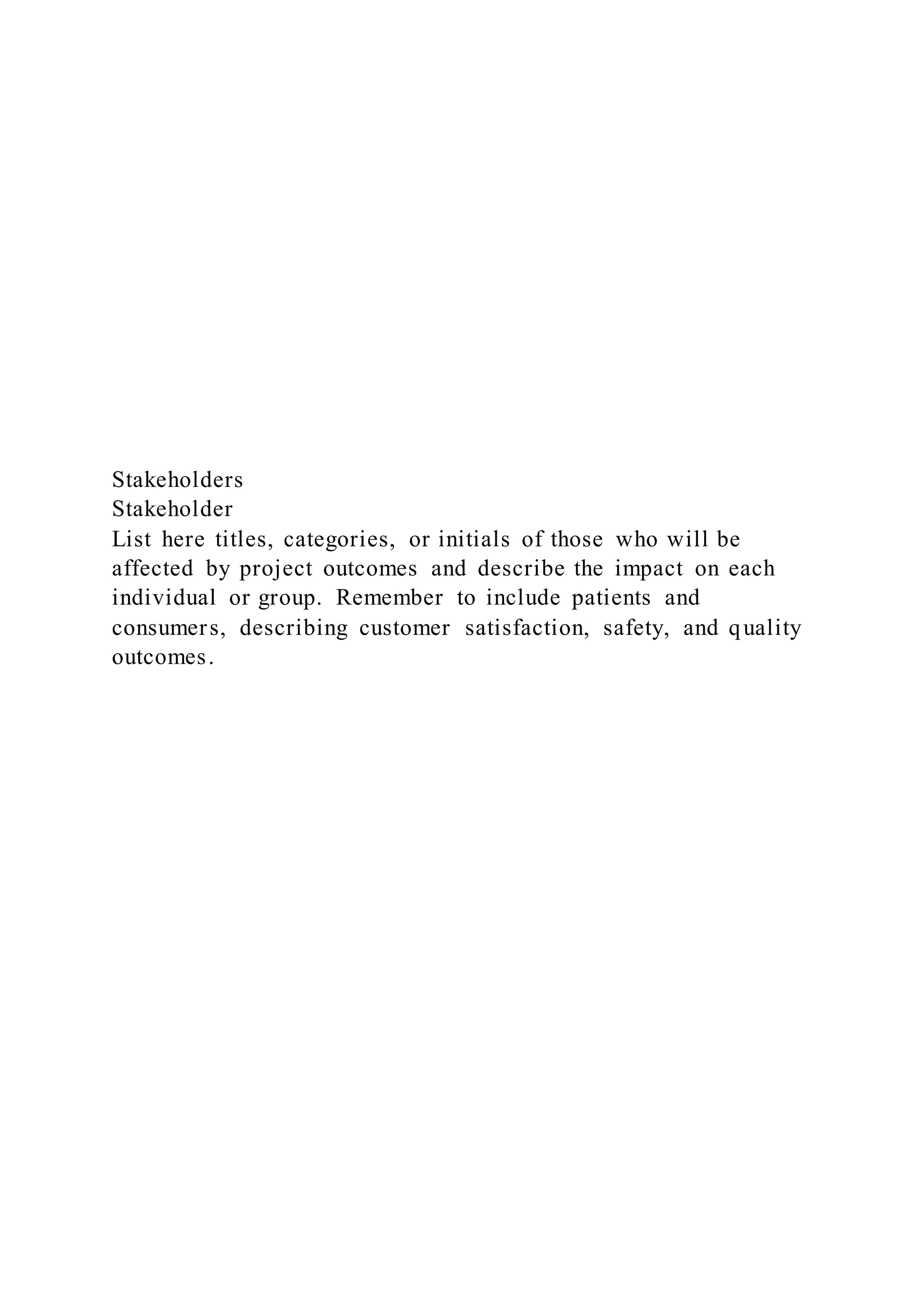
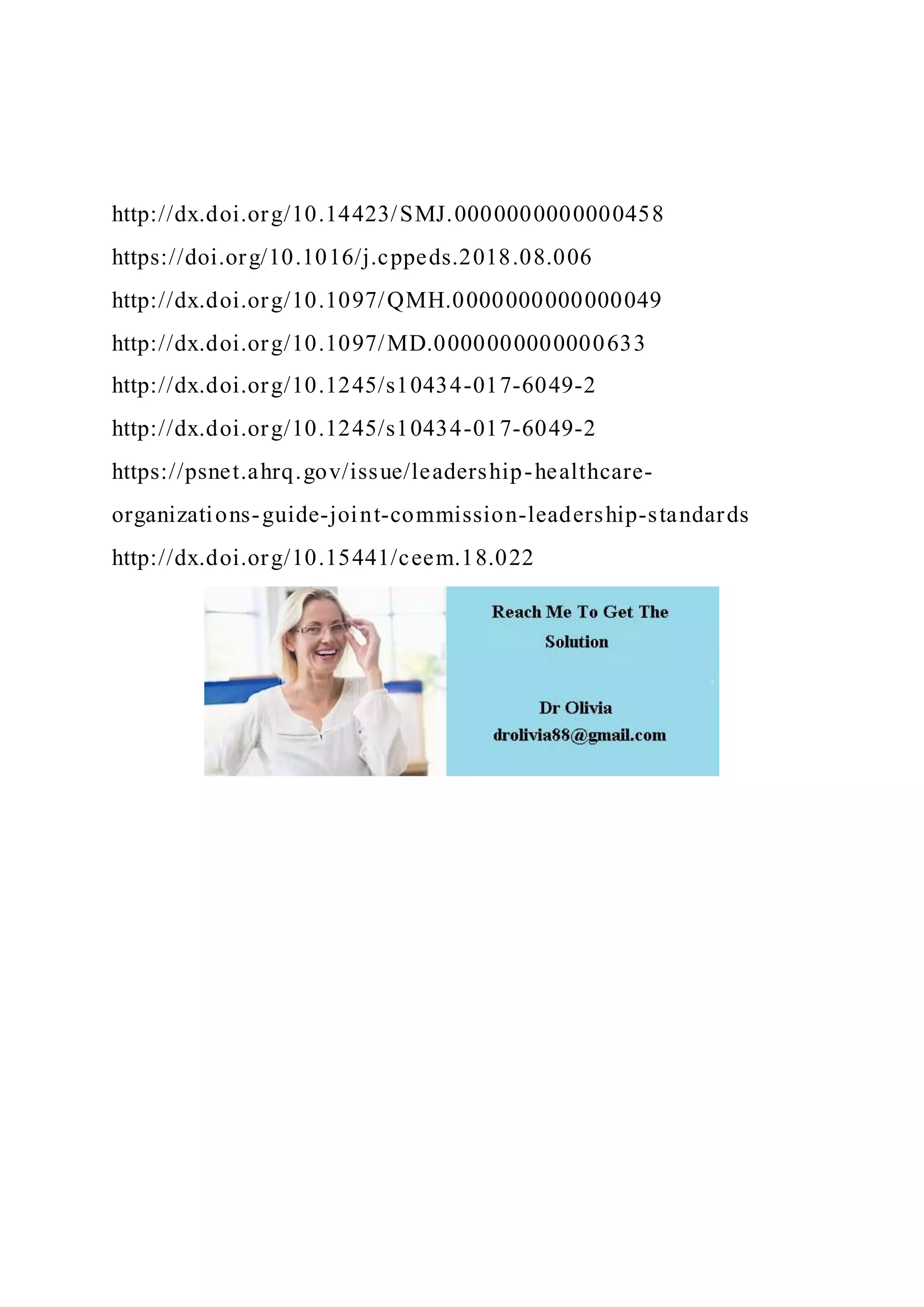
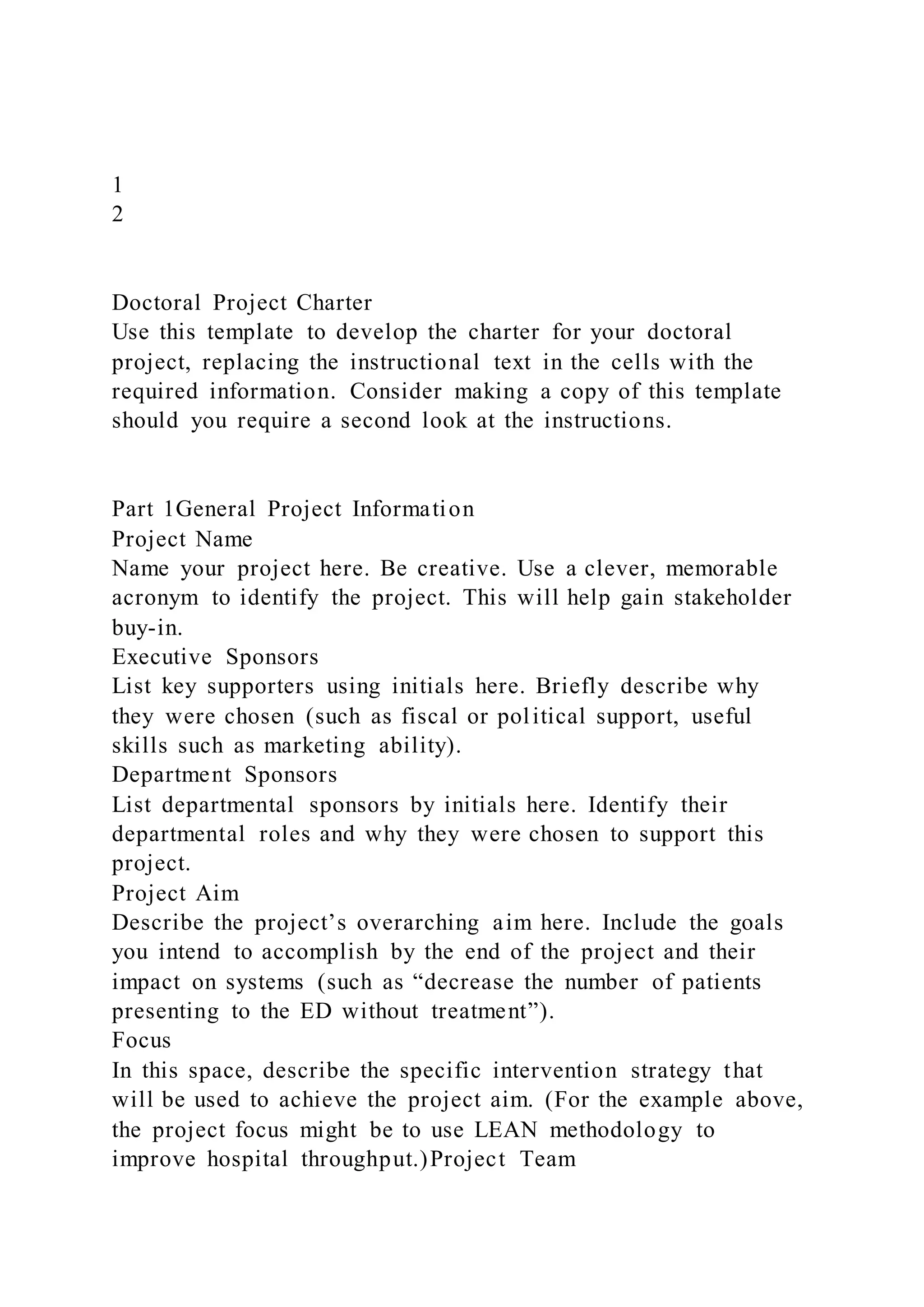
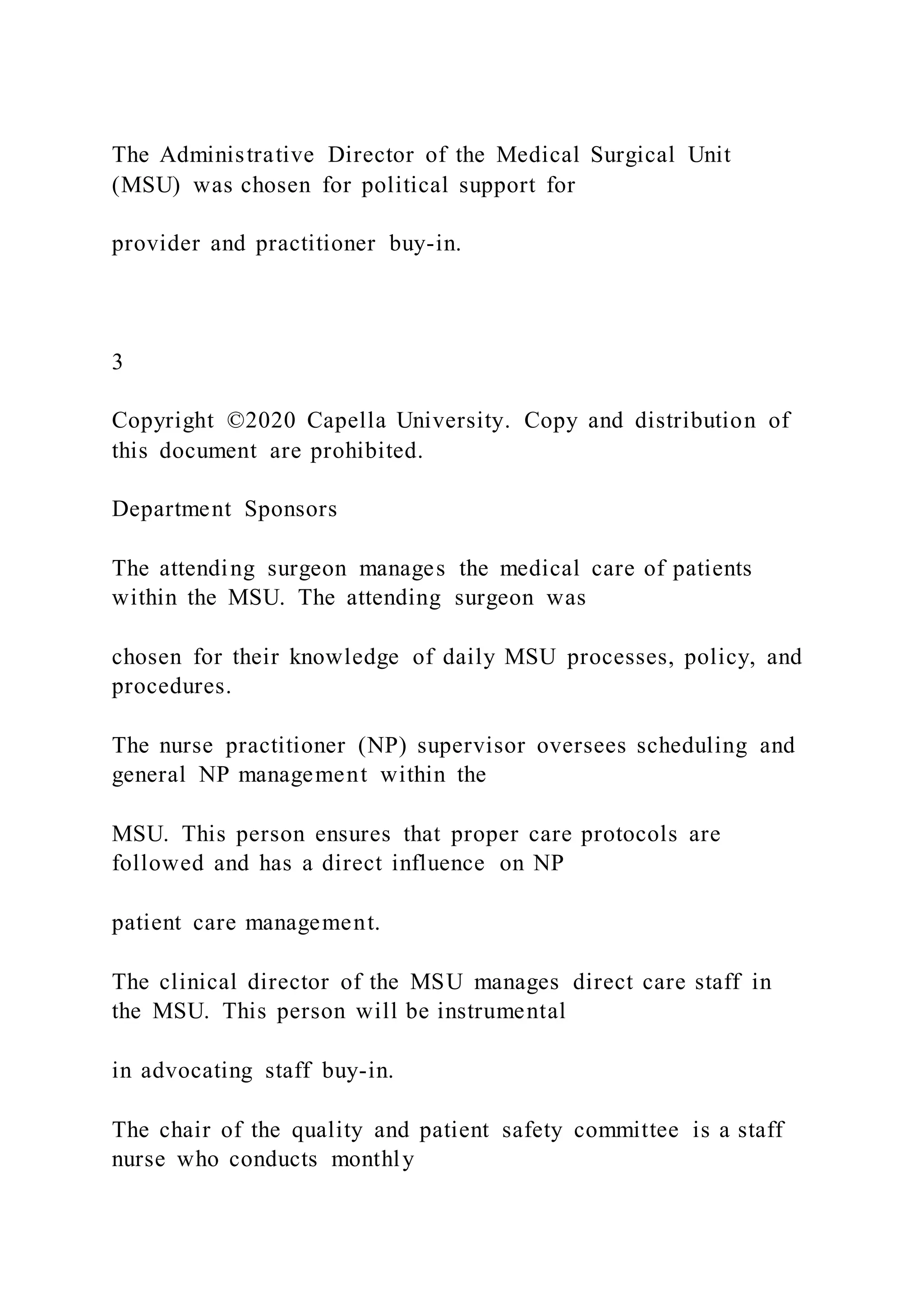
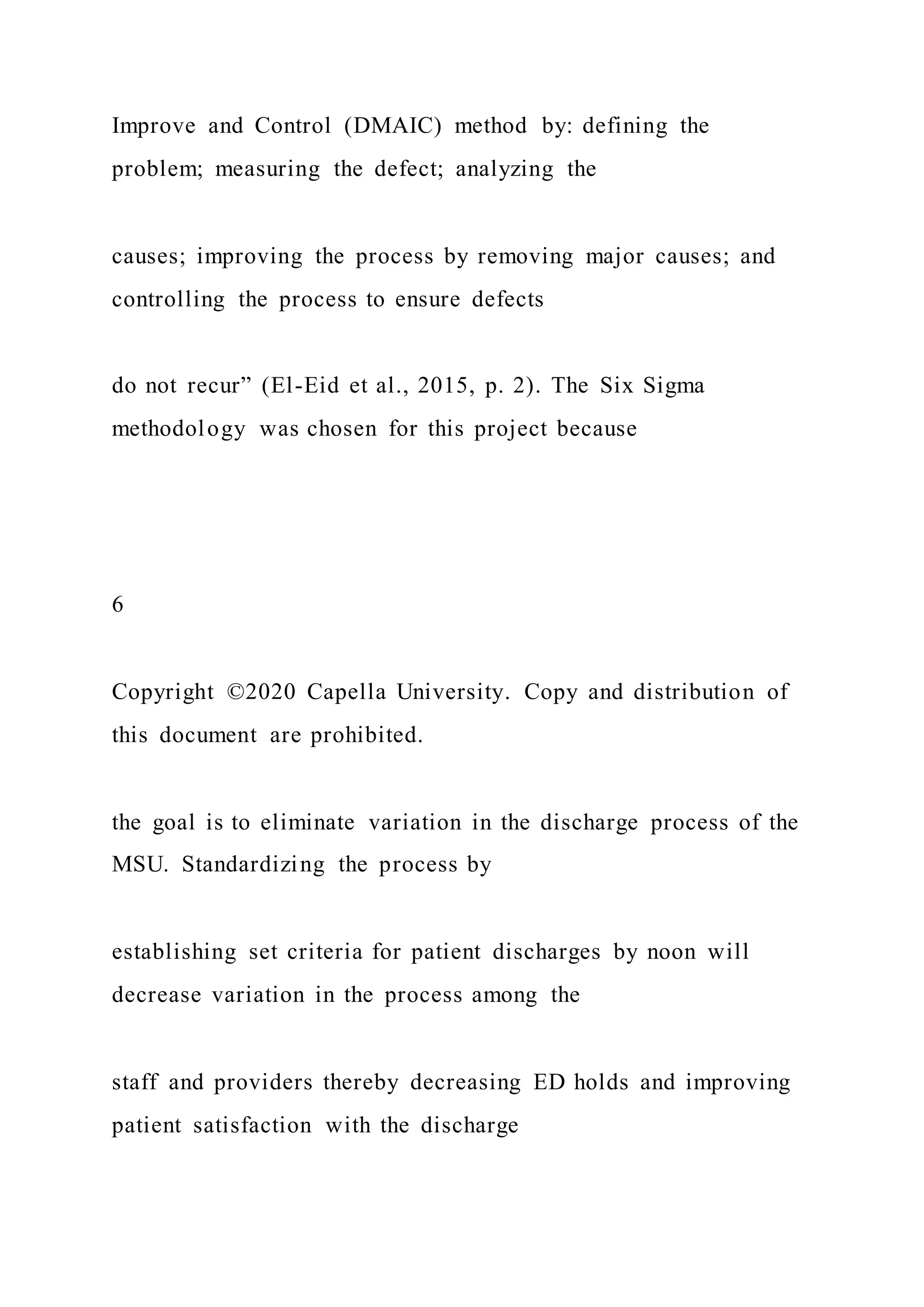
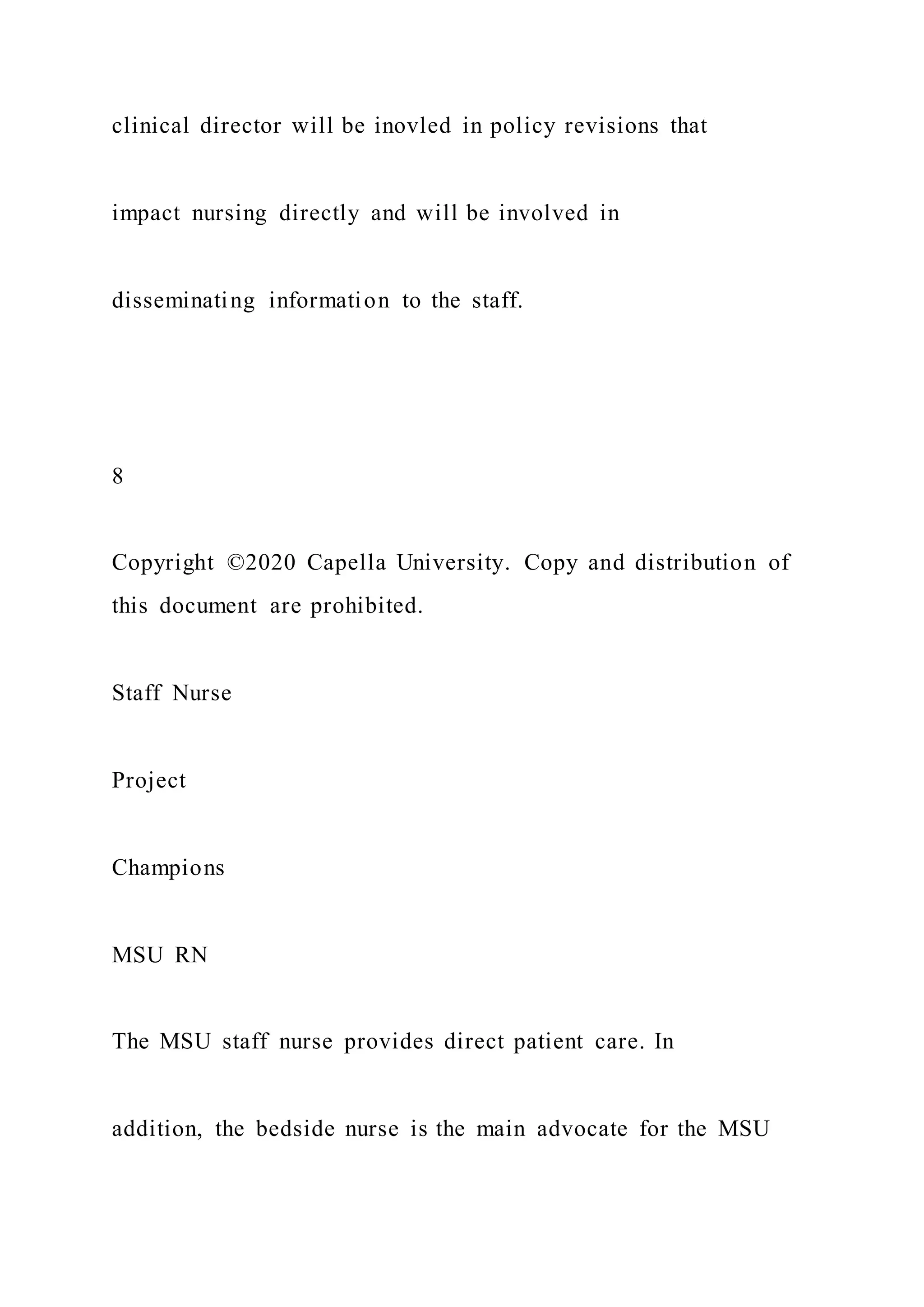
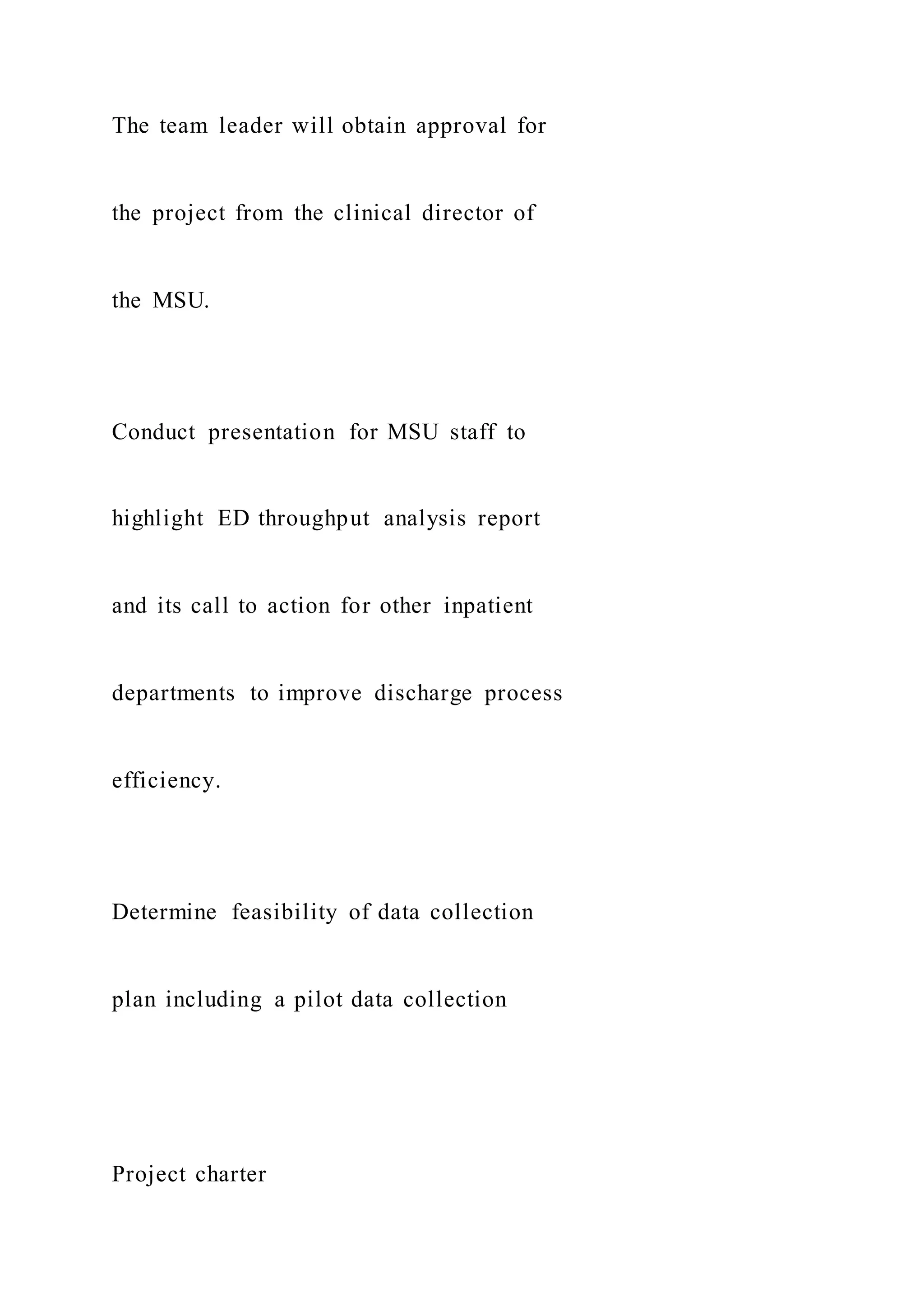
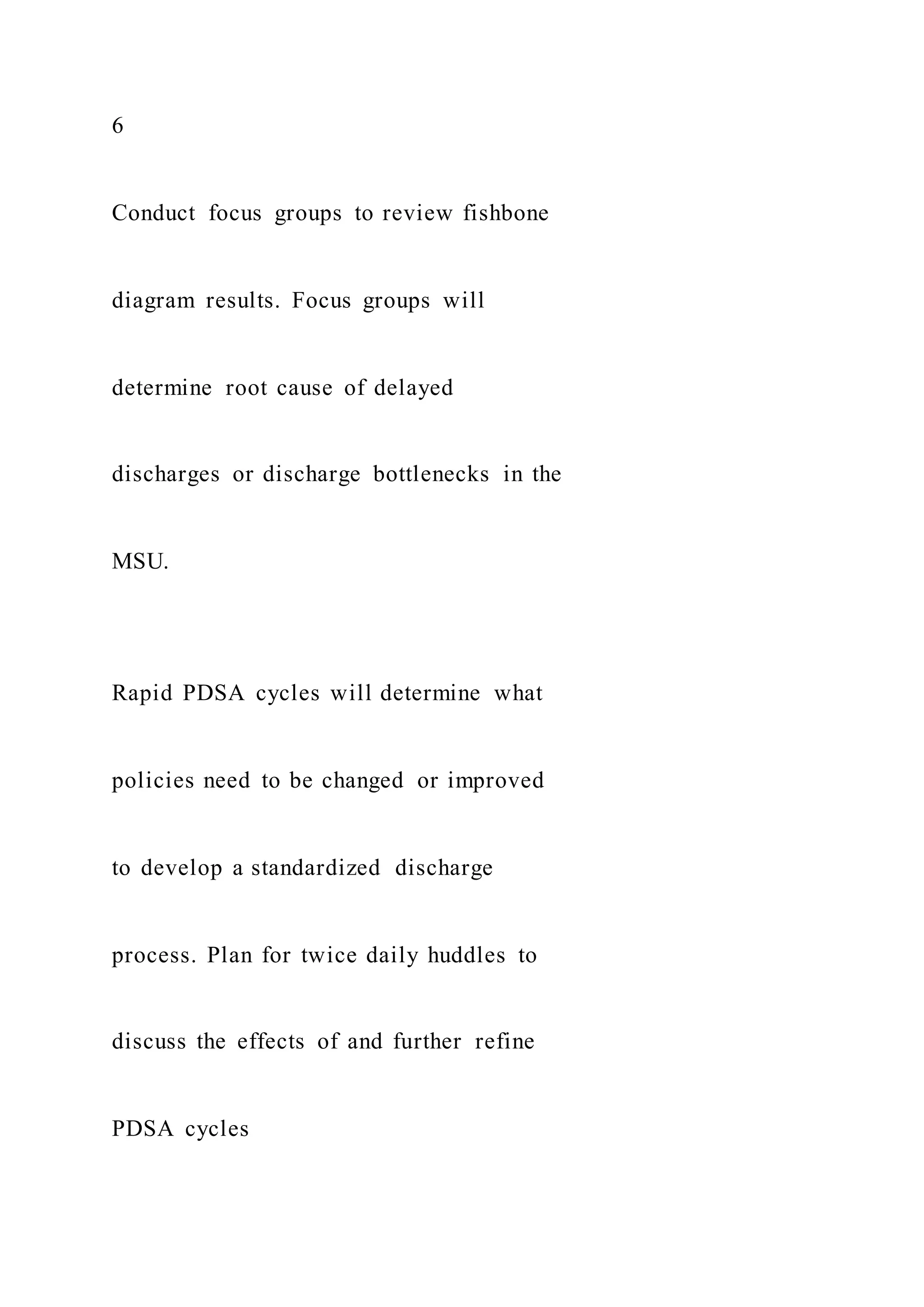
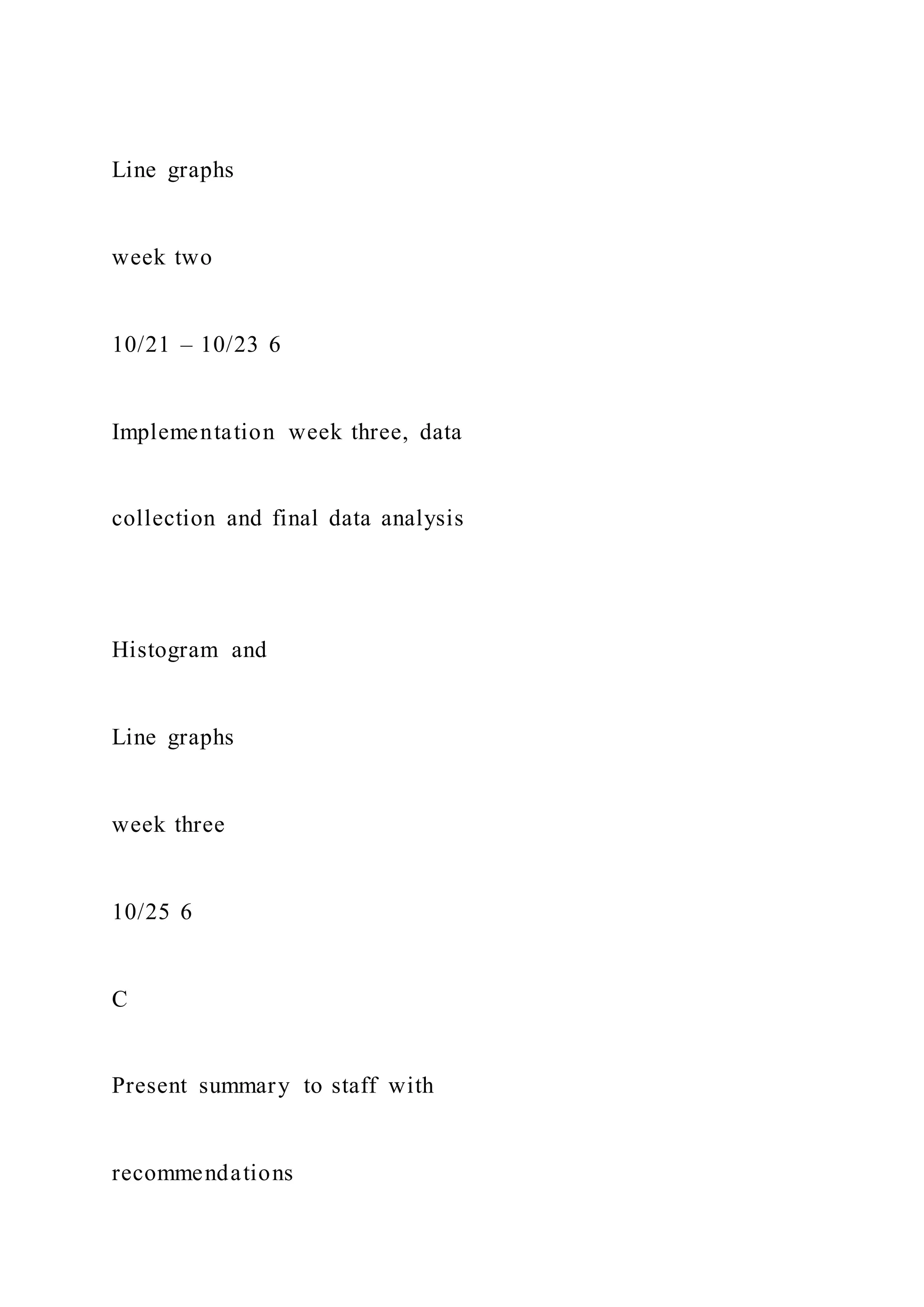
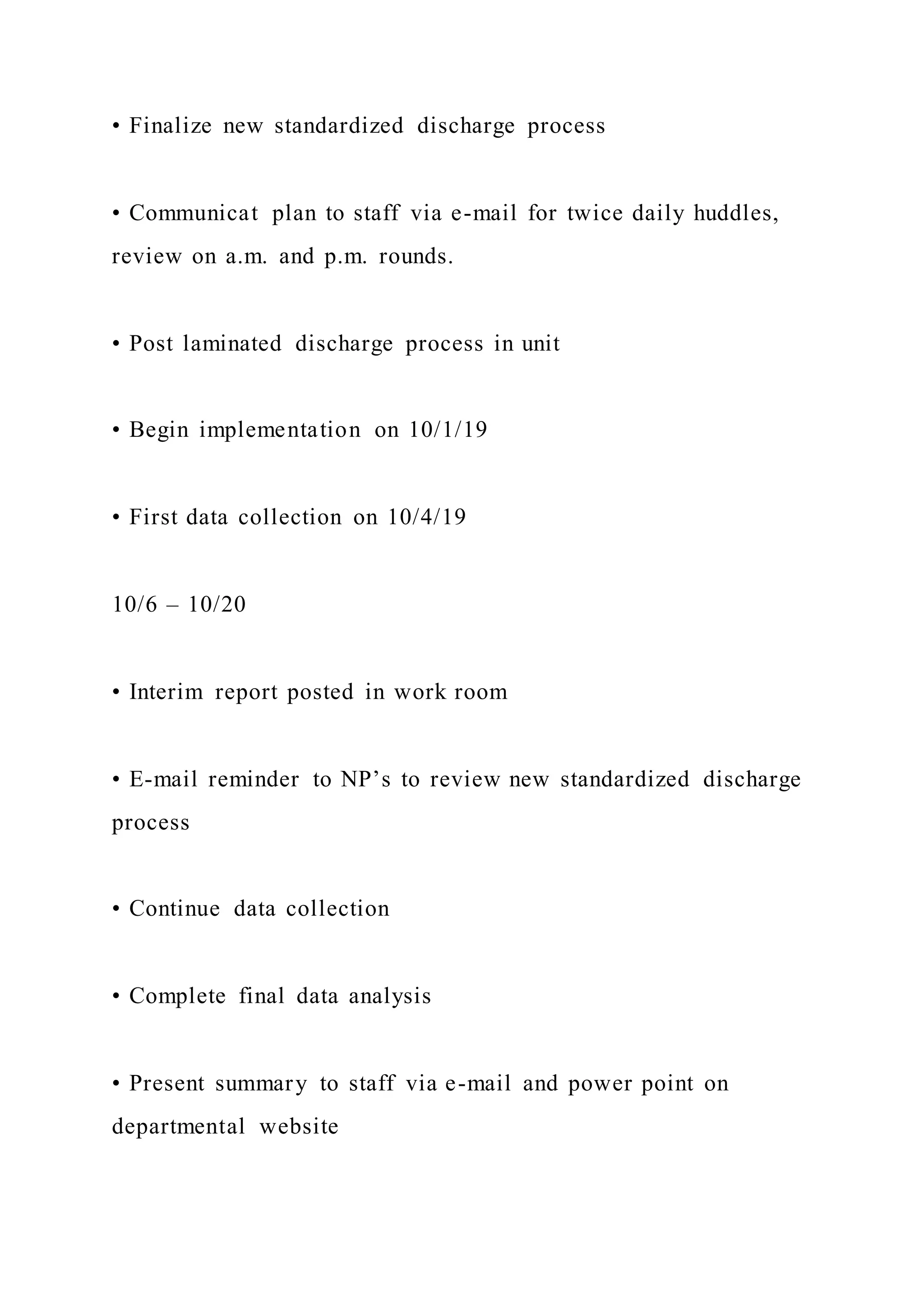
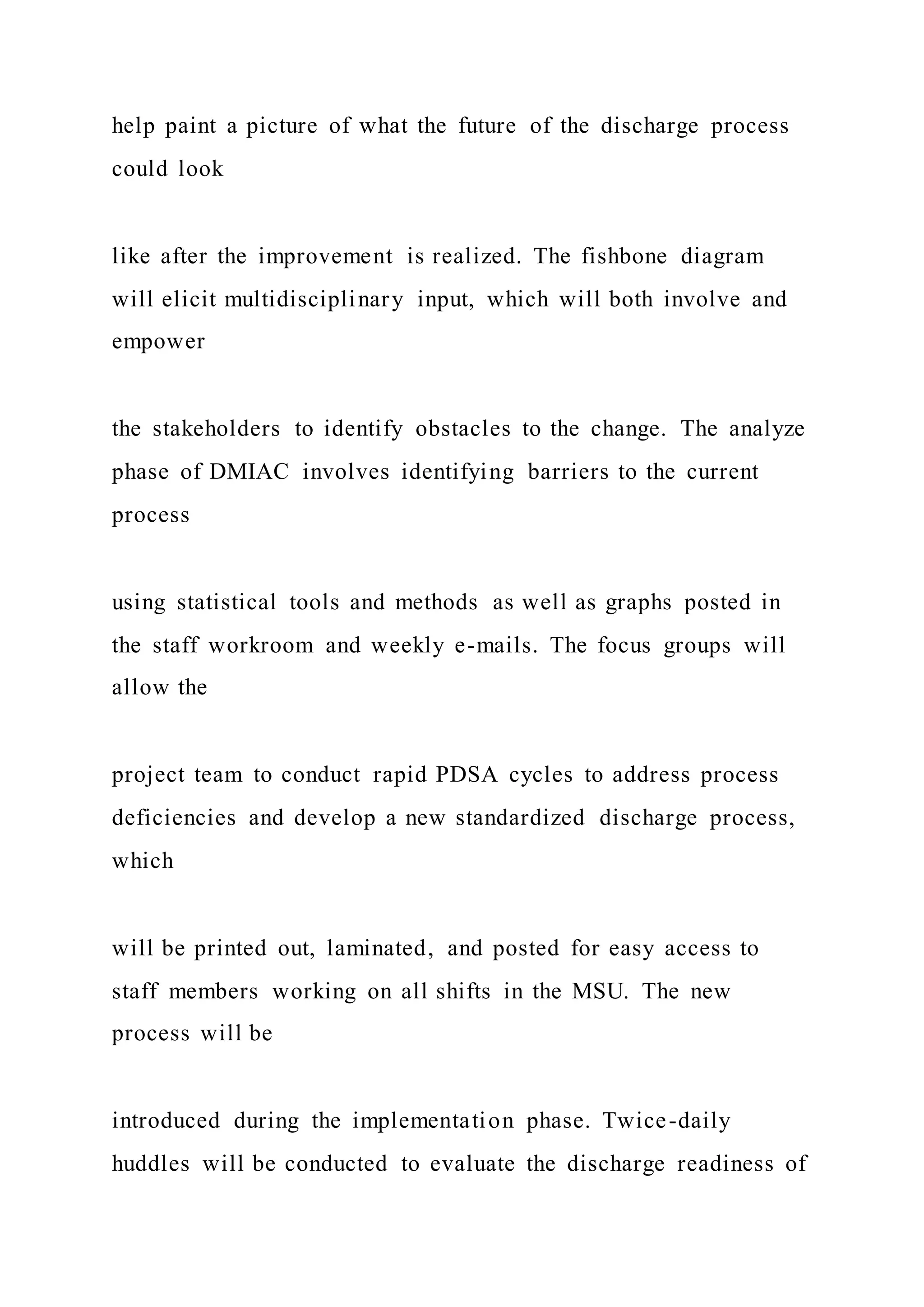
![Ethical Considerations
Taking into account PHI, HIPAA, human subject considerations,
equitable care, and IRB oversight, describe here any potential
for human rights violations. Note any vulnerable populations
involved and plans for equitable subject treatment. Describe
data security factors: how data will be accessed and stored,
including team members who will have access to personal
health data and how it will be safeguarded (such as “Only [X]
people will access the EMR”).
Constraints
List here any limits to personnel, funding, scheduling, or other
options, such as a predetermined budget, limited staff, or
deadline.
External Dependencies
If the project’s success may depend on external relationships or
resources such as personnel, funding, communication channels,
or community resources, describe them here. If there are no
external dependencies, describe internal support.
Communication Strategy
Indicate here how the project manager will communicate to
sponsors, project team, and stakeholders. Describe the means
and frequency of communication, including meetings,
processes, and tools such as charts, wikis, and dashboards.
Proposed Outcomes
Metric](https://image.slidesharecdn.com/1doctoralprojectcharterproposalchecklistinstruct-220920053858-baf1555b/75/1-Doctoral-Project-Charter-Proposal-Checklist-Instruct-47-2048.jpg)
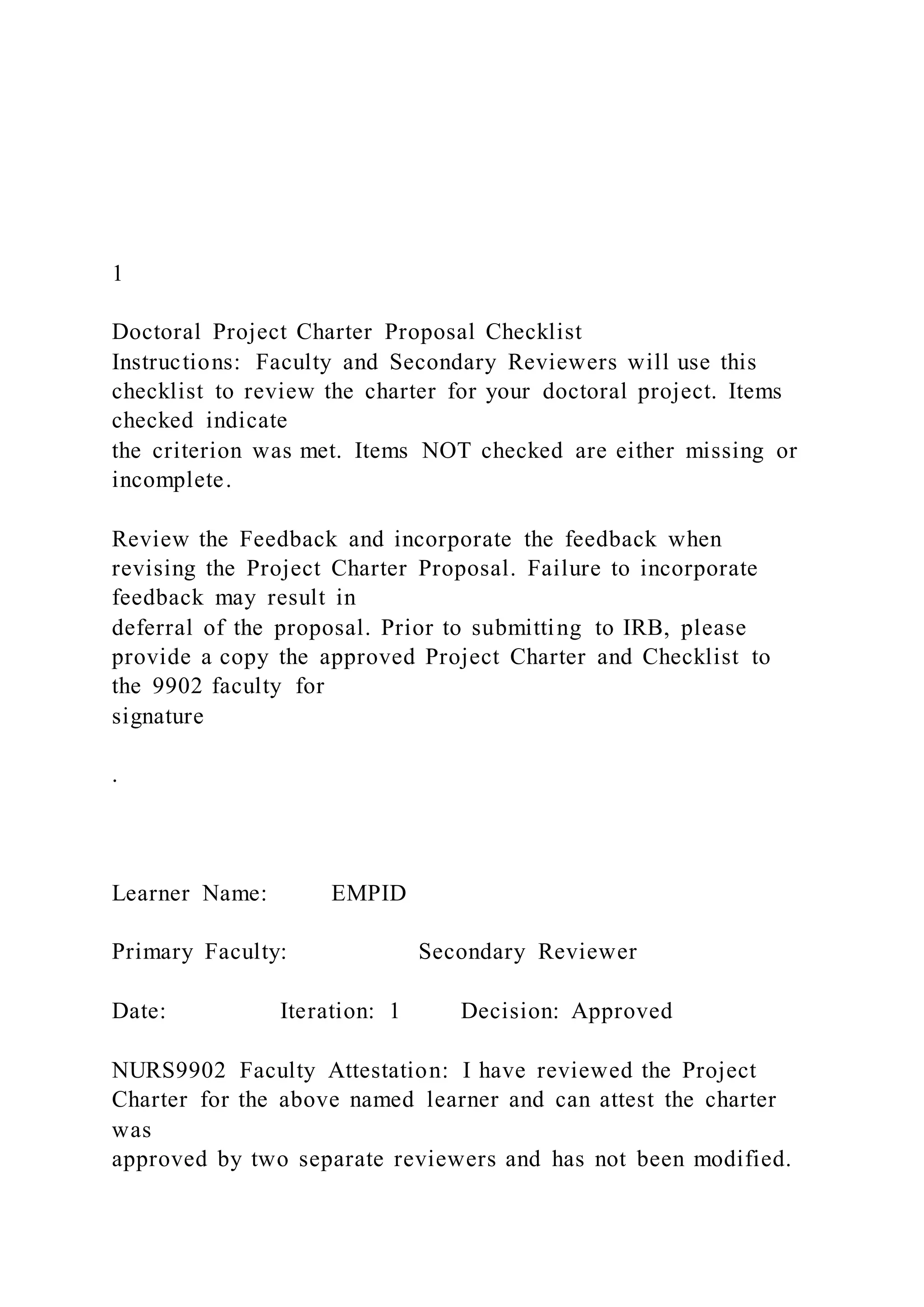
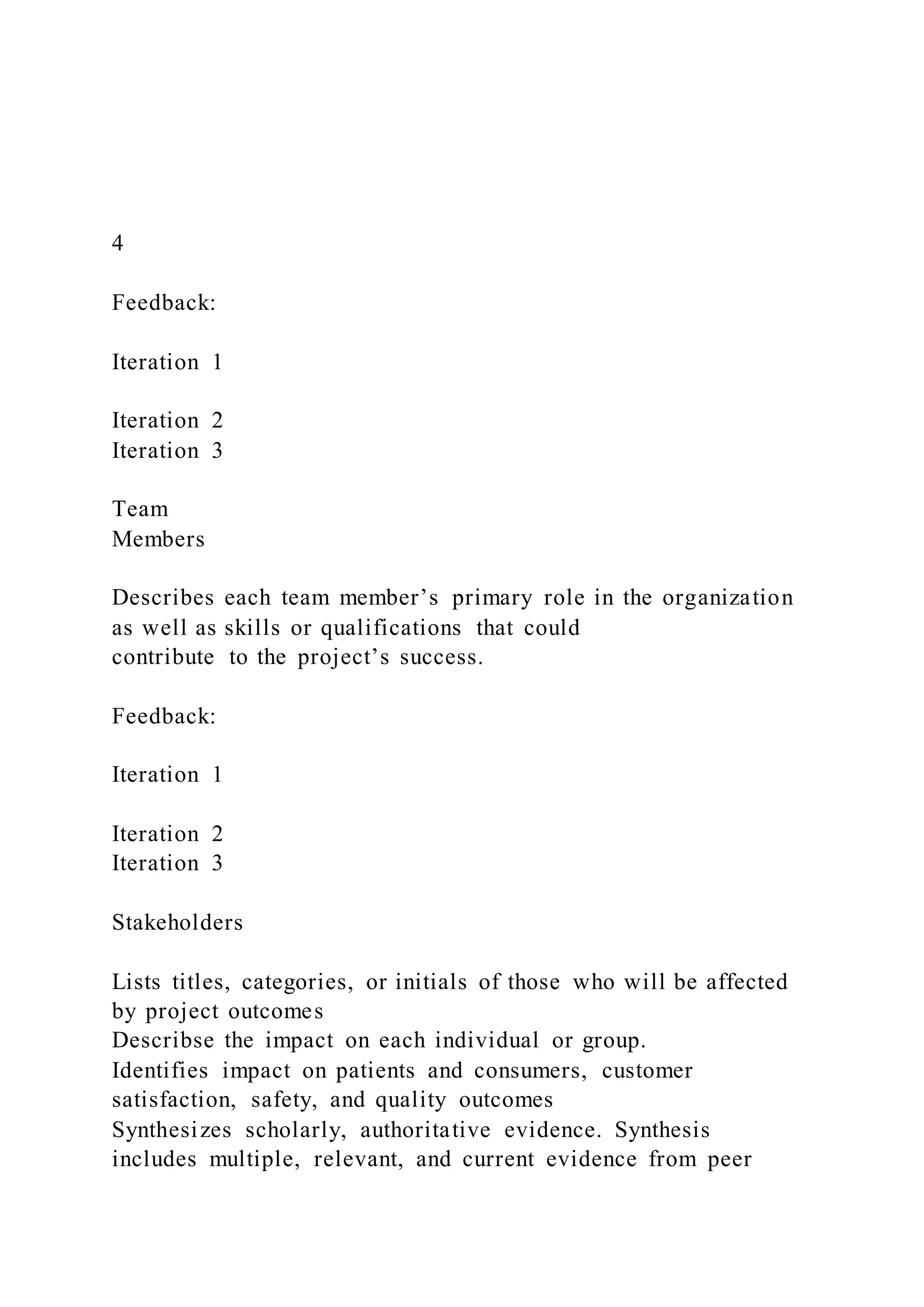
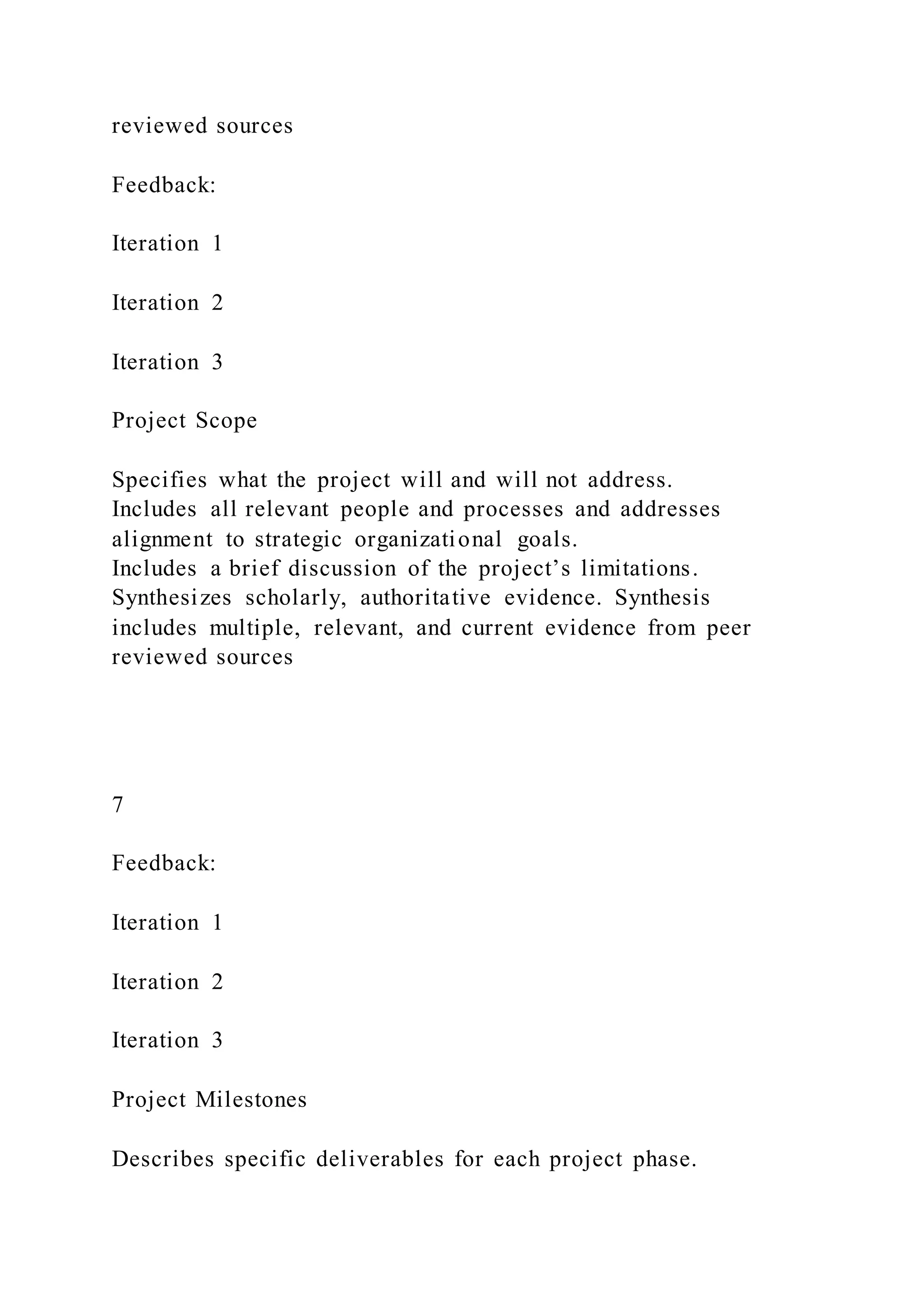
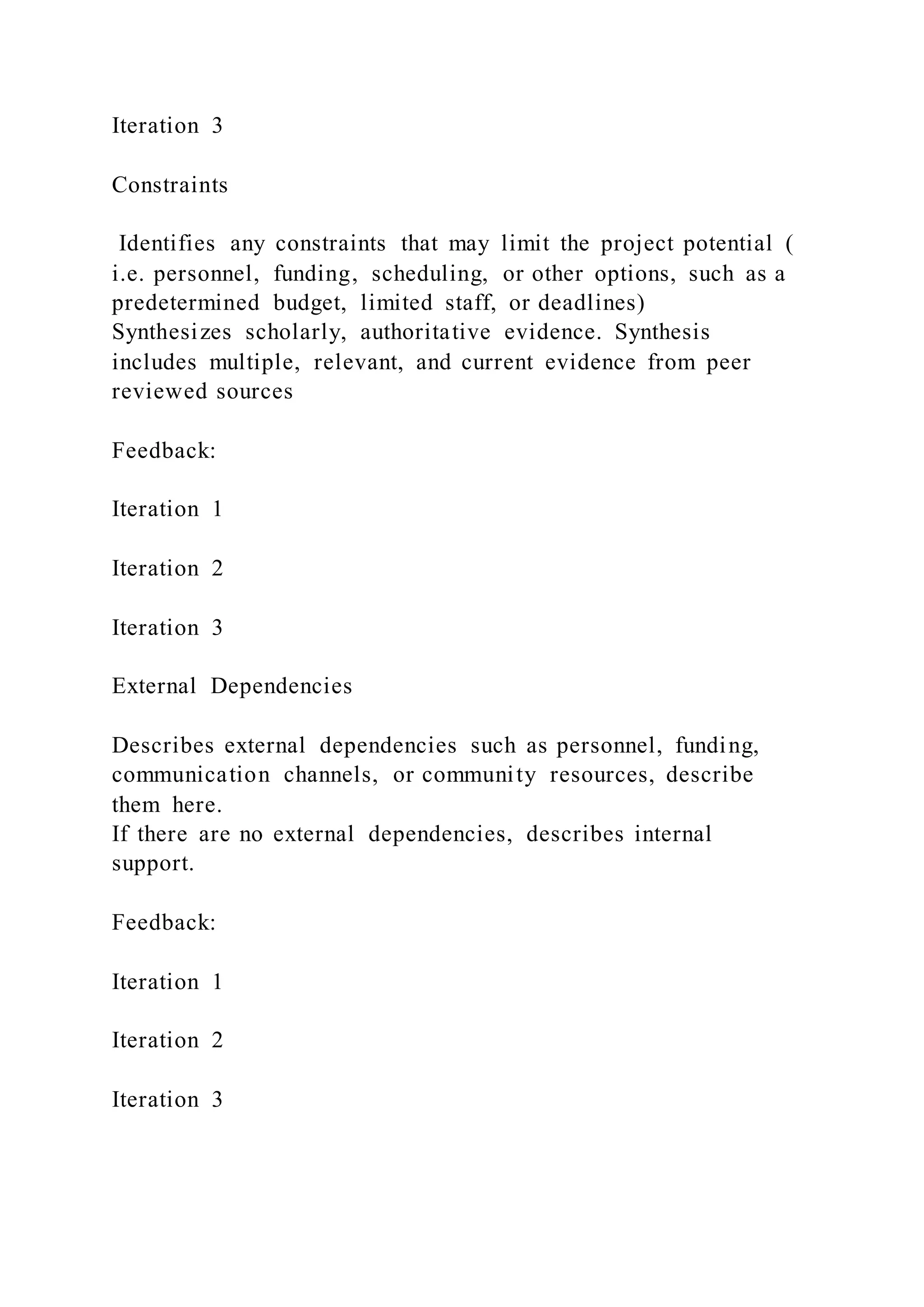
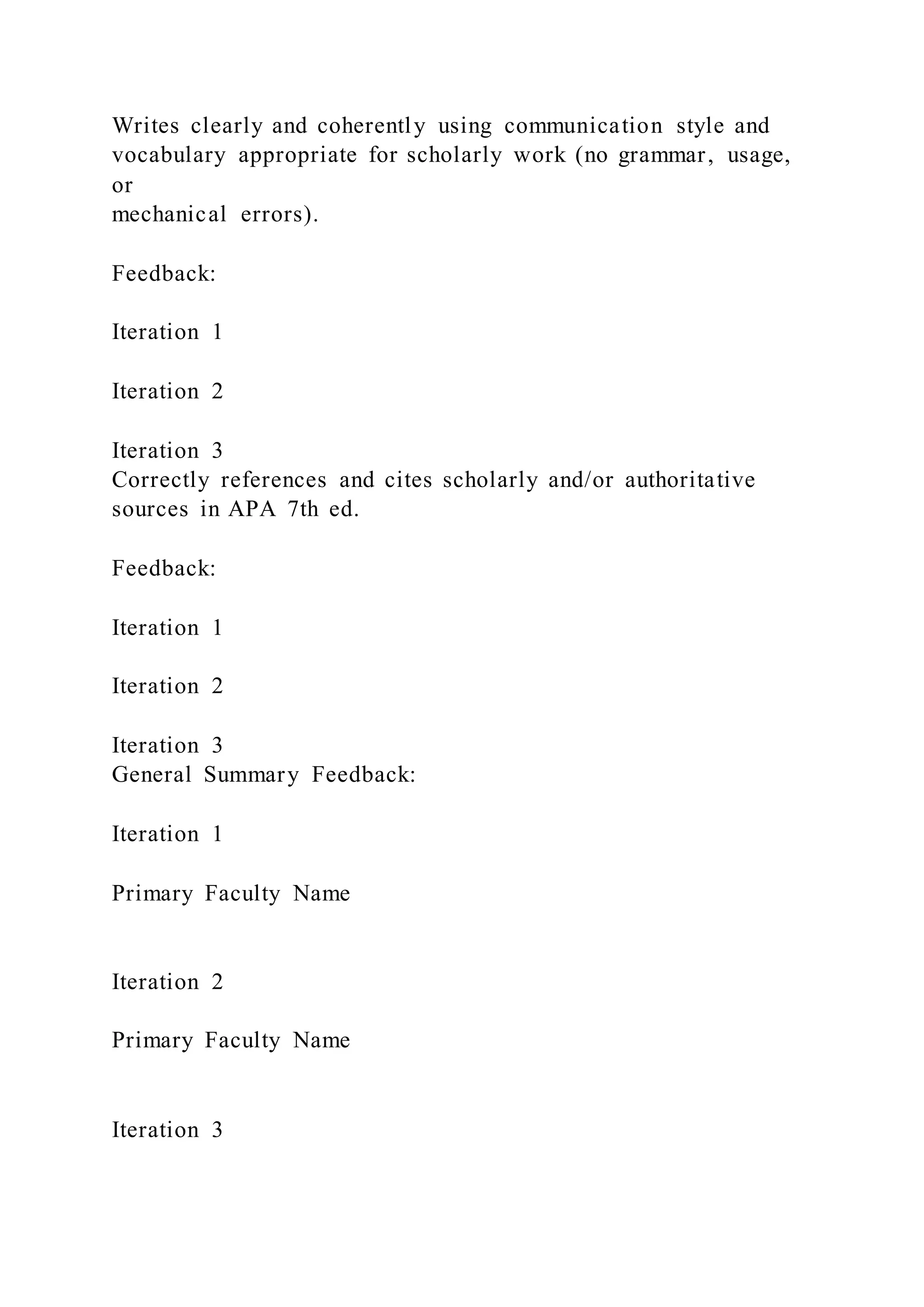
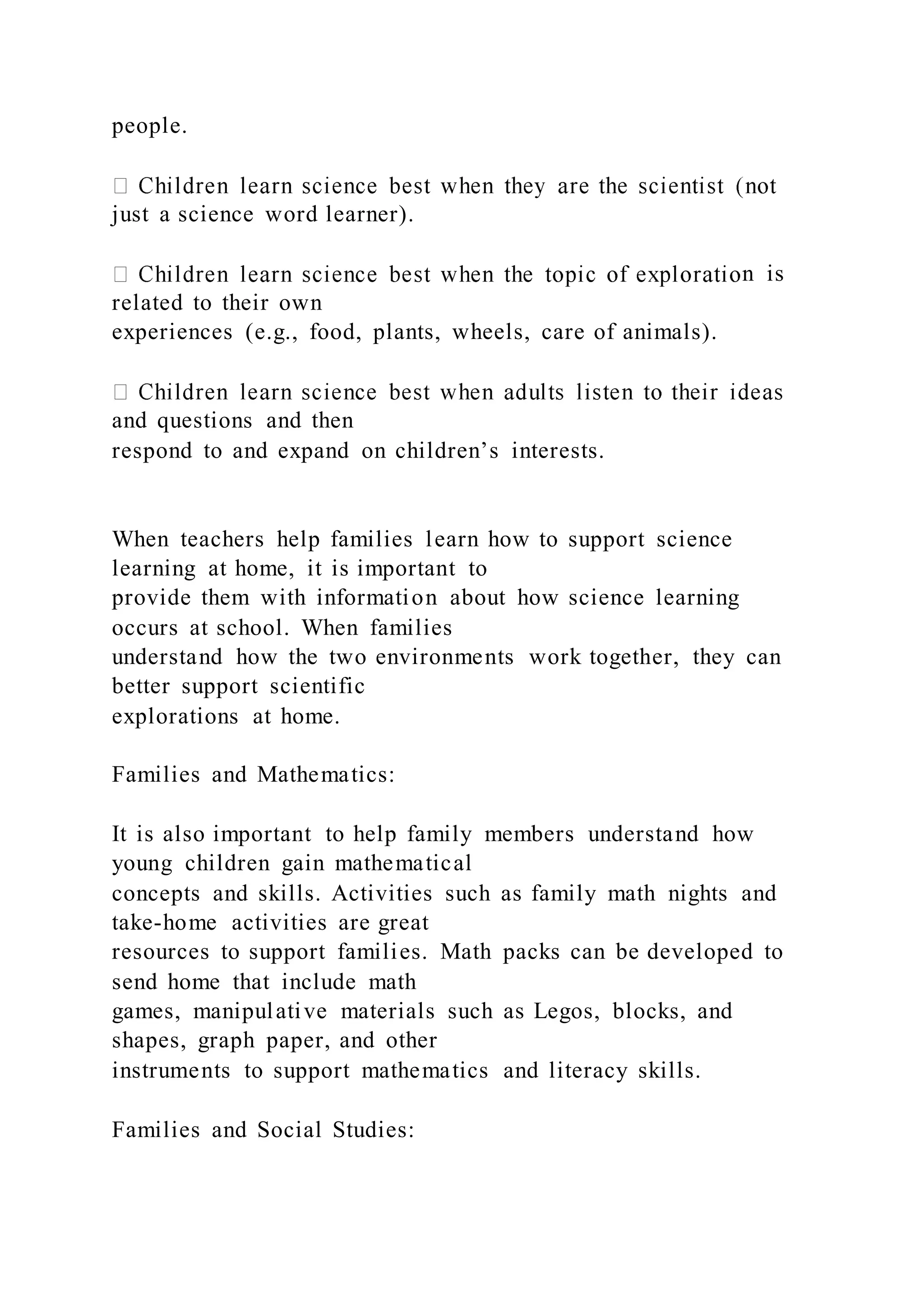
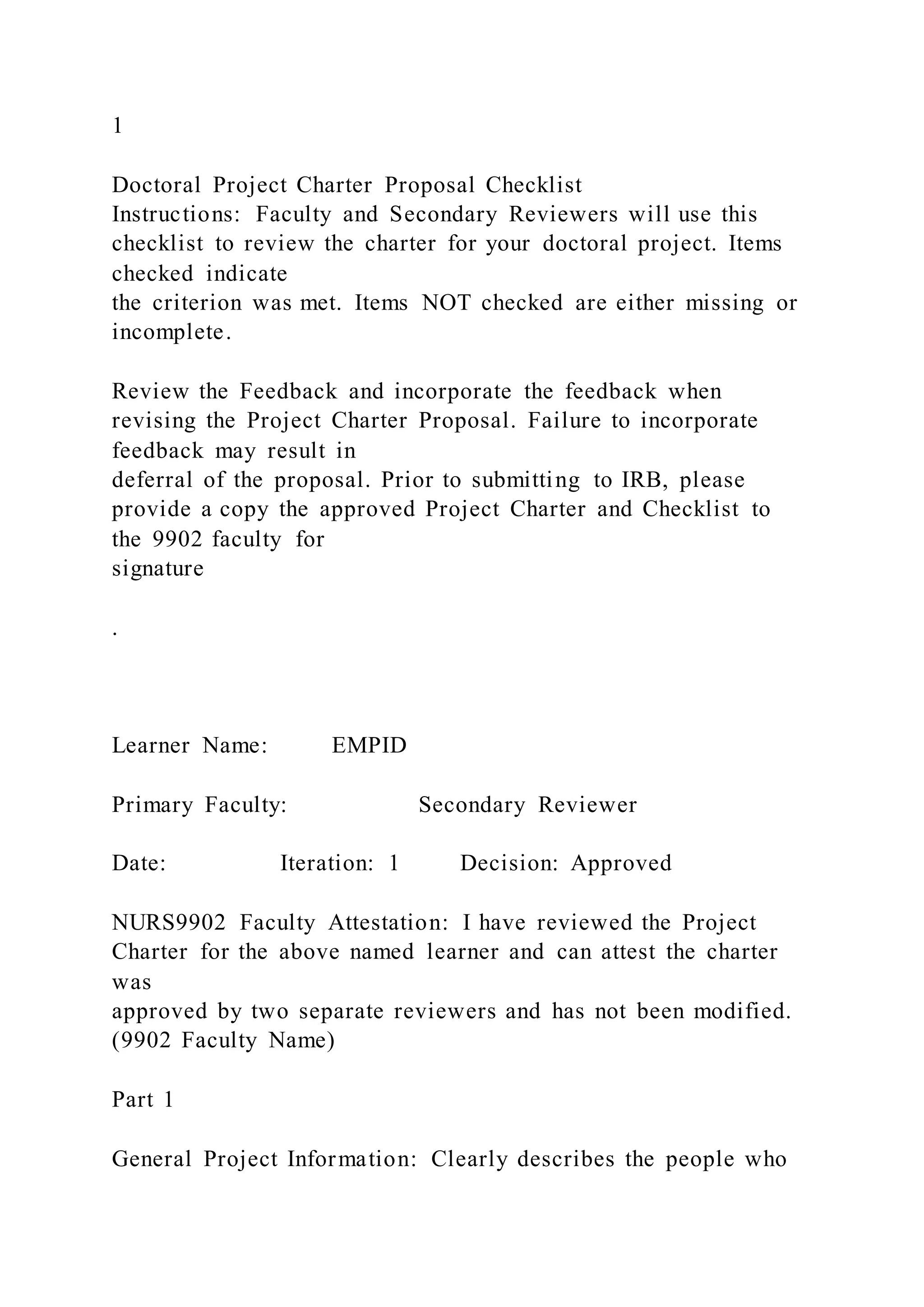
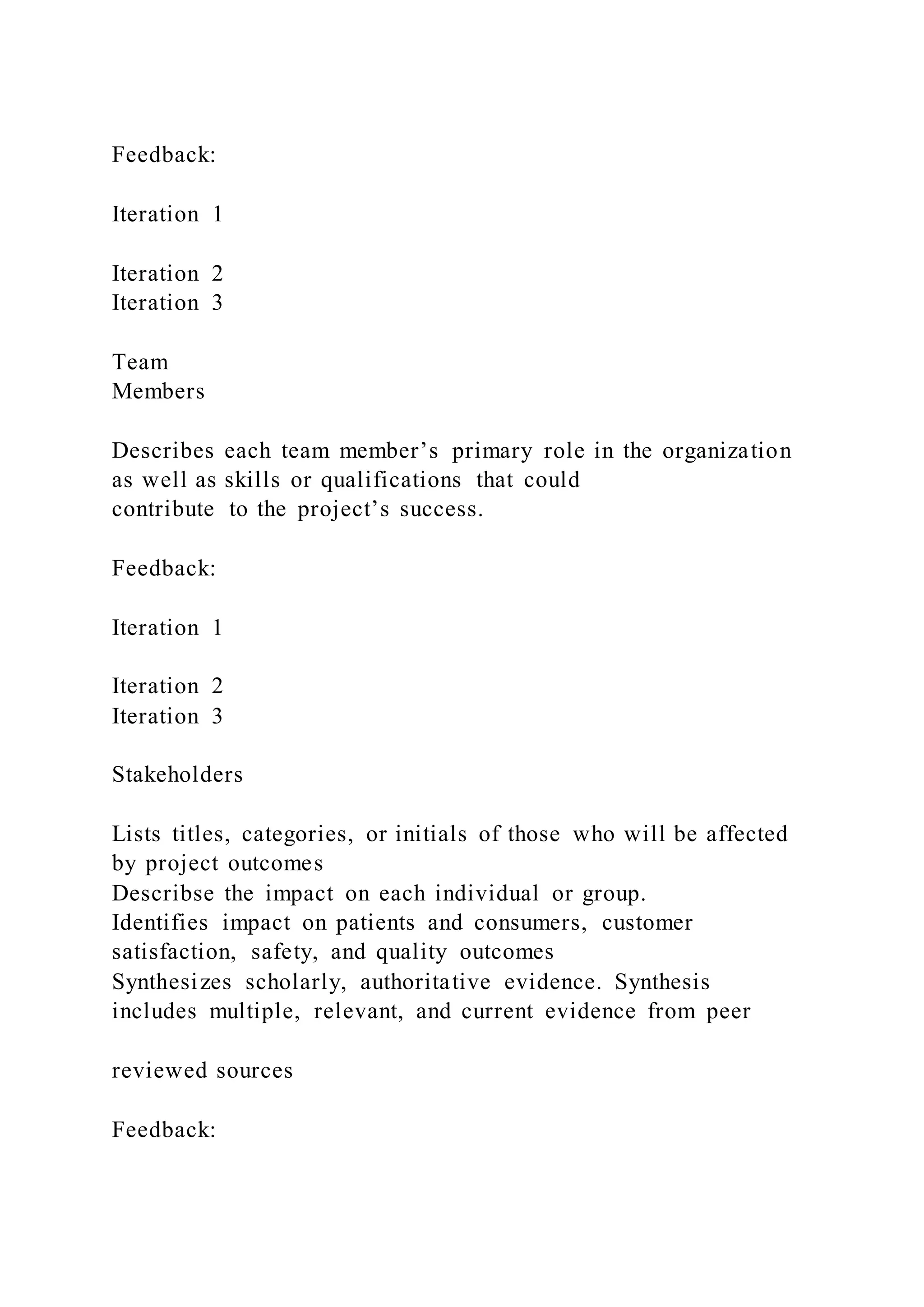
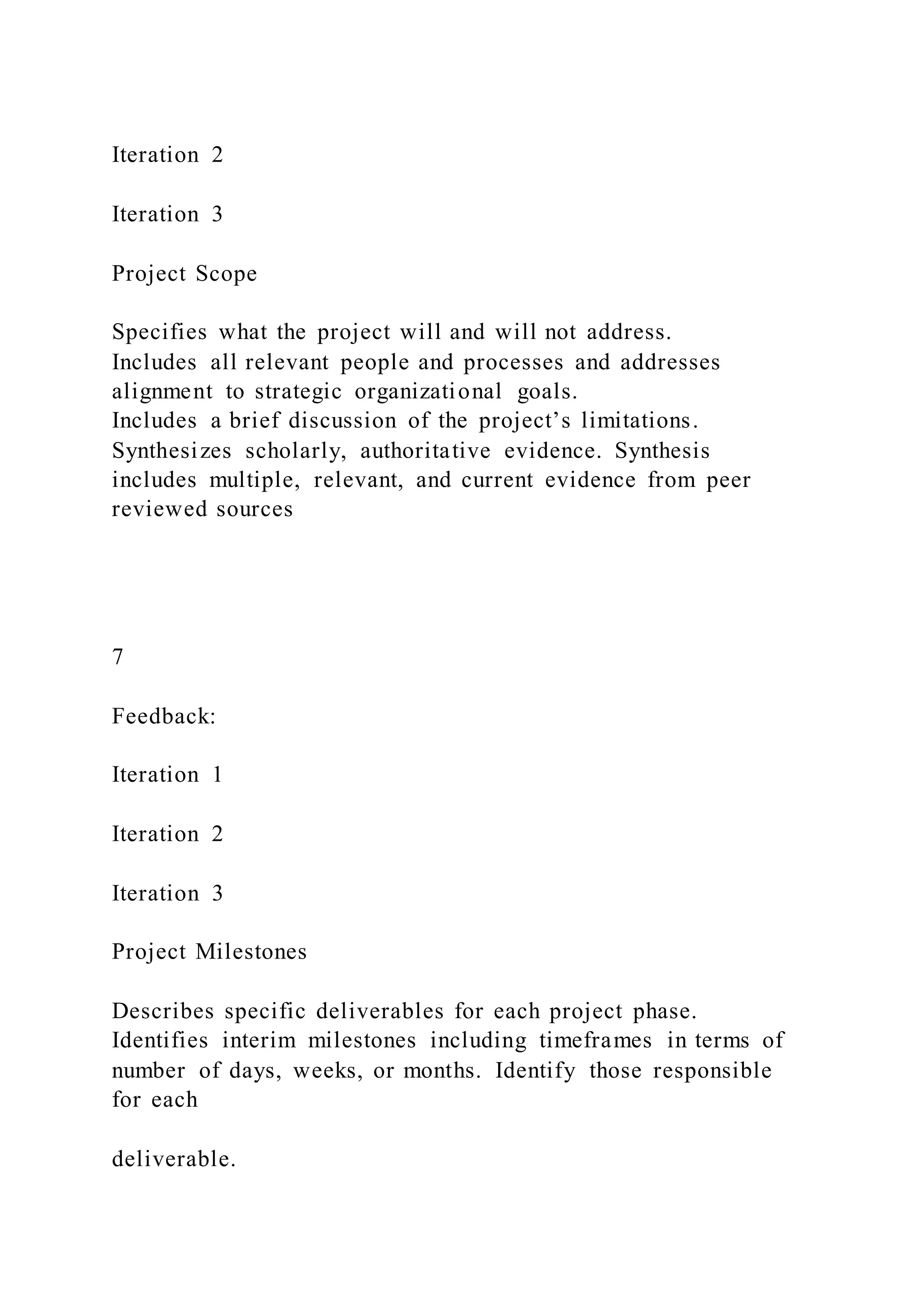
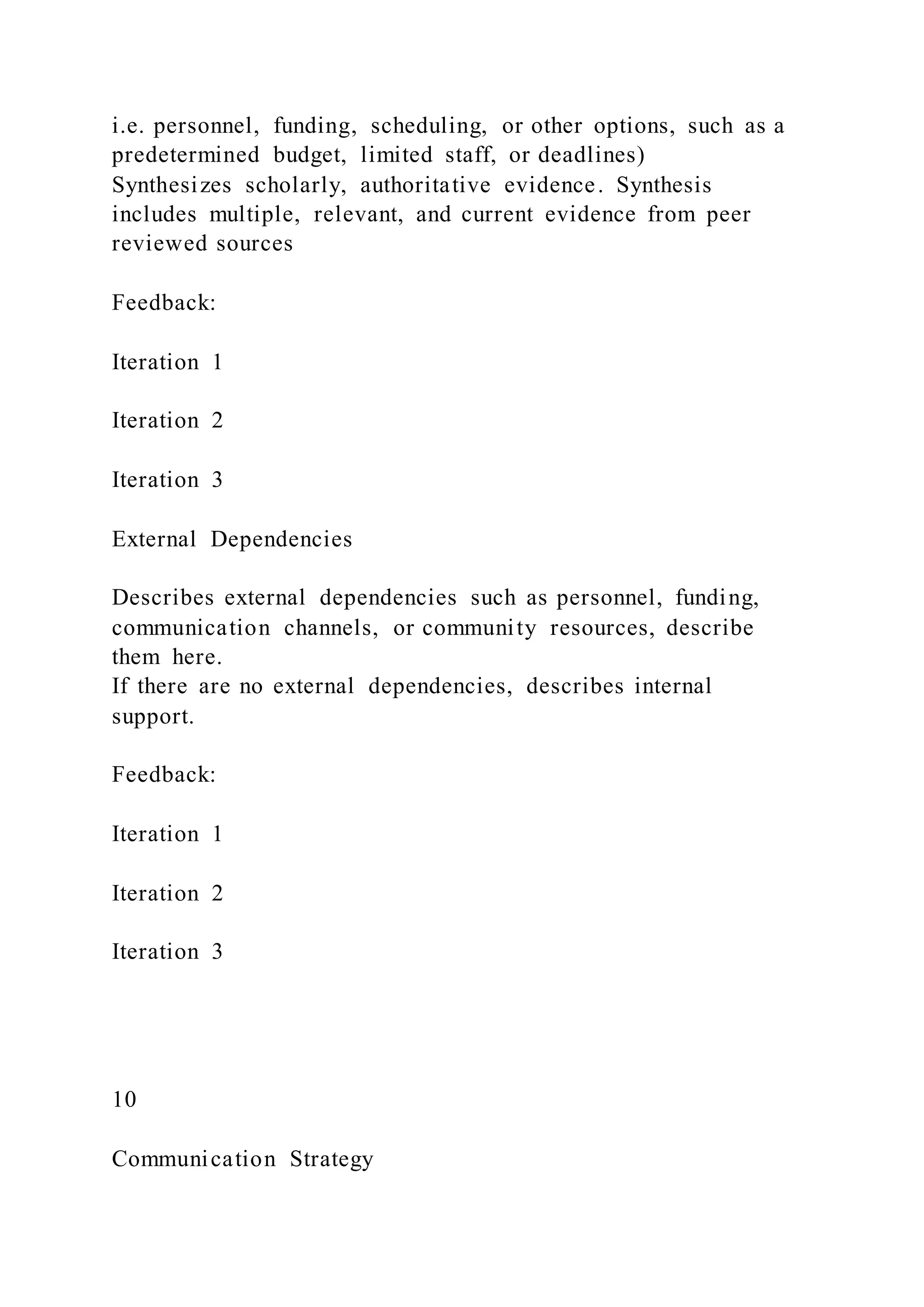
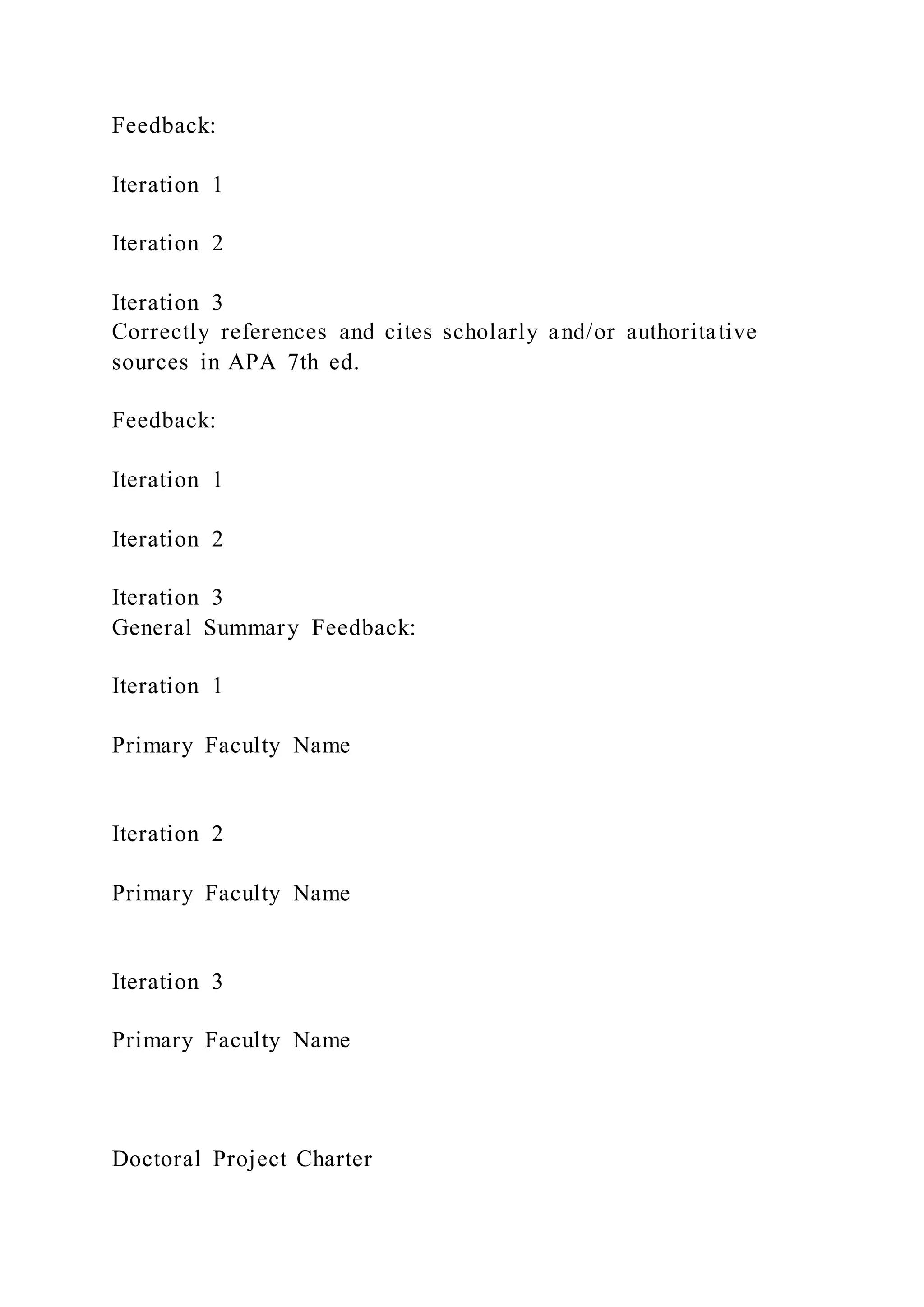
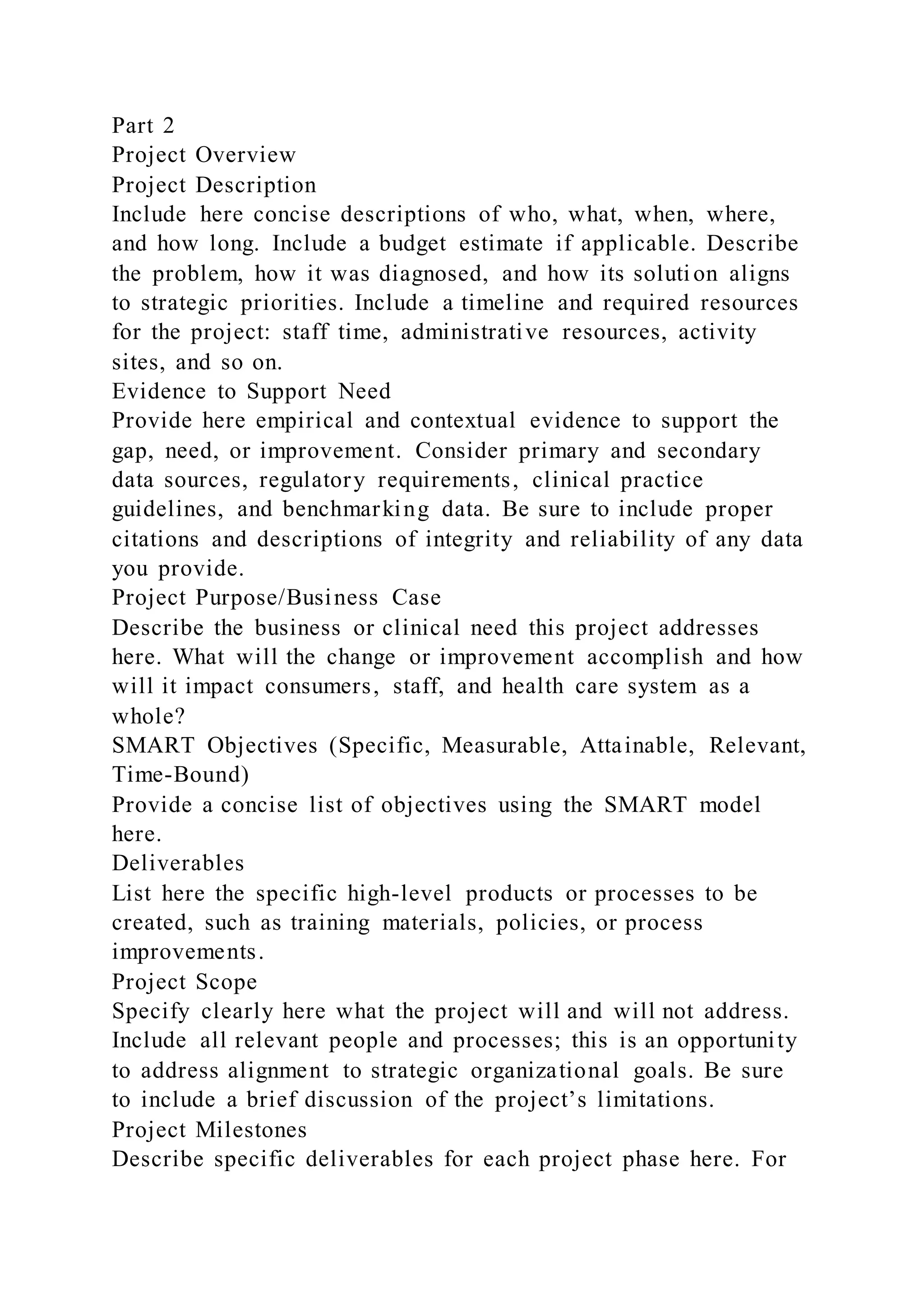
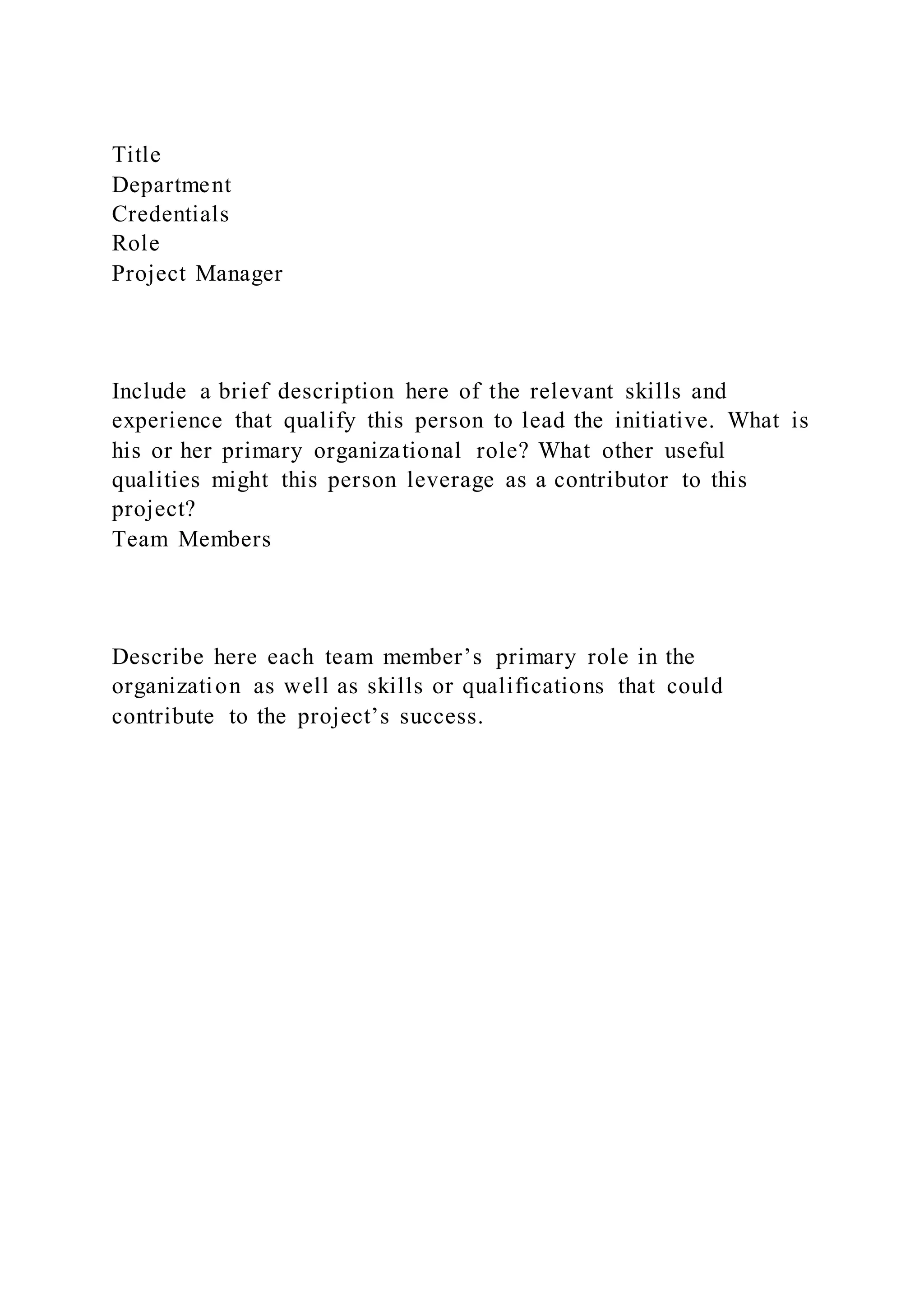
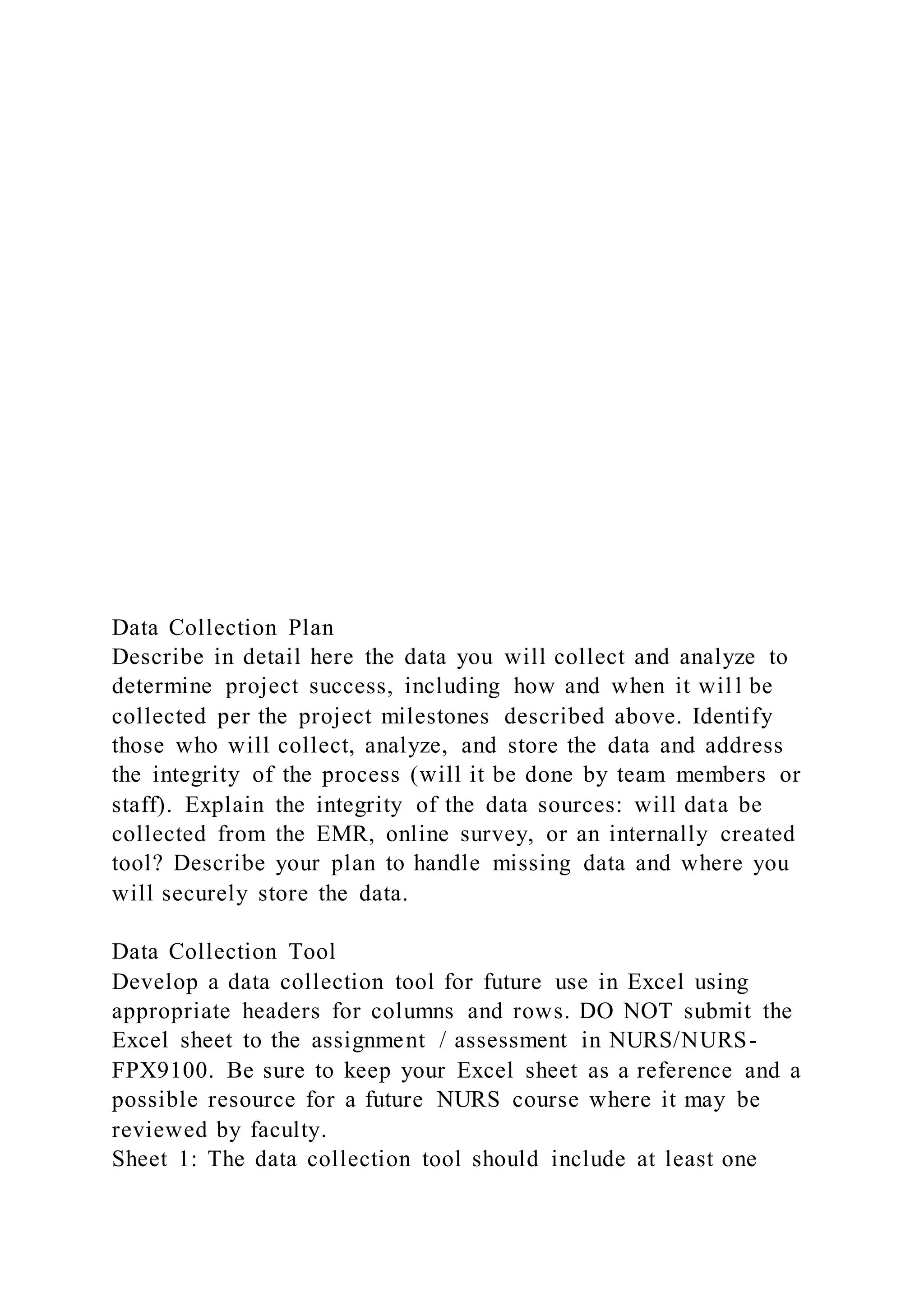
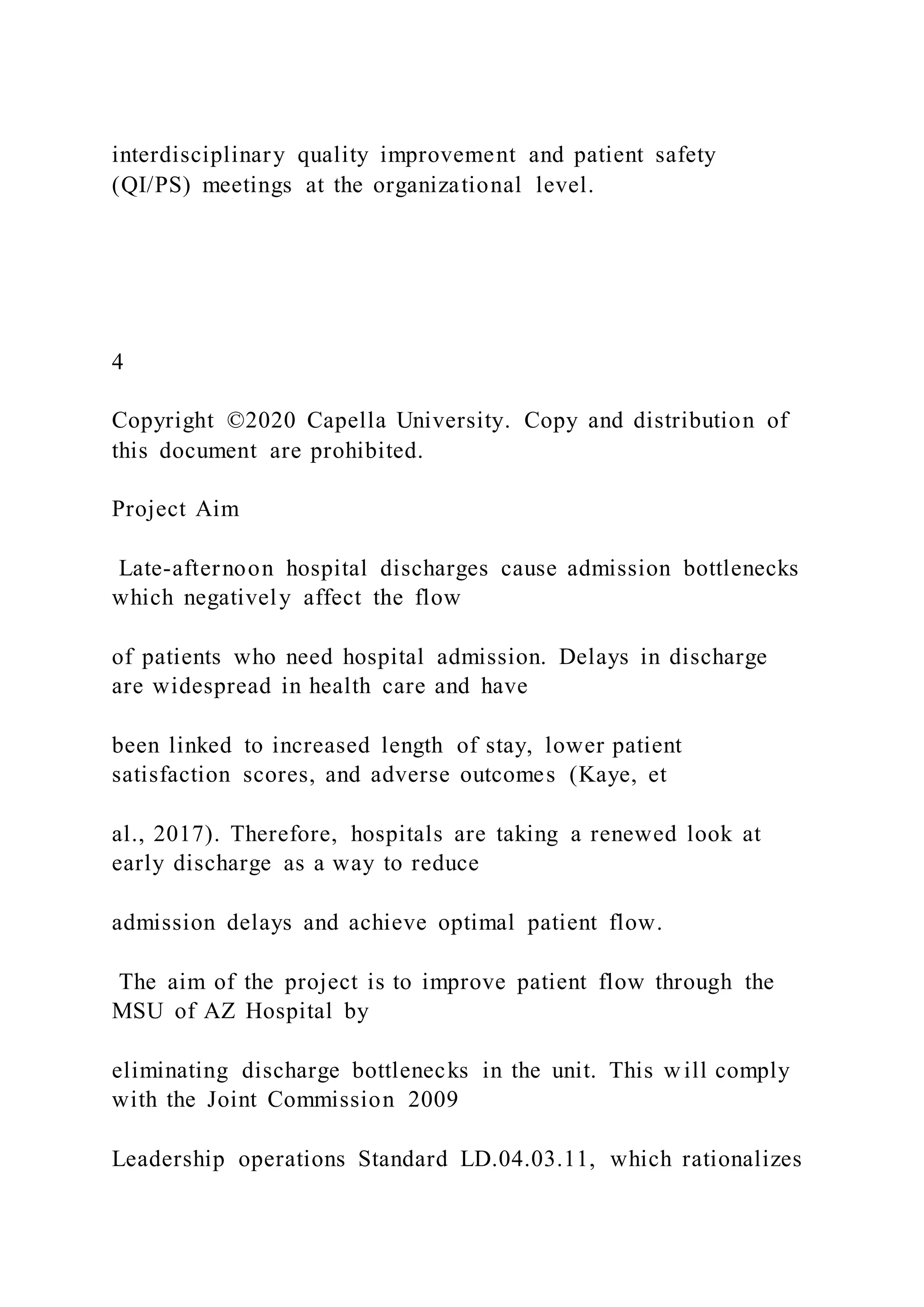
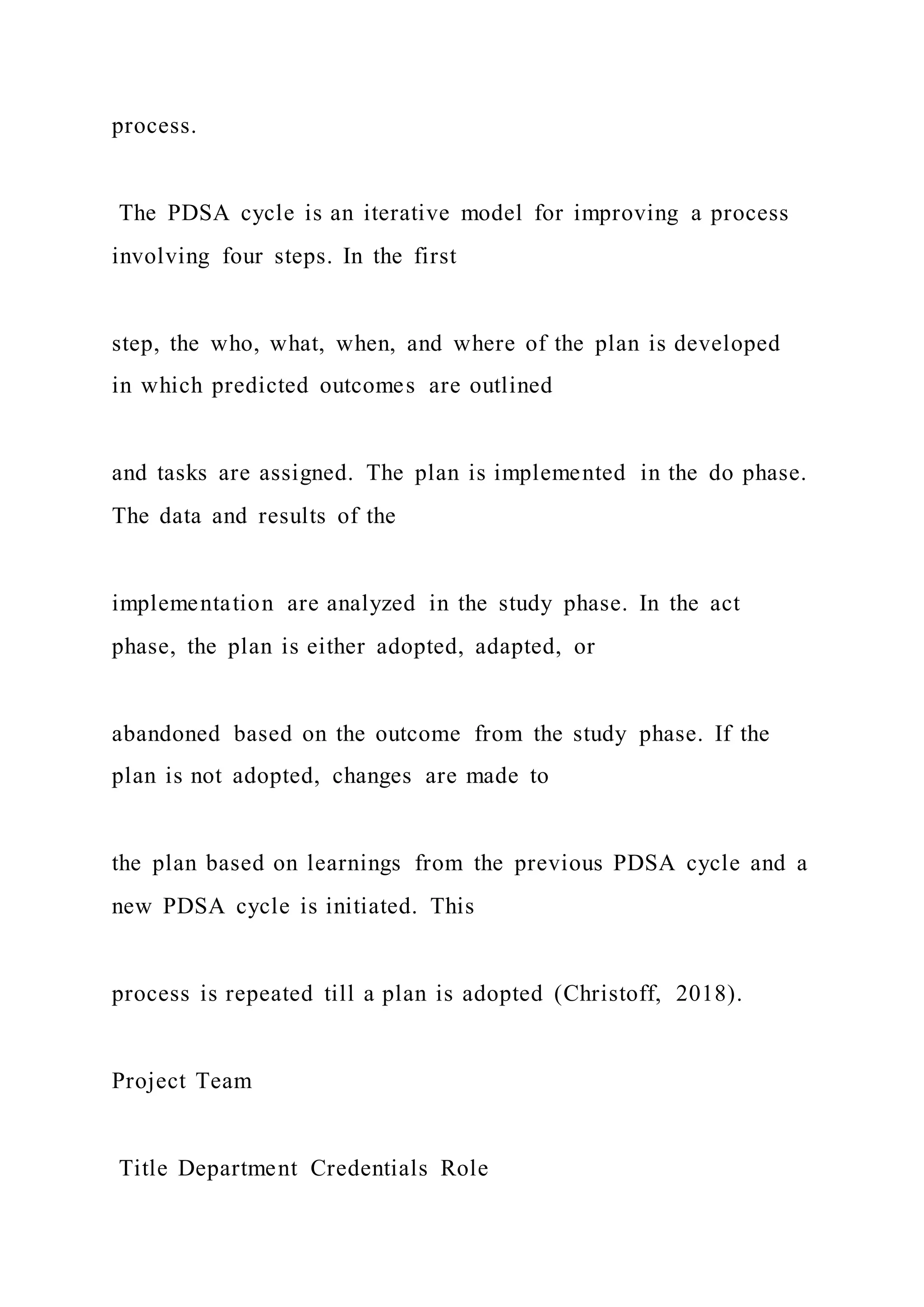
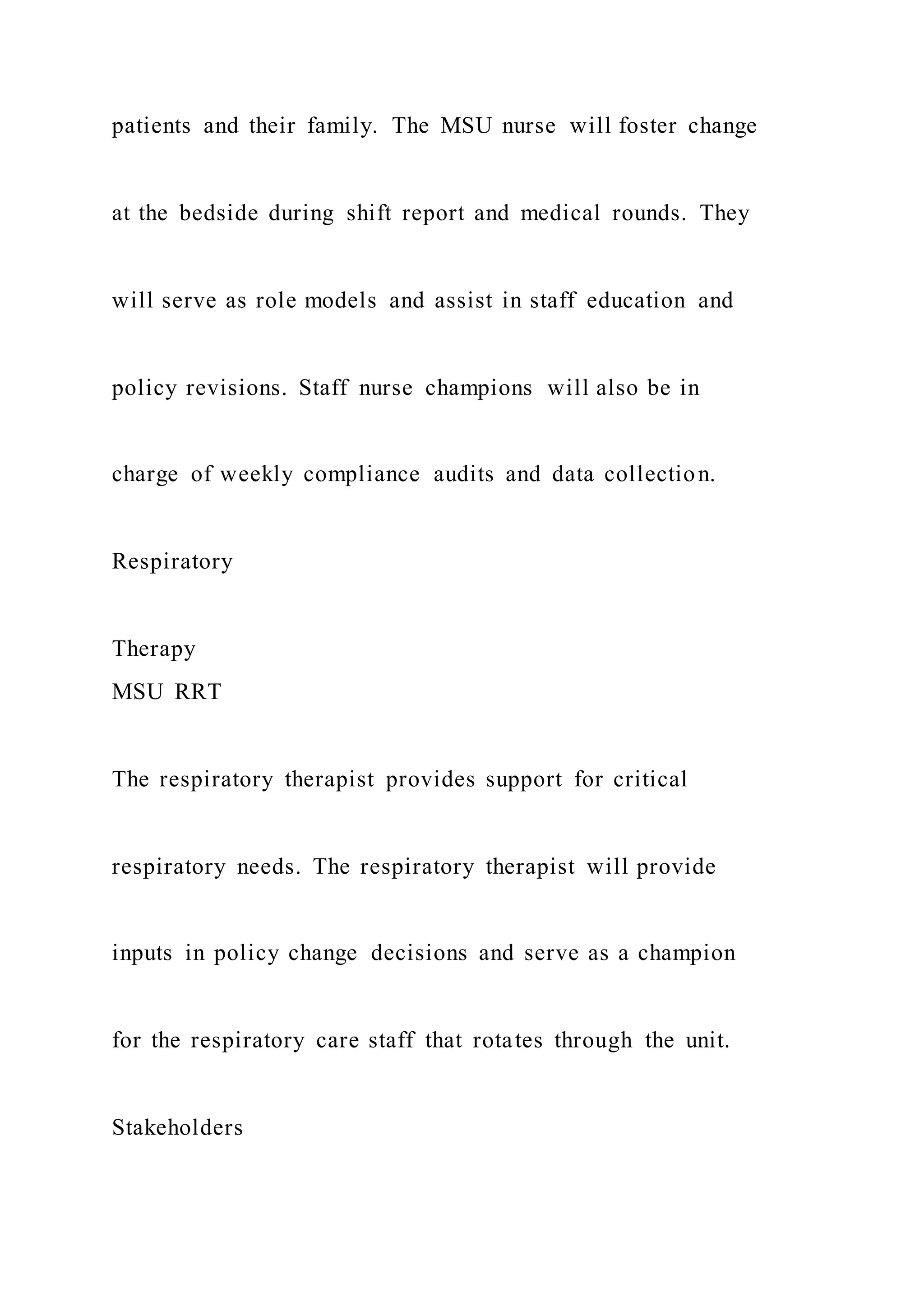
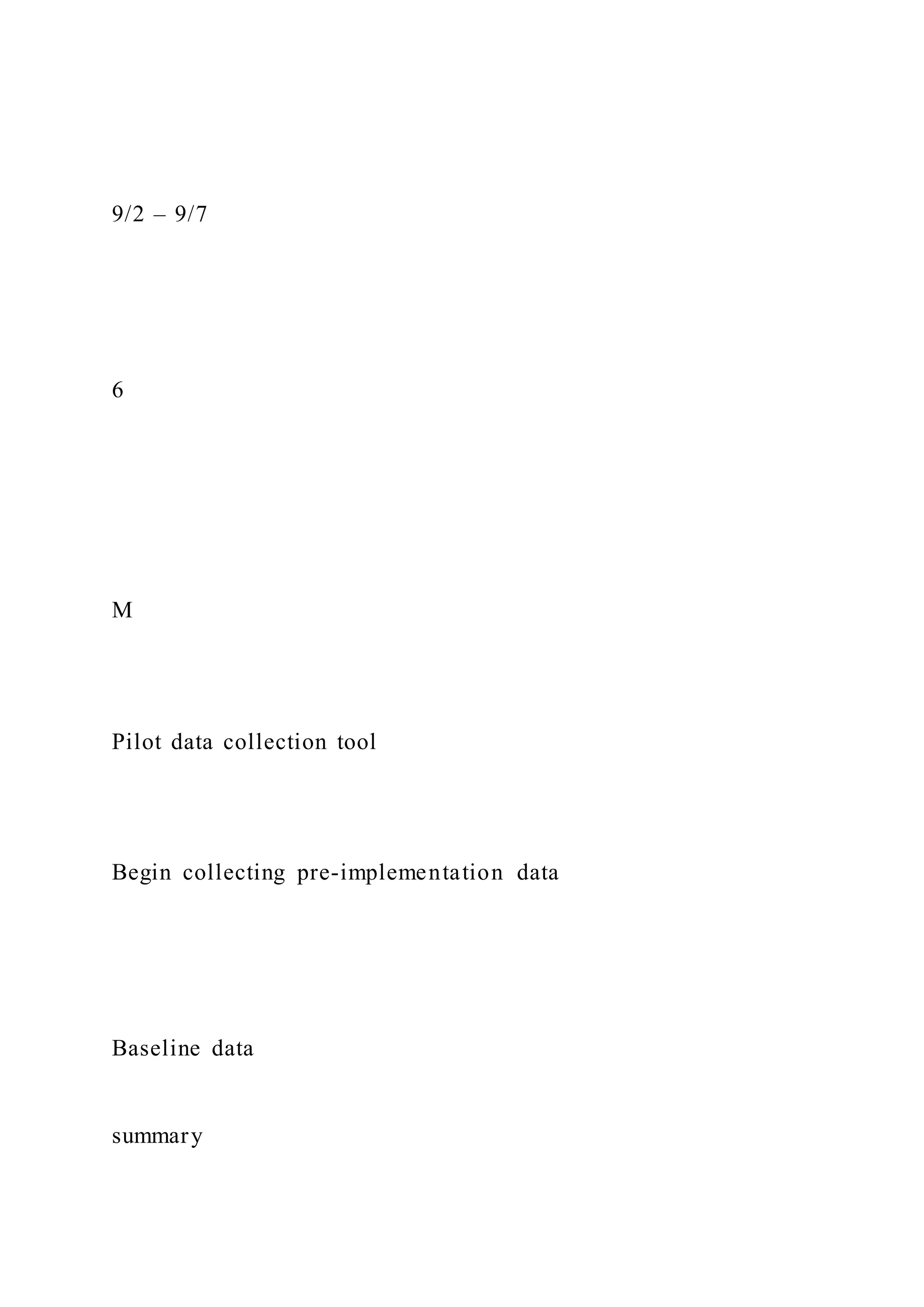
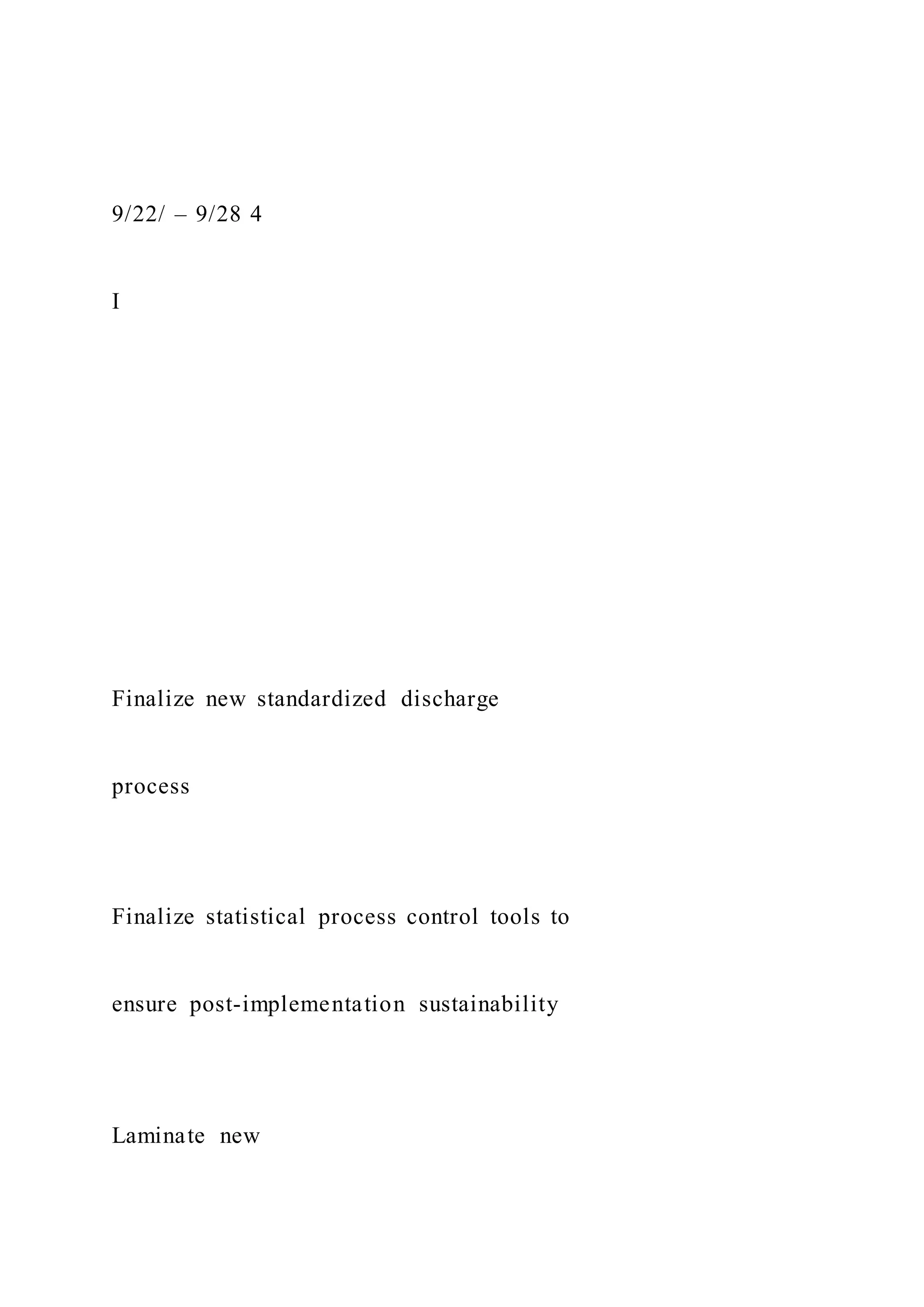
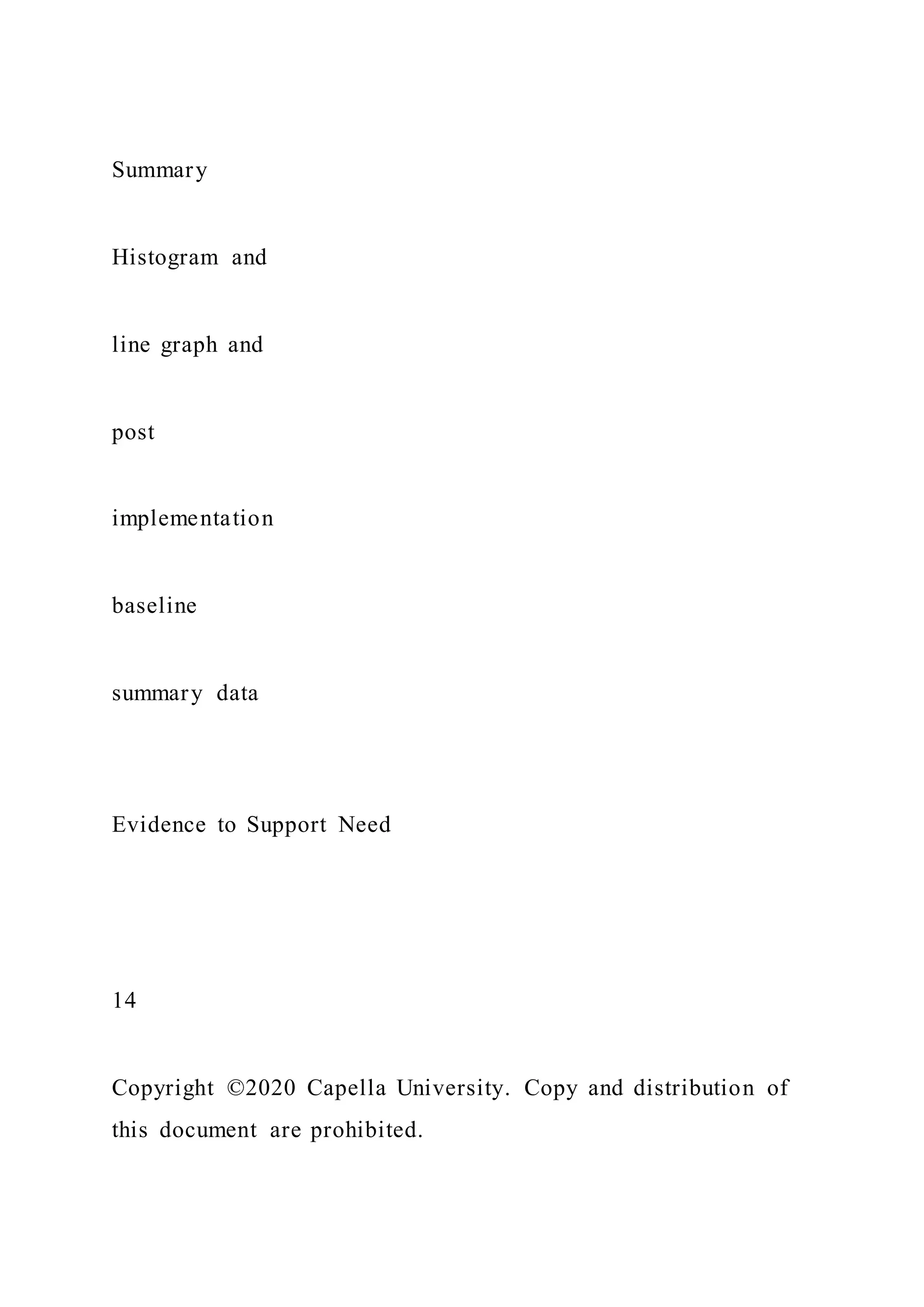
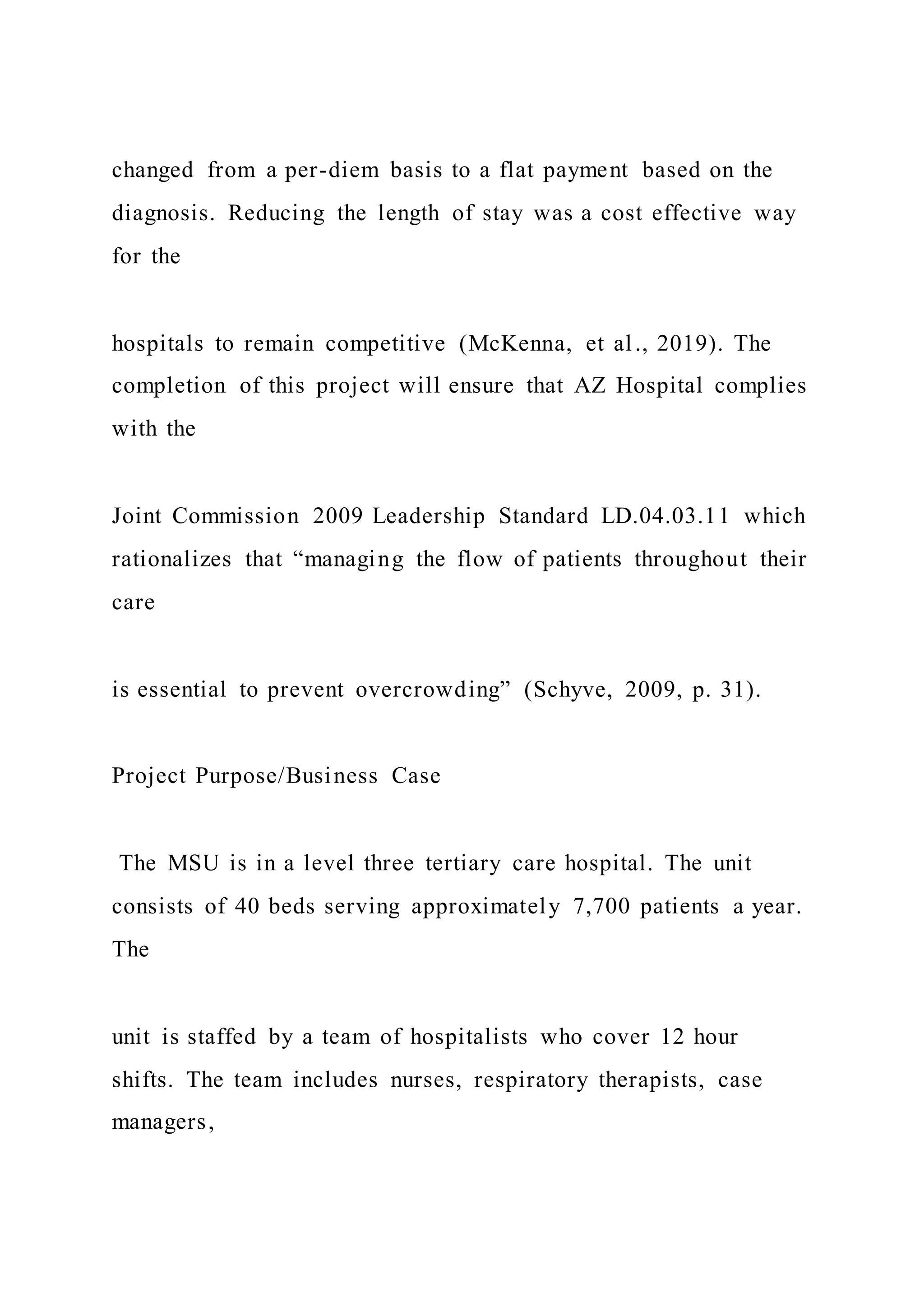
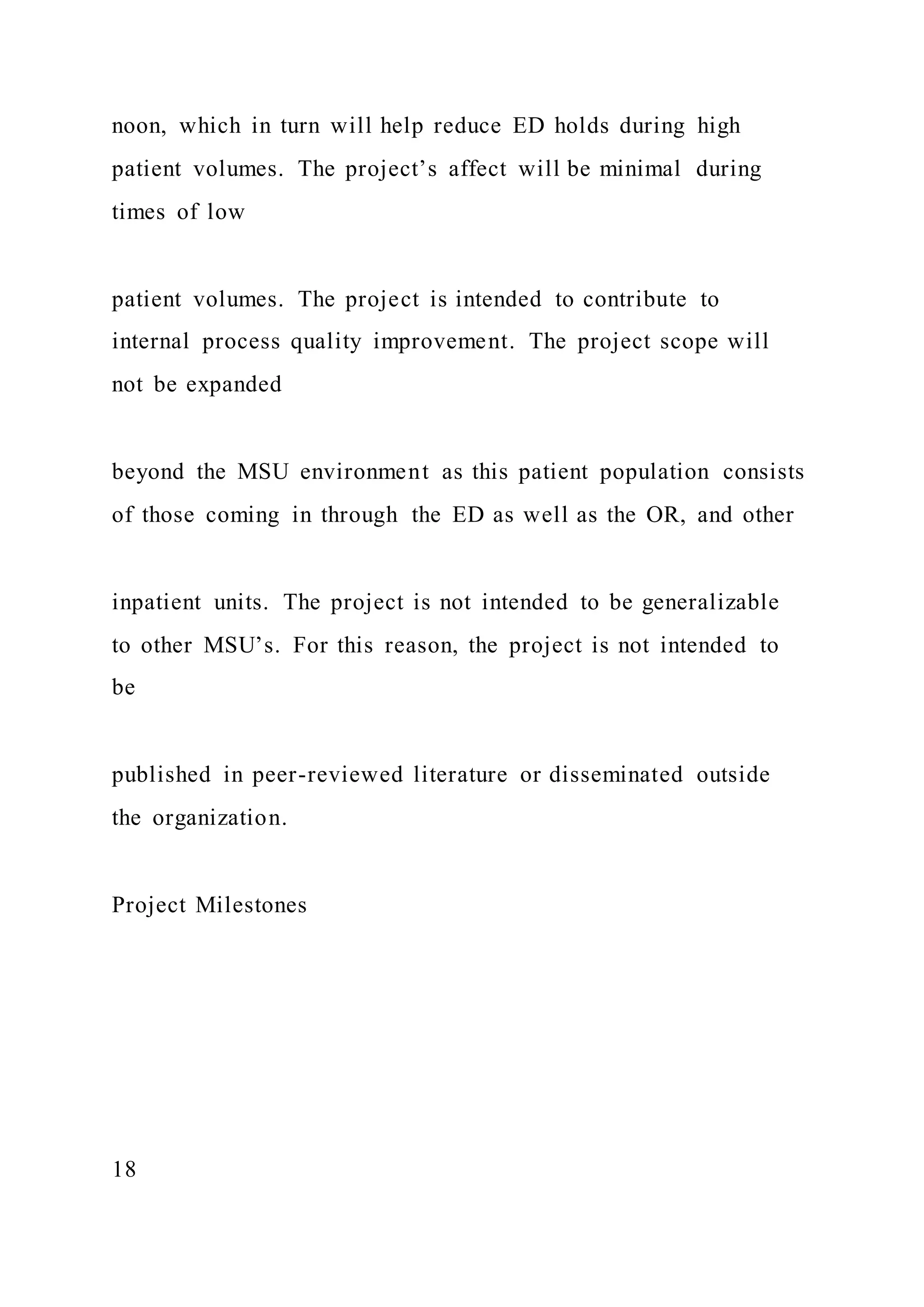
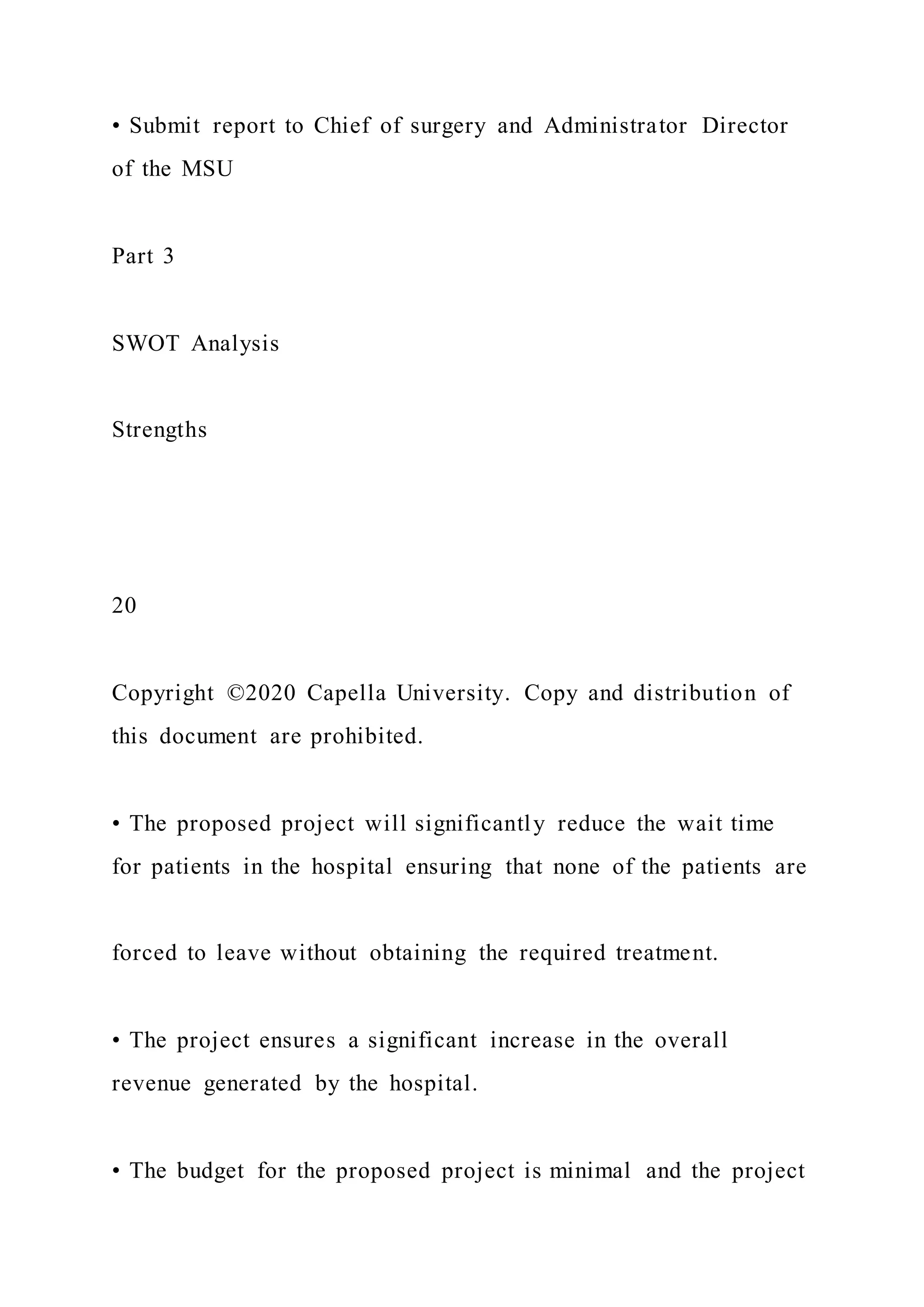
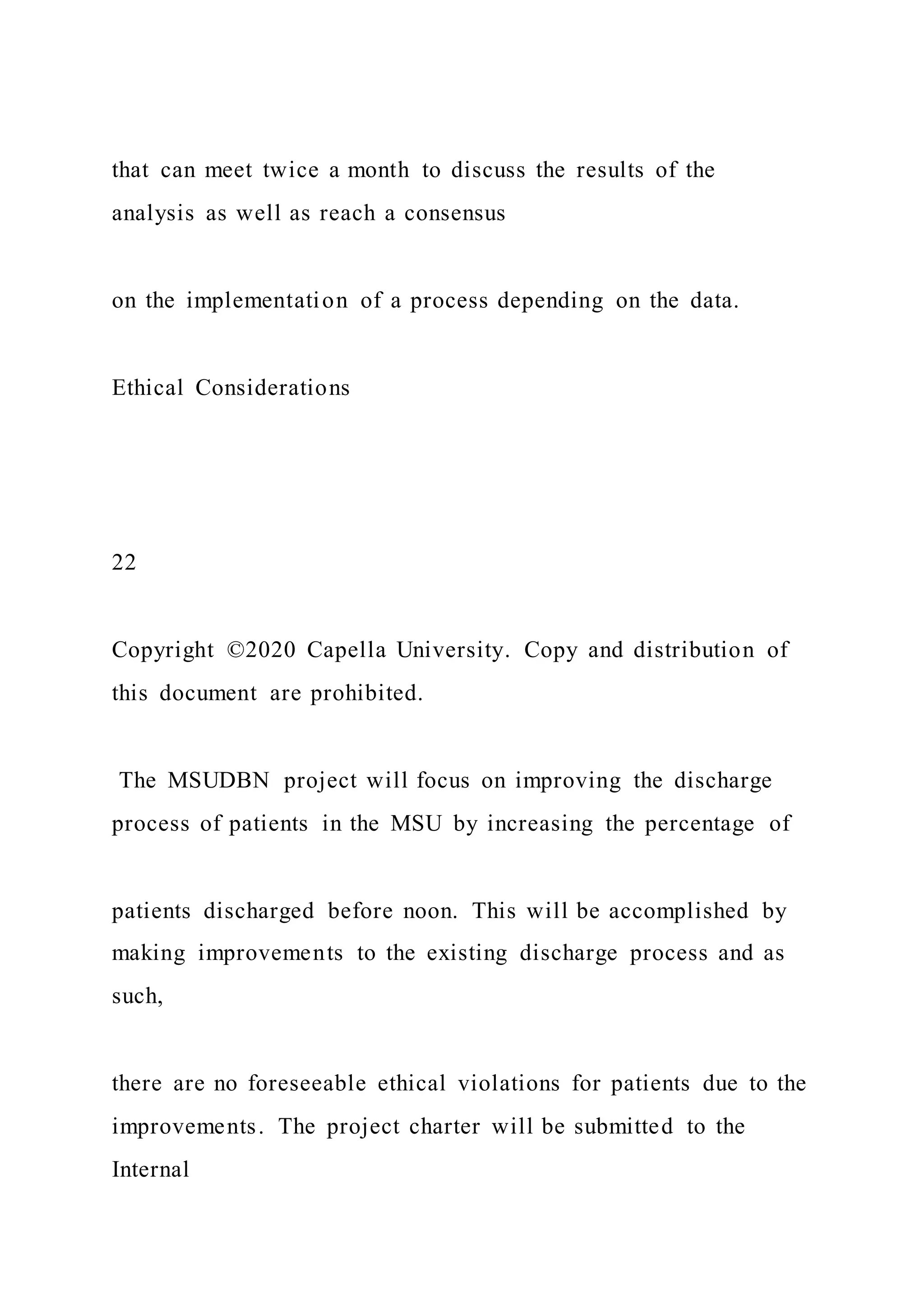
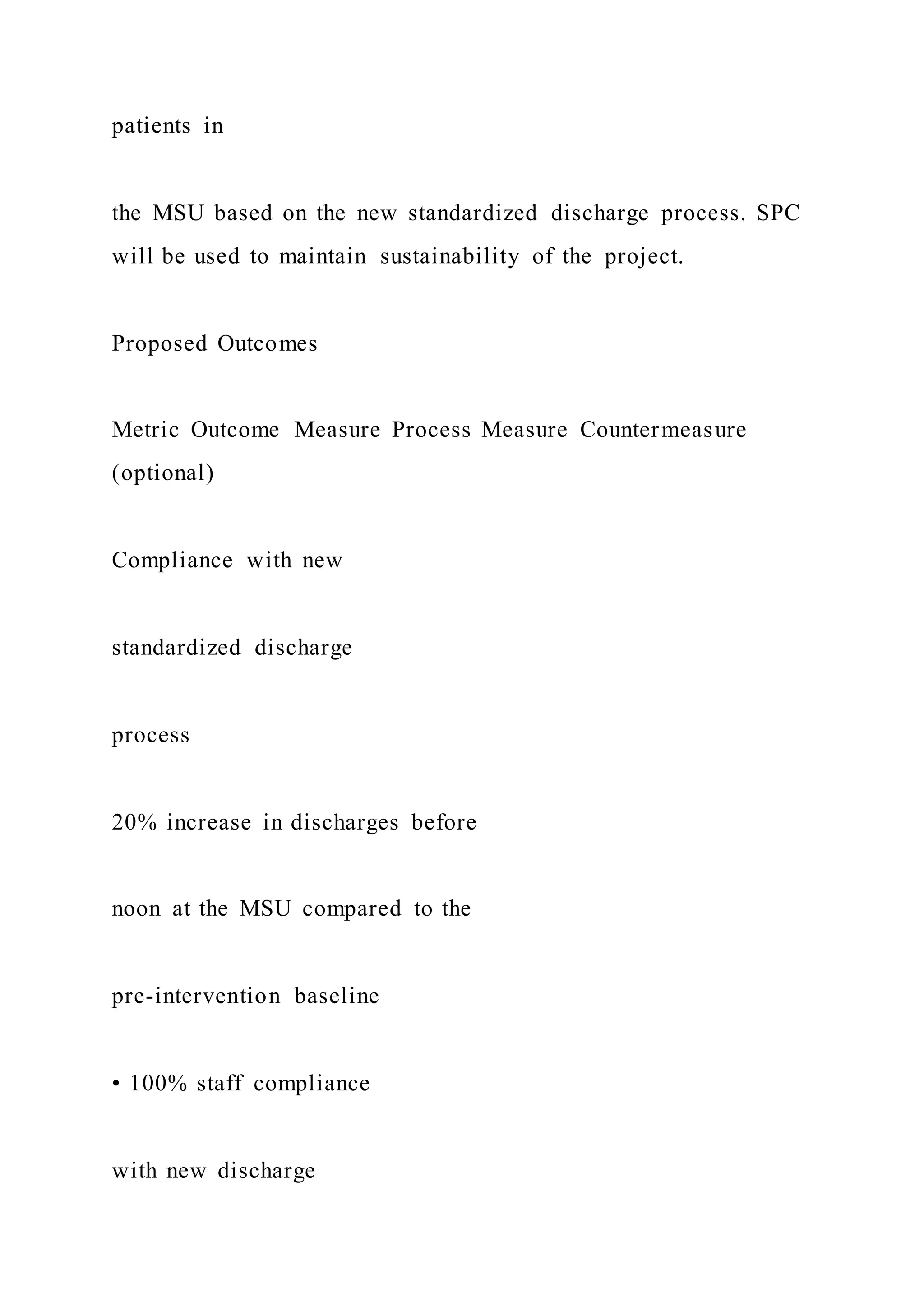
![Outcome Measure
Process Measure
Countermeasure (optional)
What is being measured to determine project success
Answers specifically final outcome (“So what?”), such as [X]
percent patient satisfaction rate increase
Measures supporting final outcome such as compliance, time
motion, competency
Measures to ensure that there are no negative consequences in
other areas](https://image.slidesharecdn.com/1doctoralprojectcharterproposalchecklistinstruct-220920053858-baf1555b/75/1-Doctoral-Project-Charter-Proposal-Checklist-Instruct-48-2048.jpg)
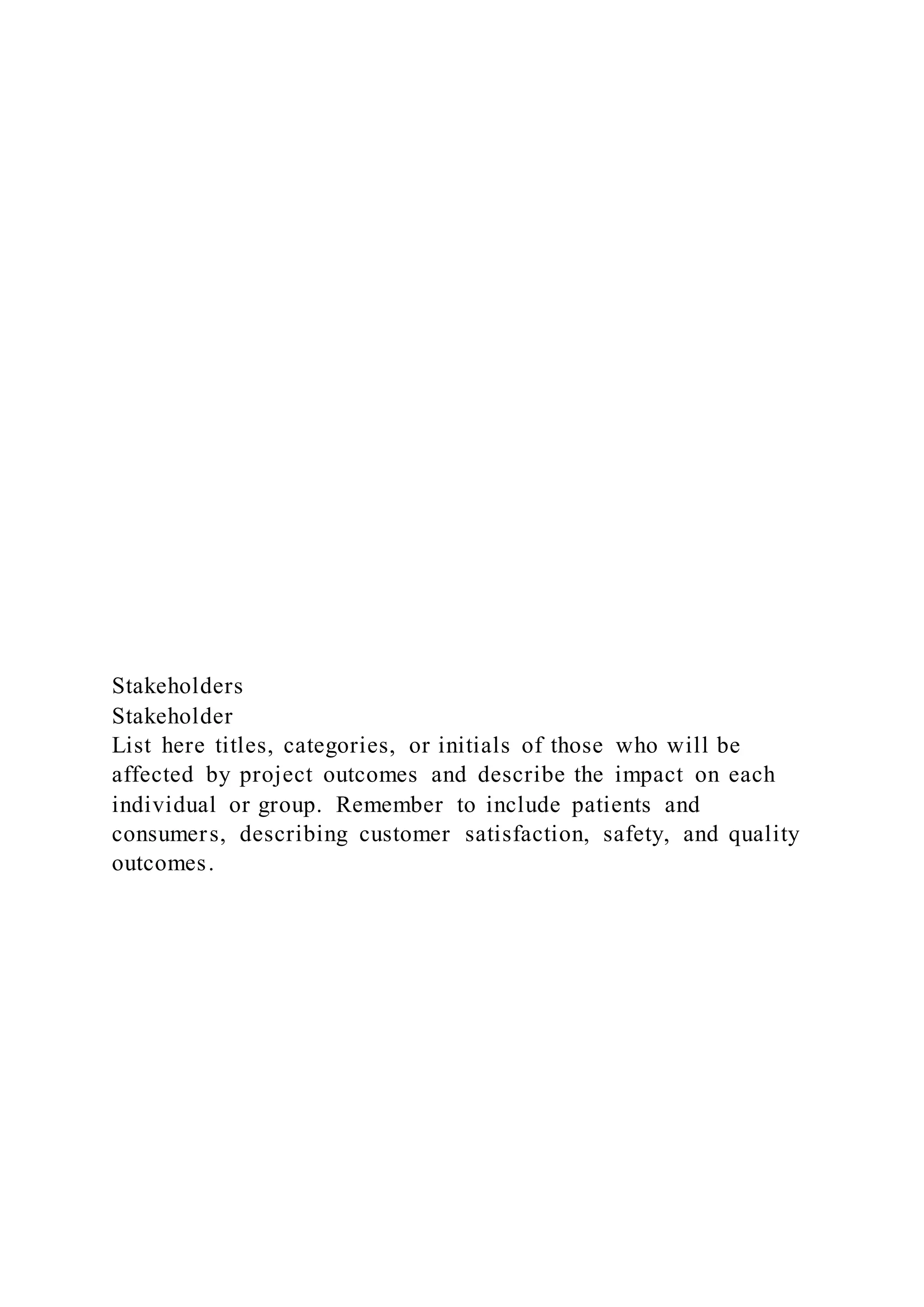
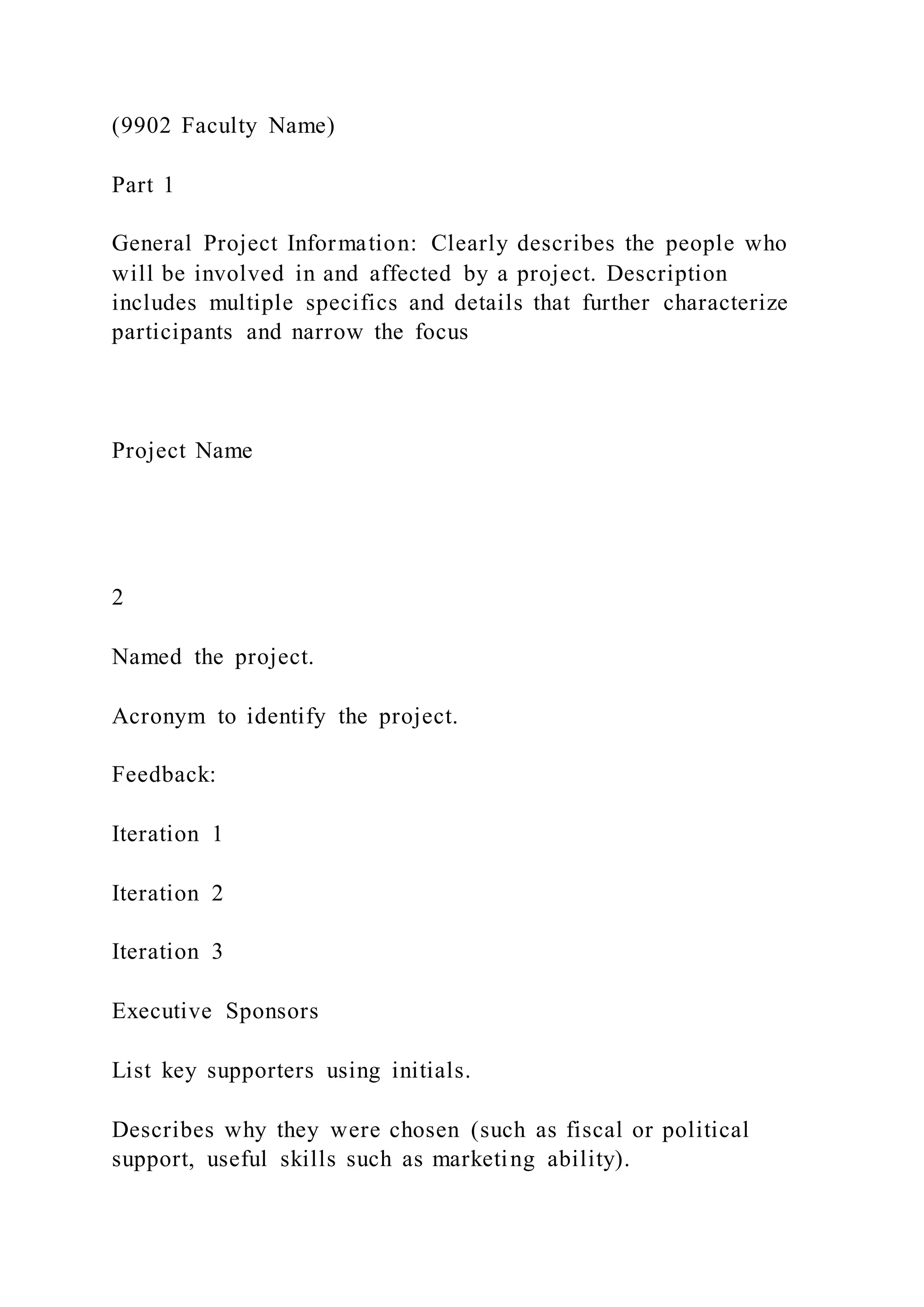
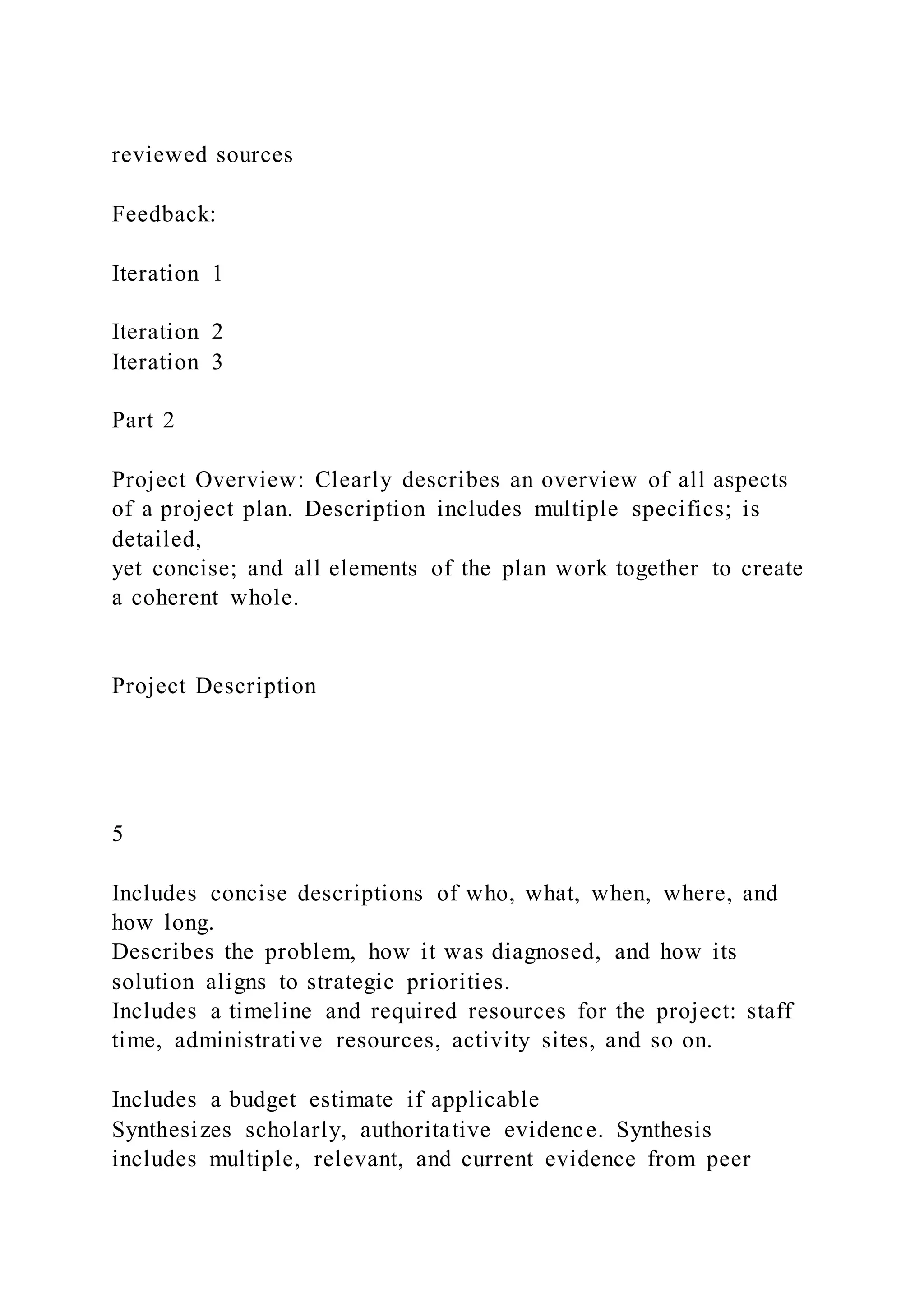
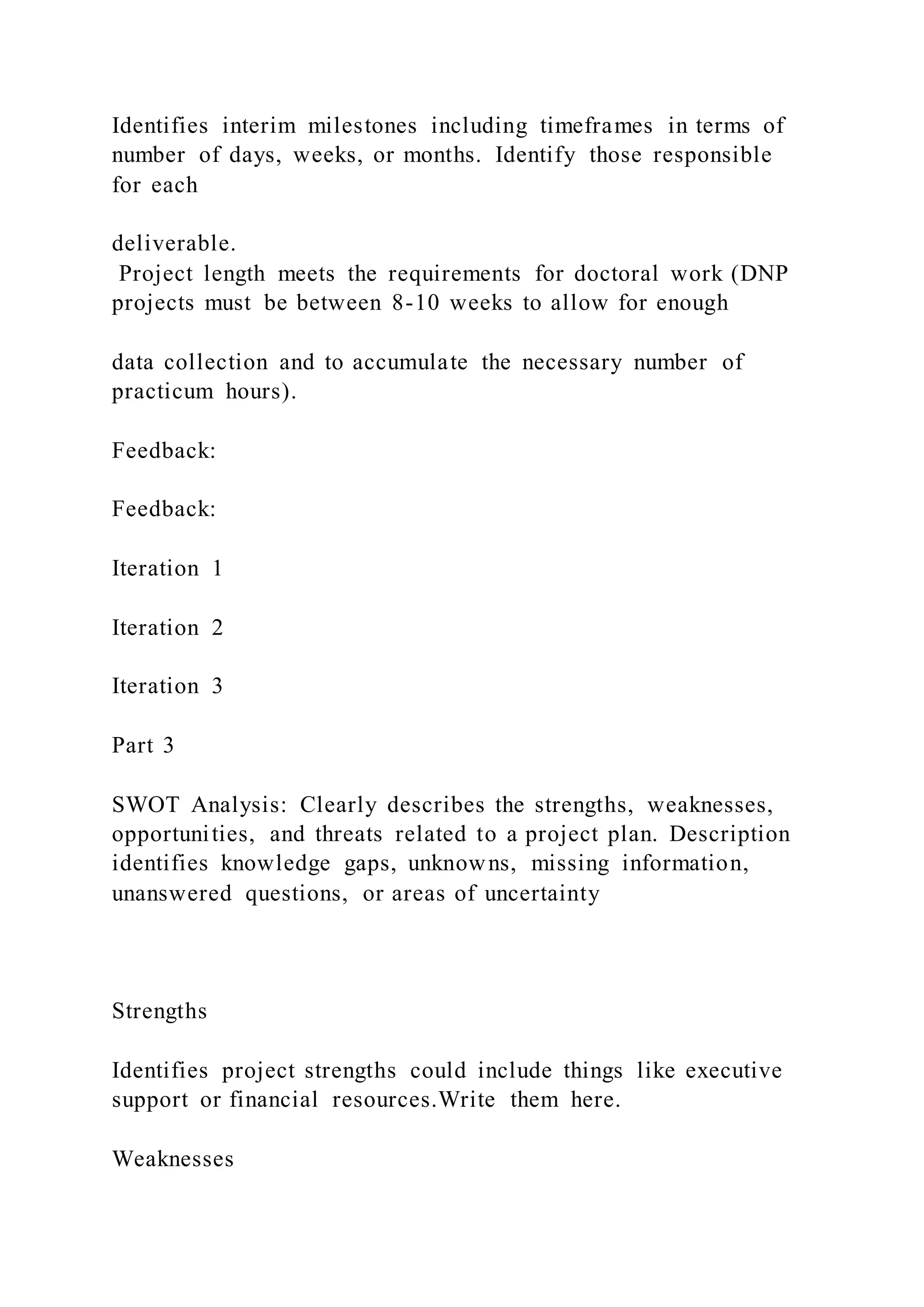
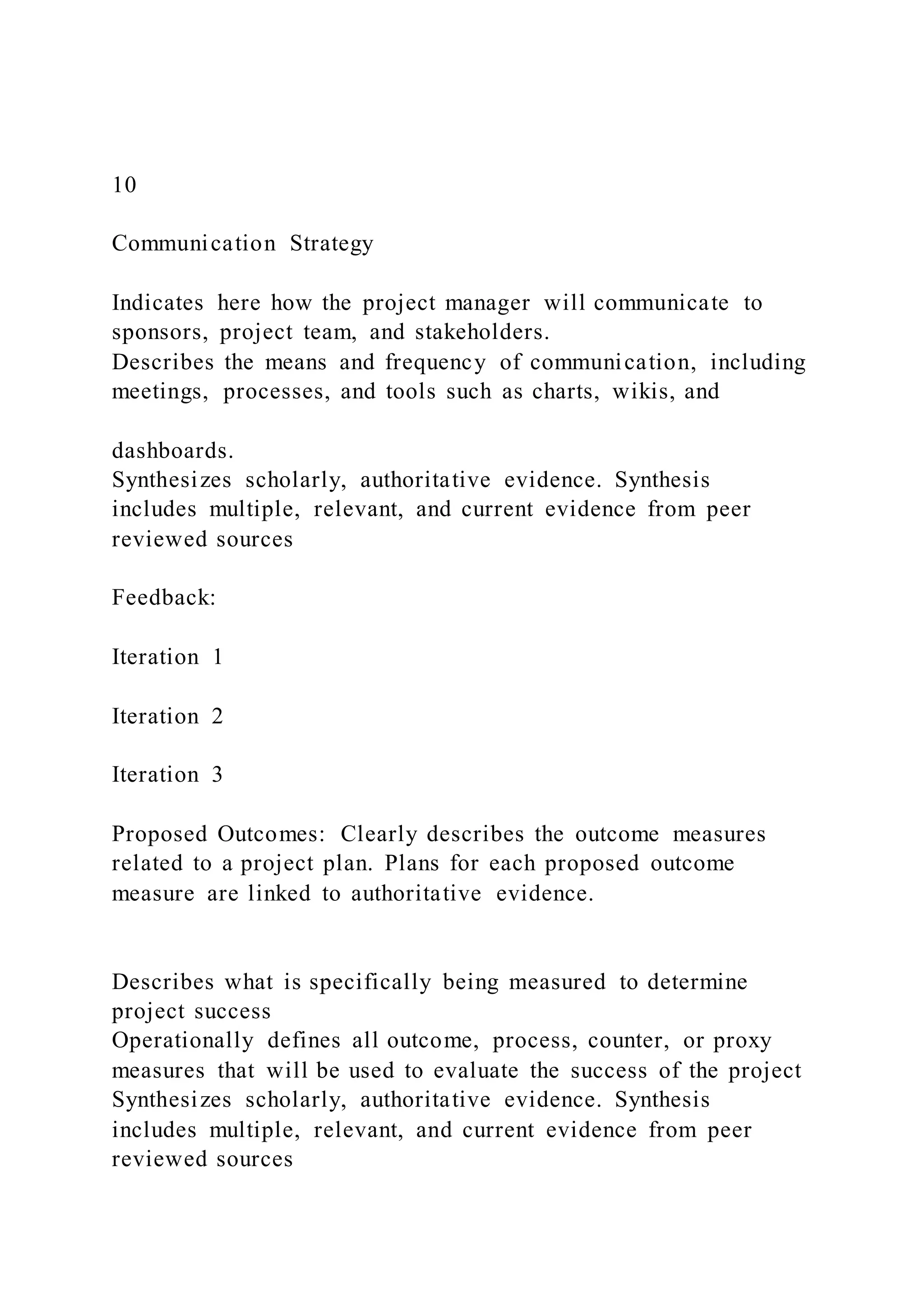
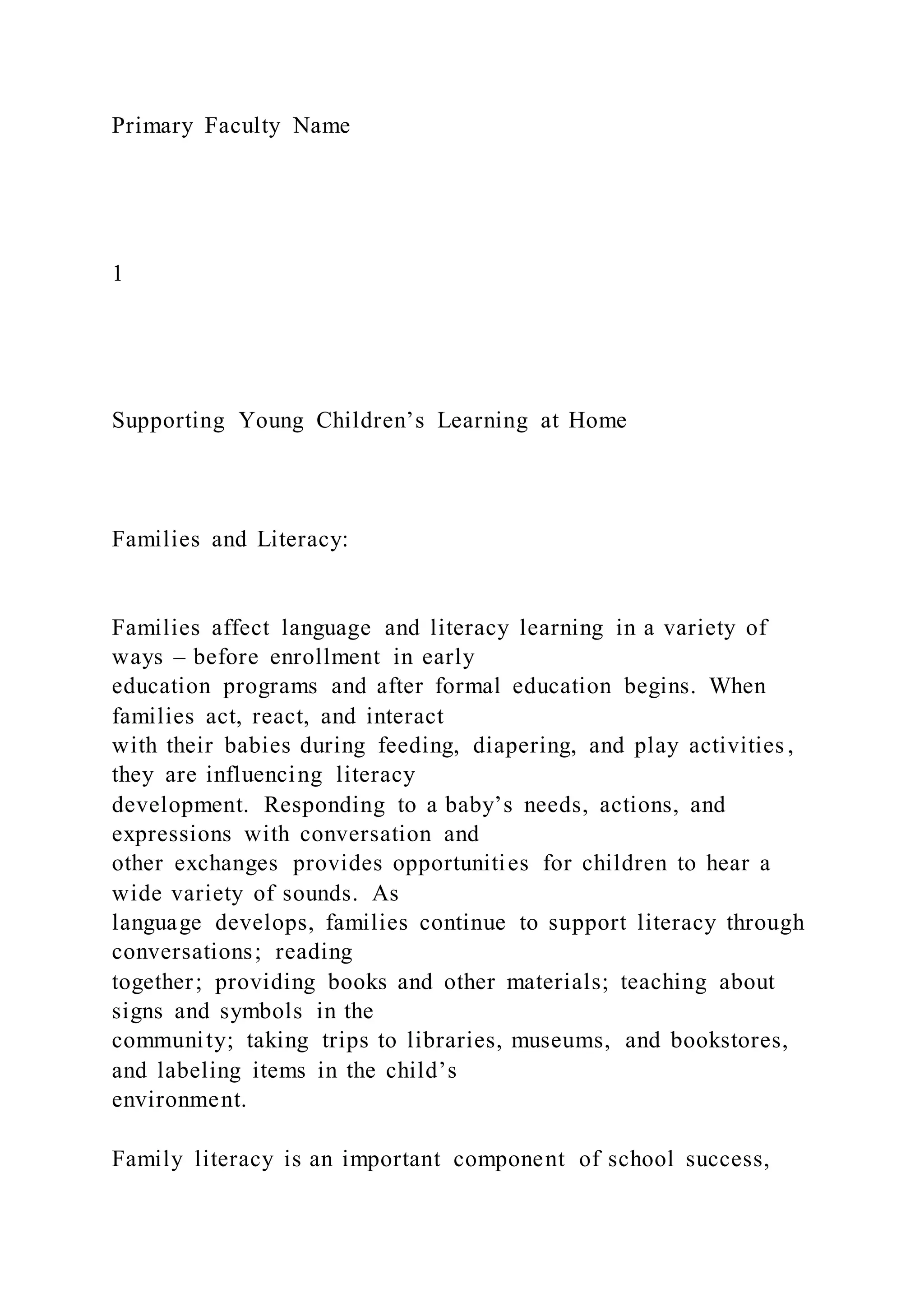
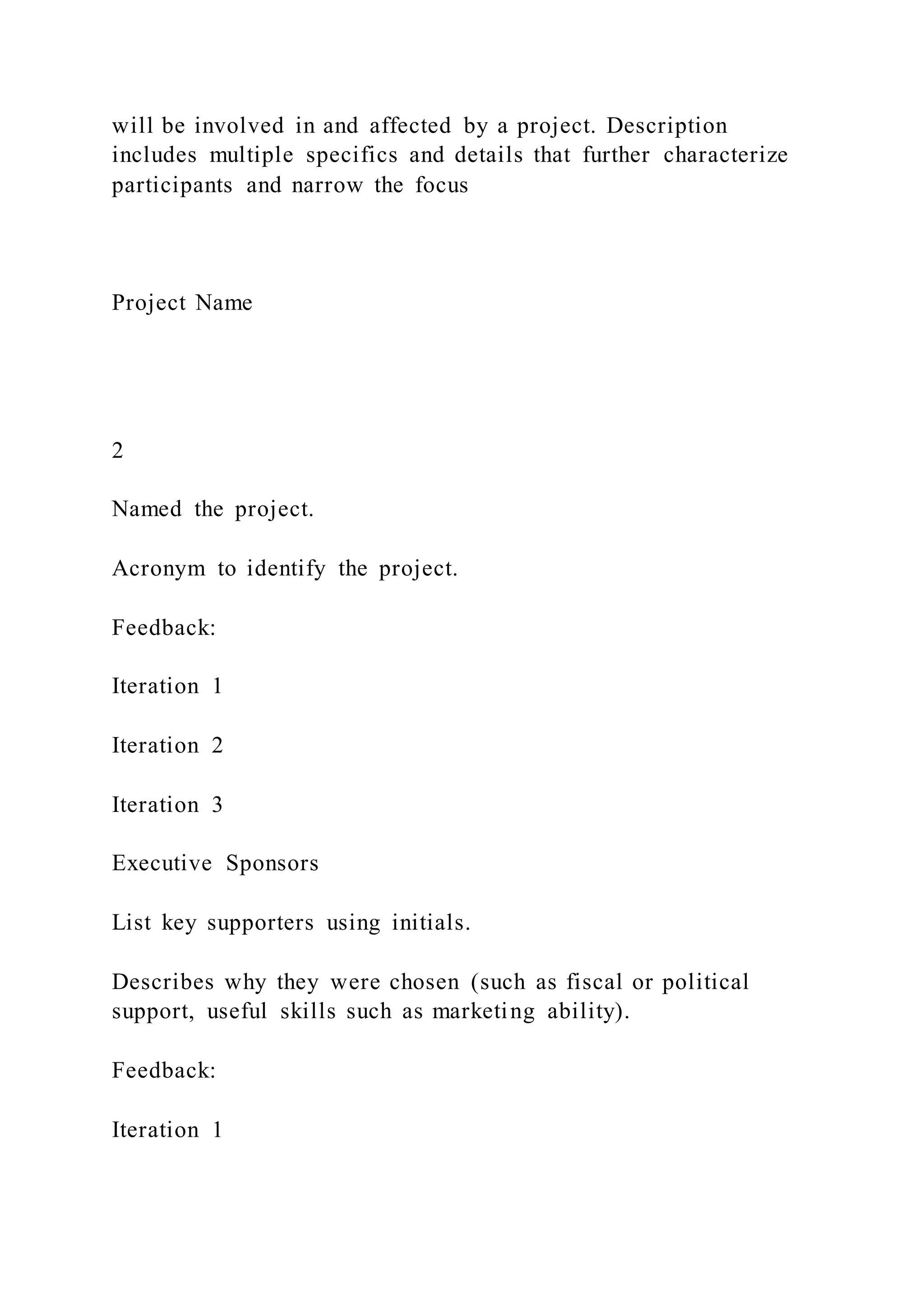
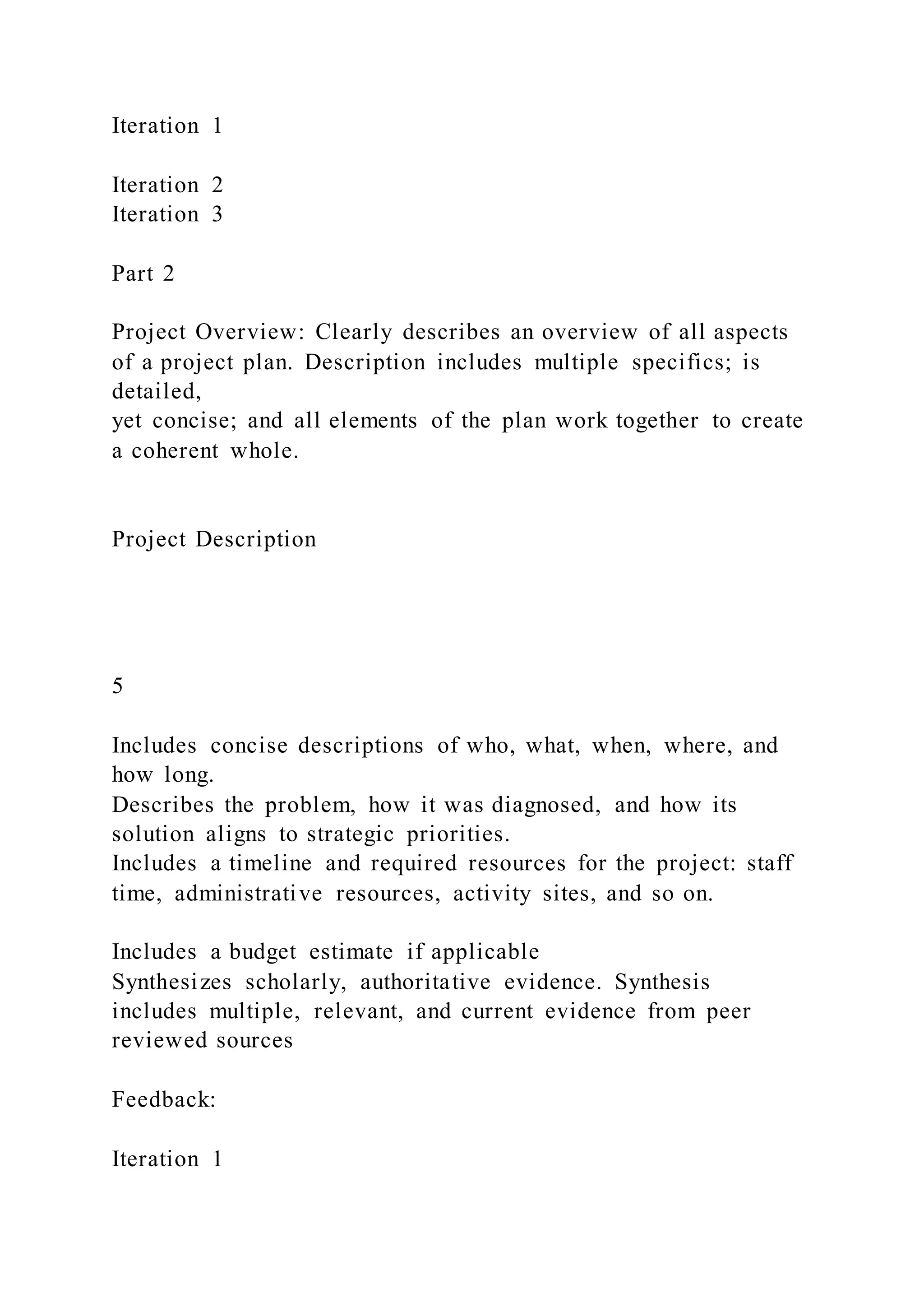
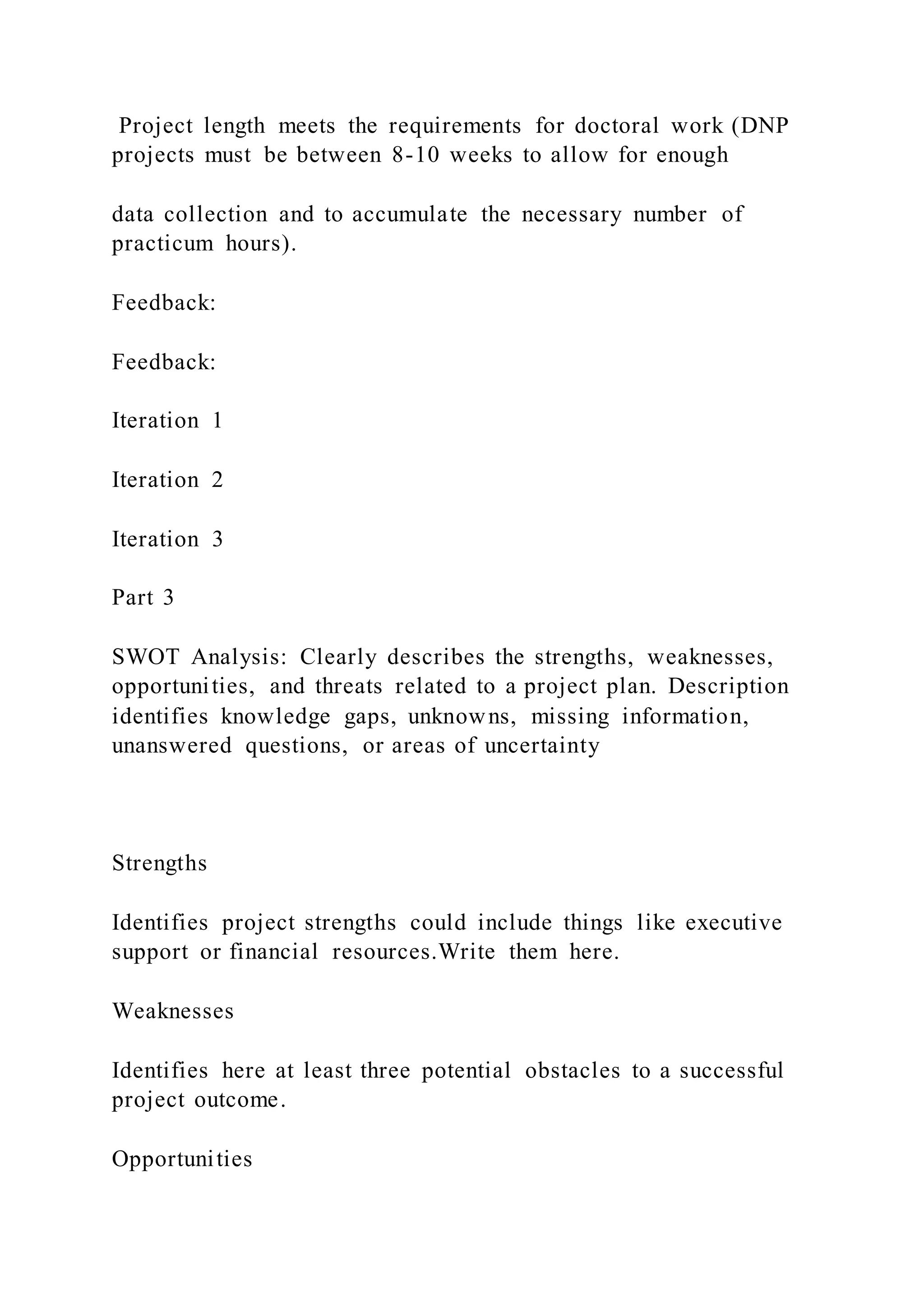
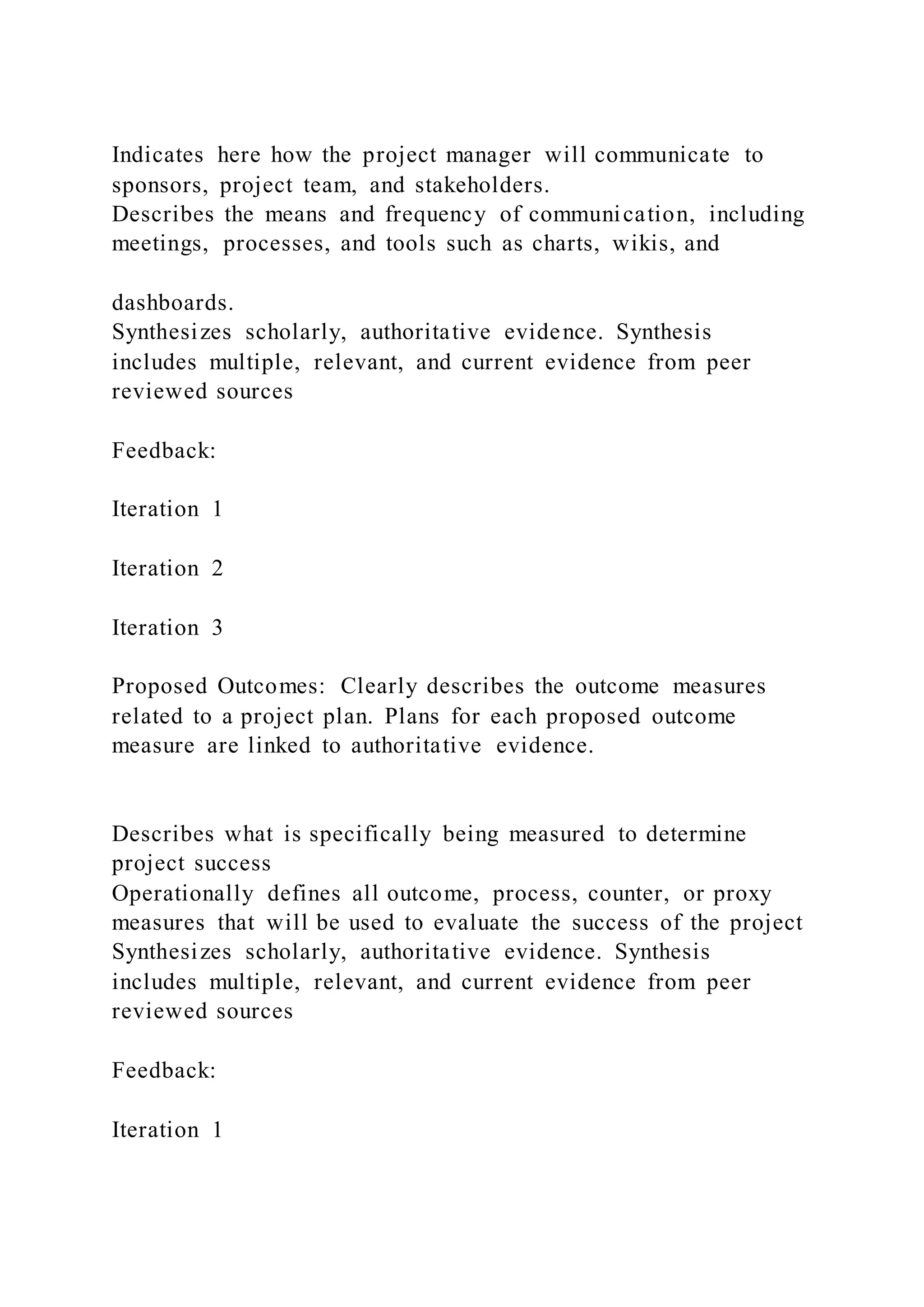
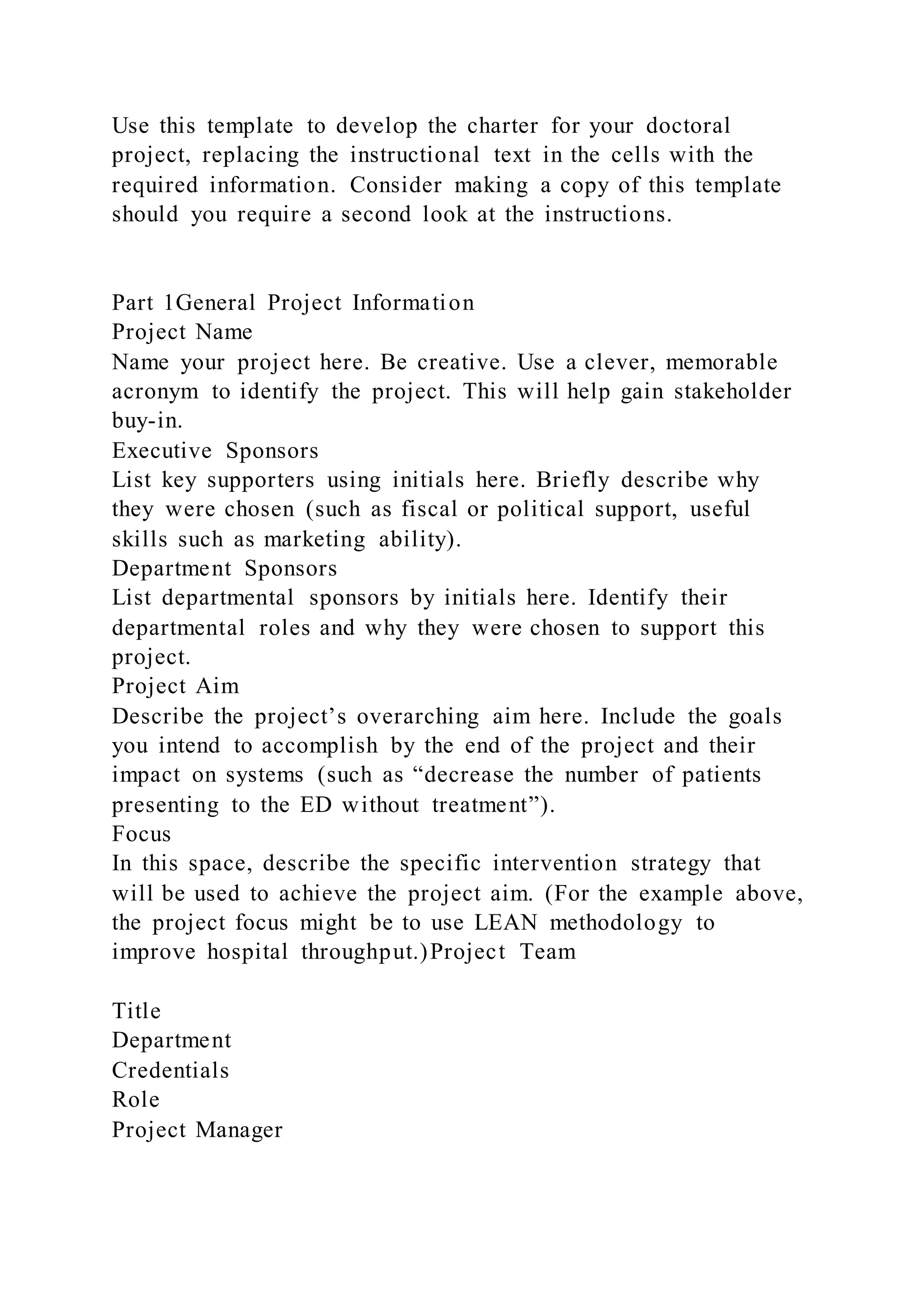
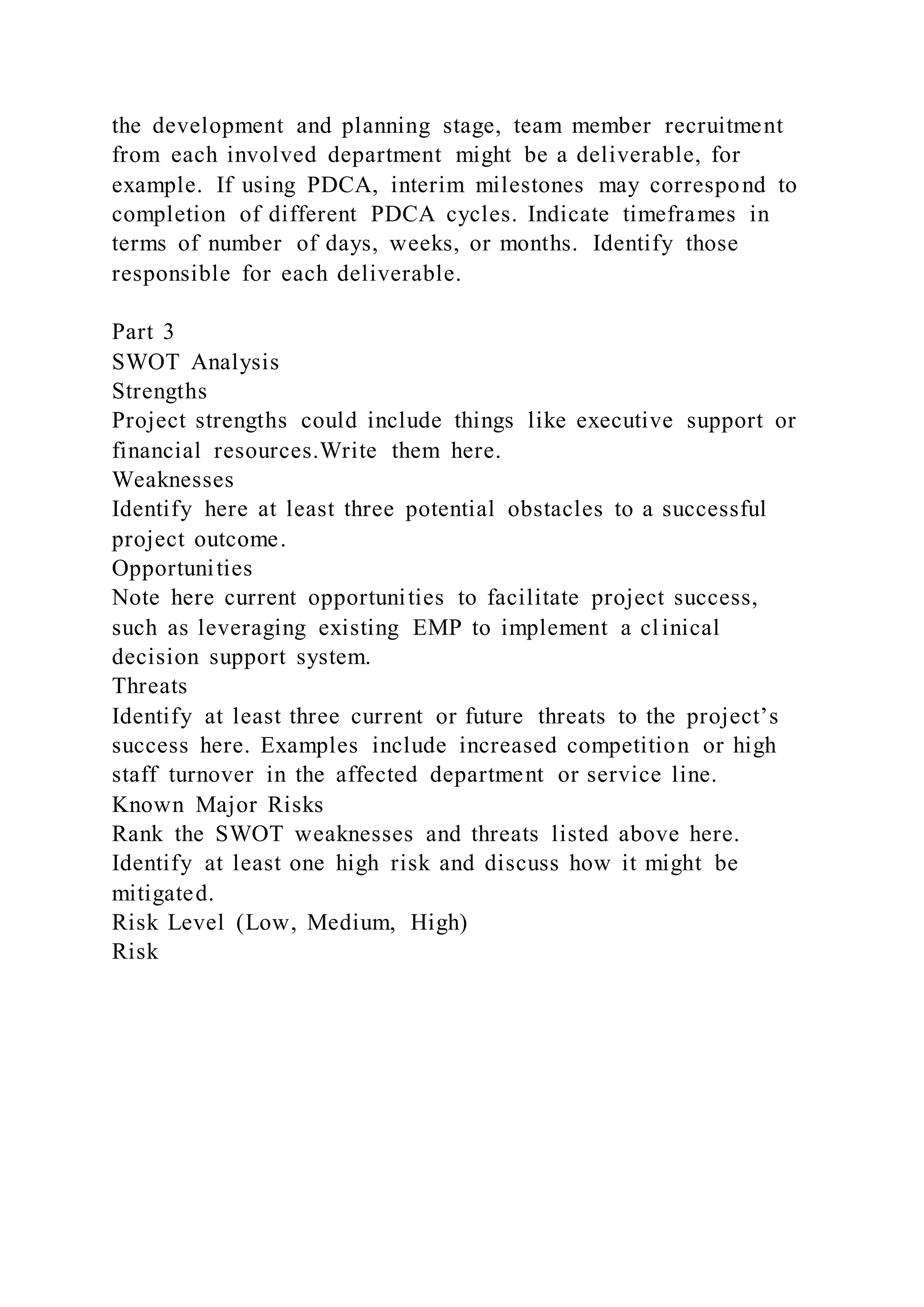
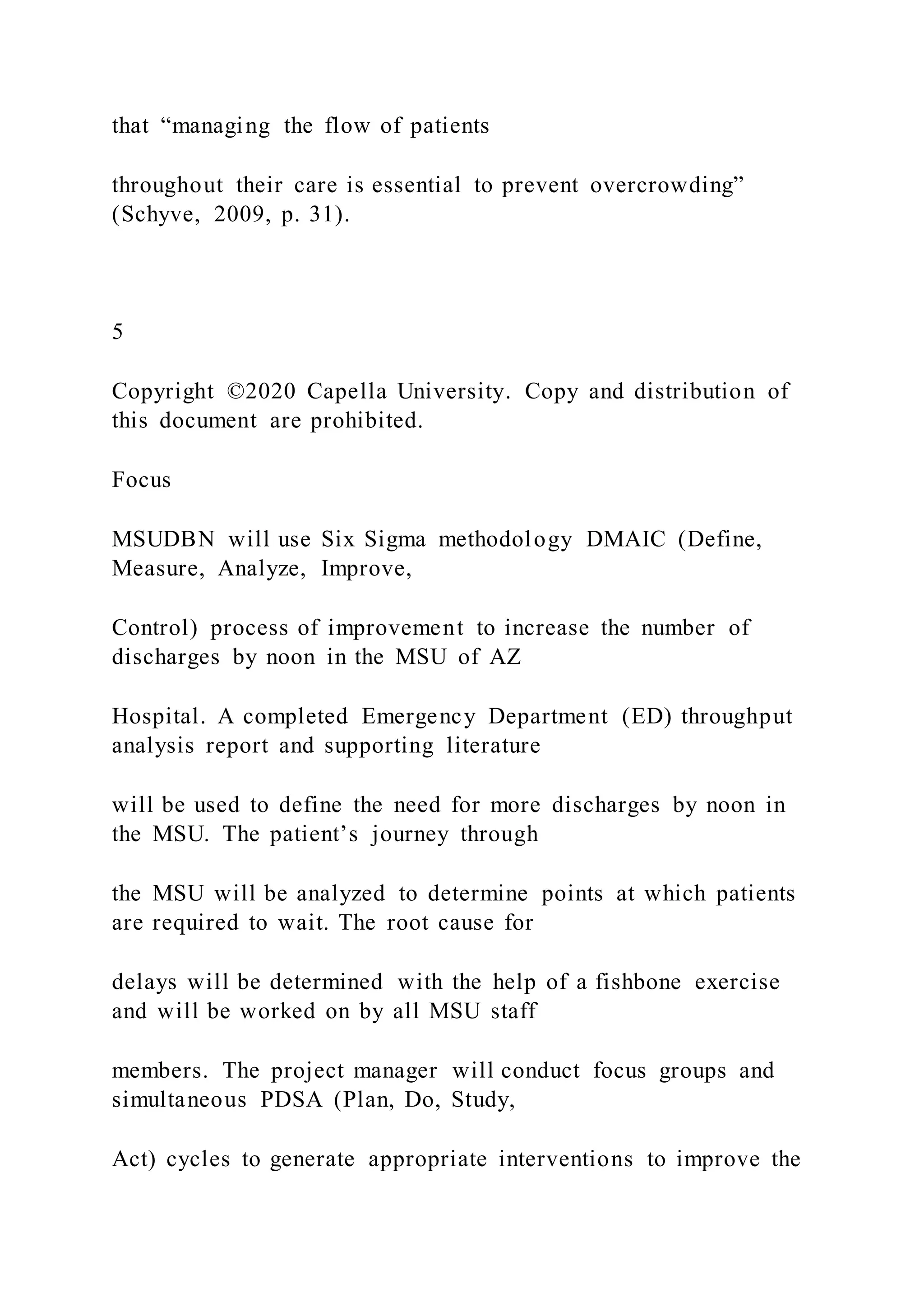
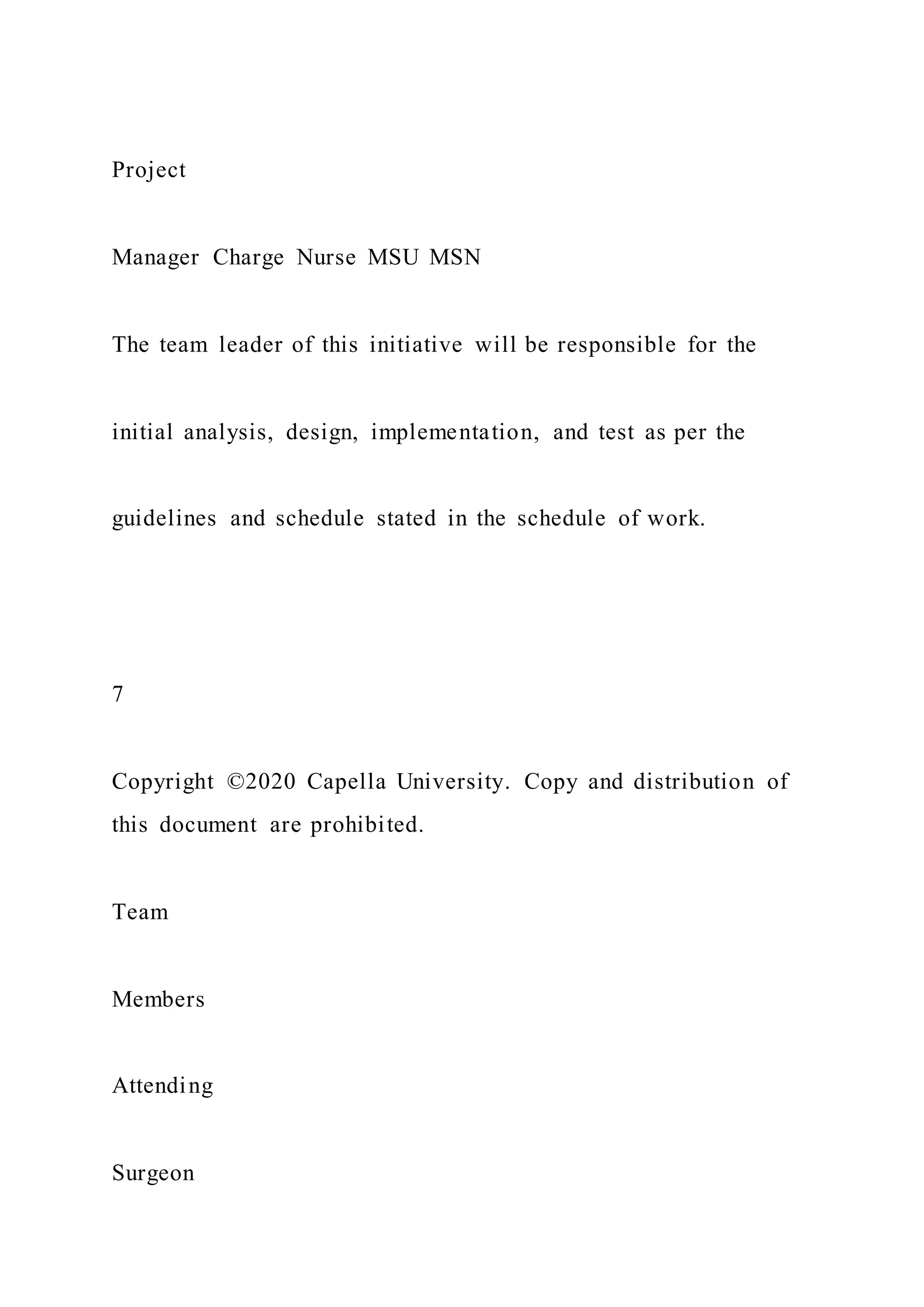
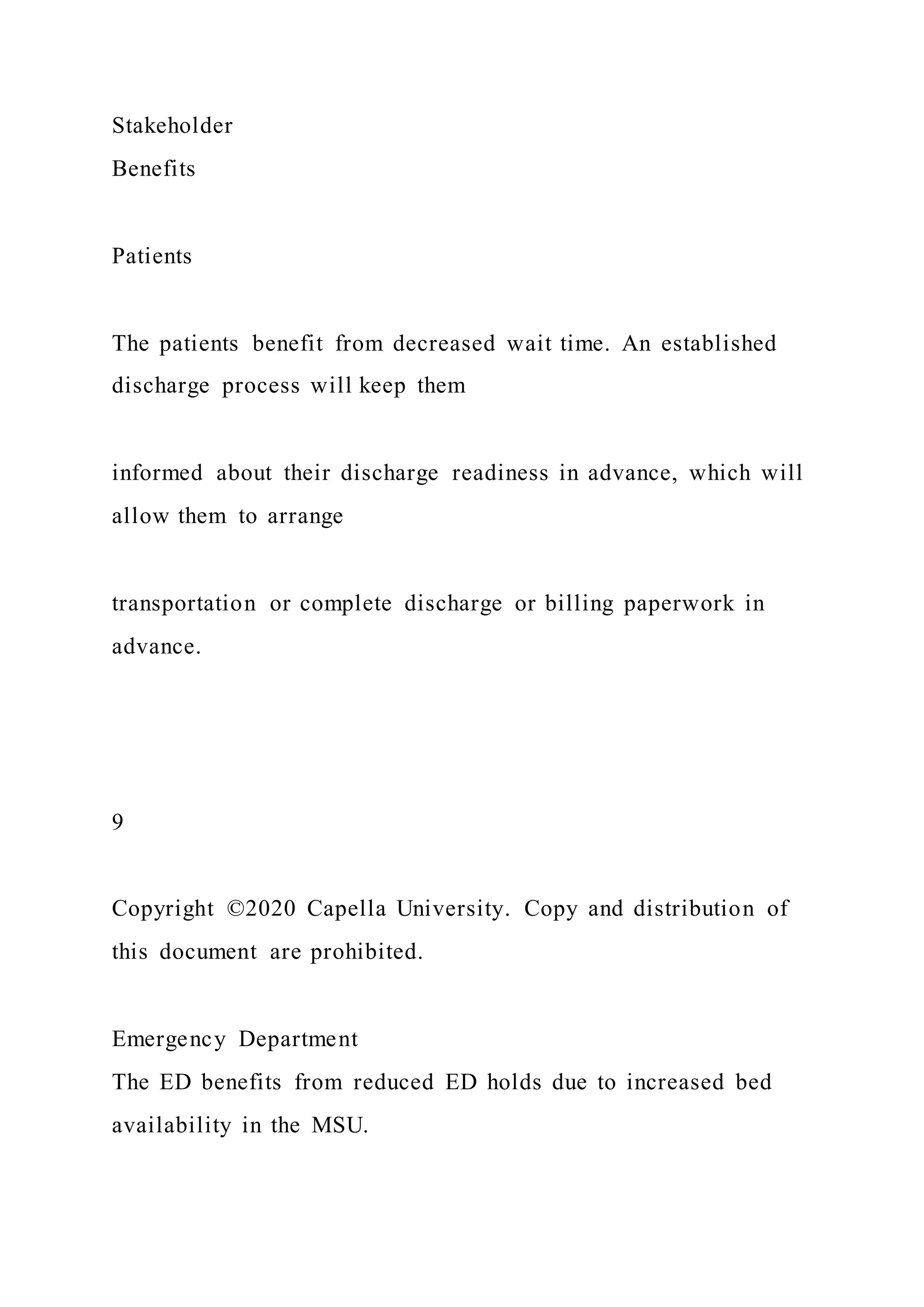
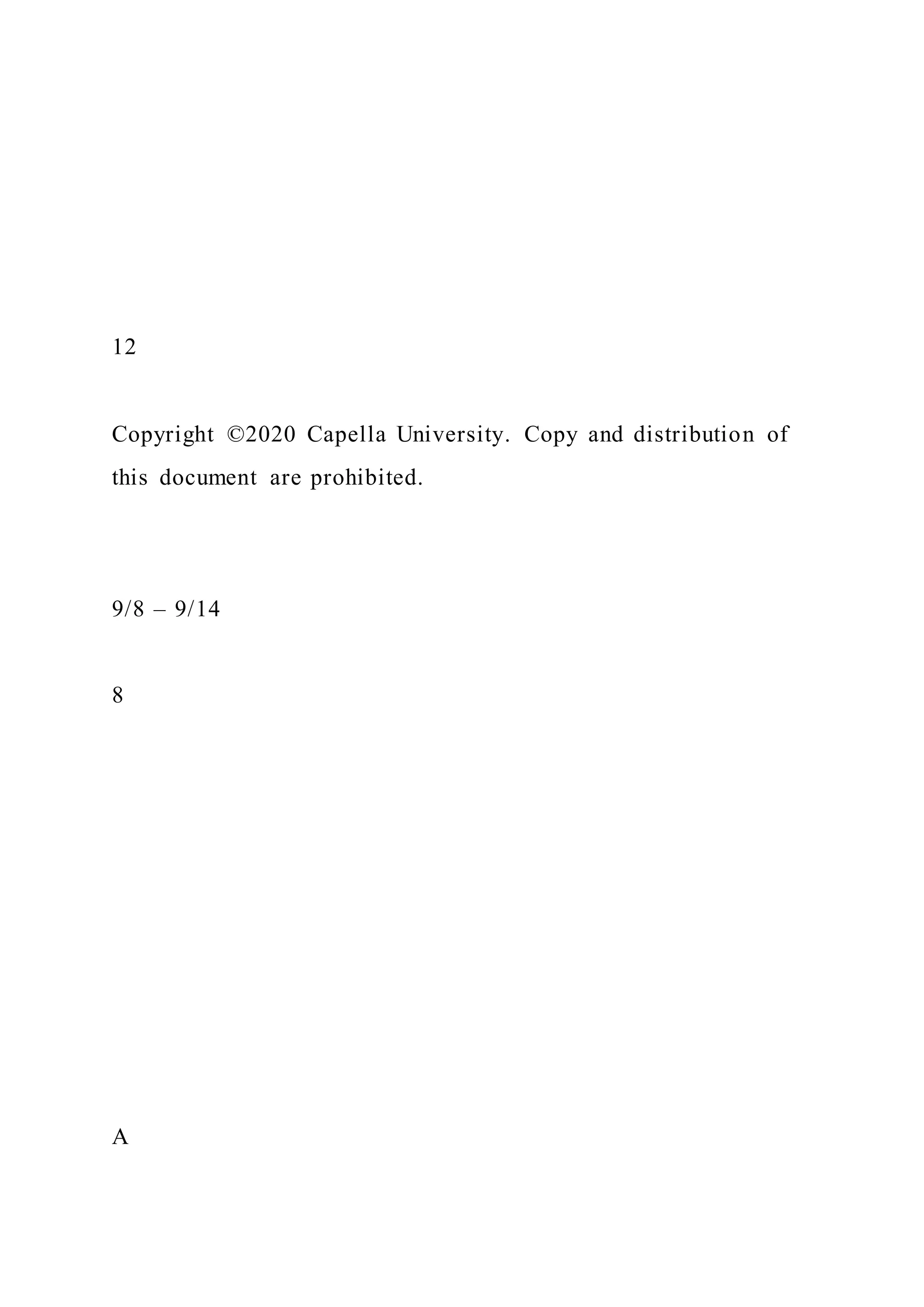
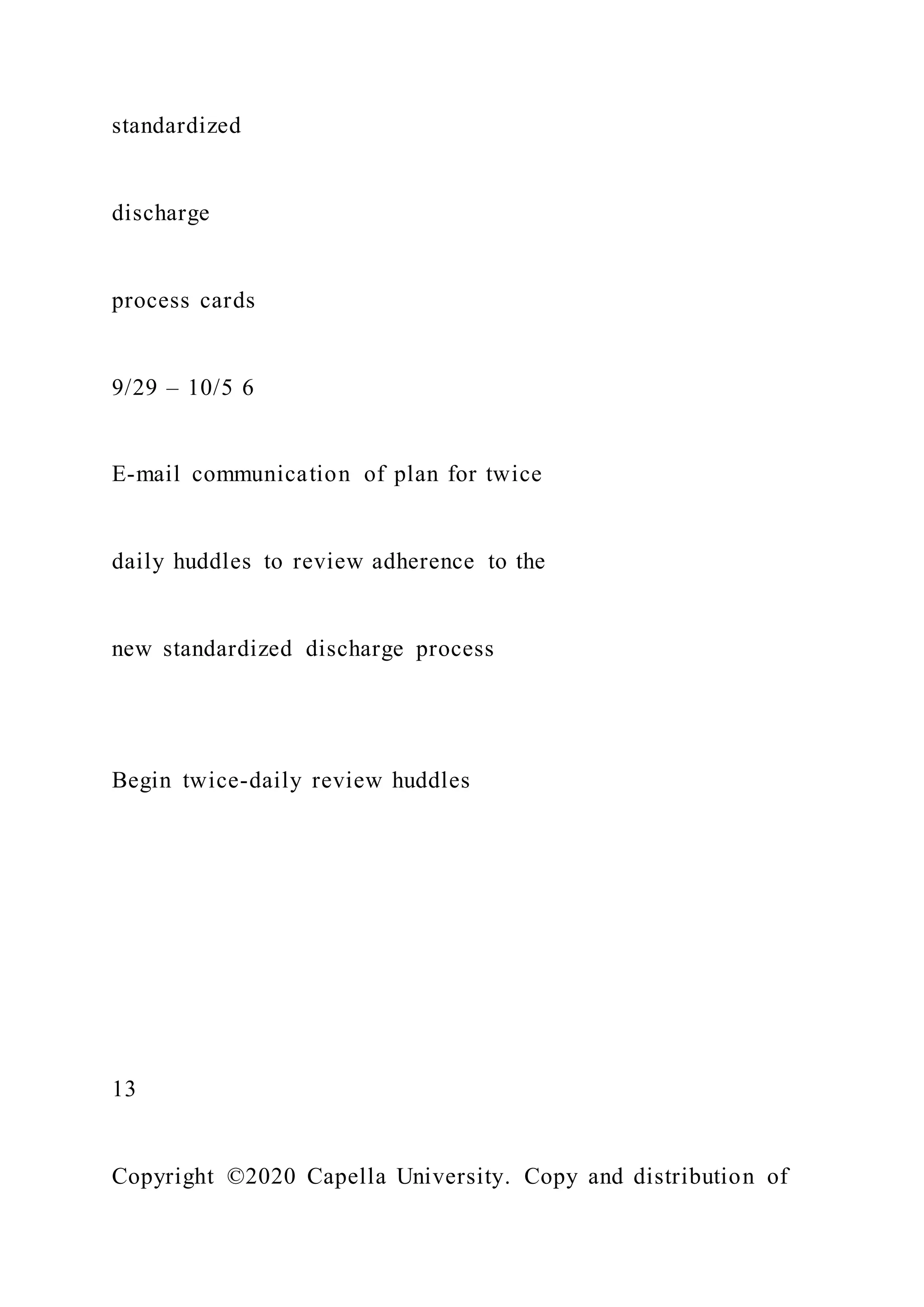
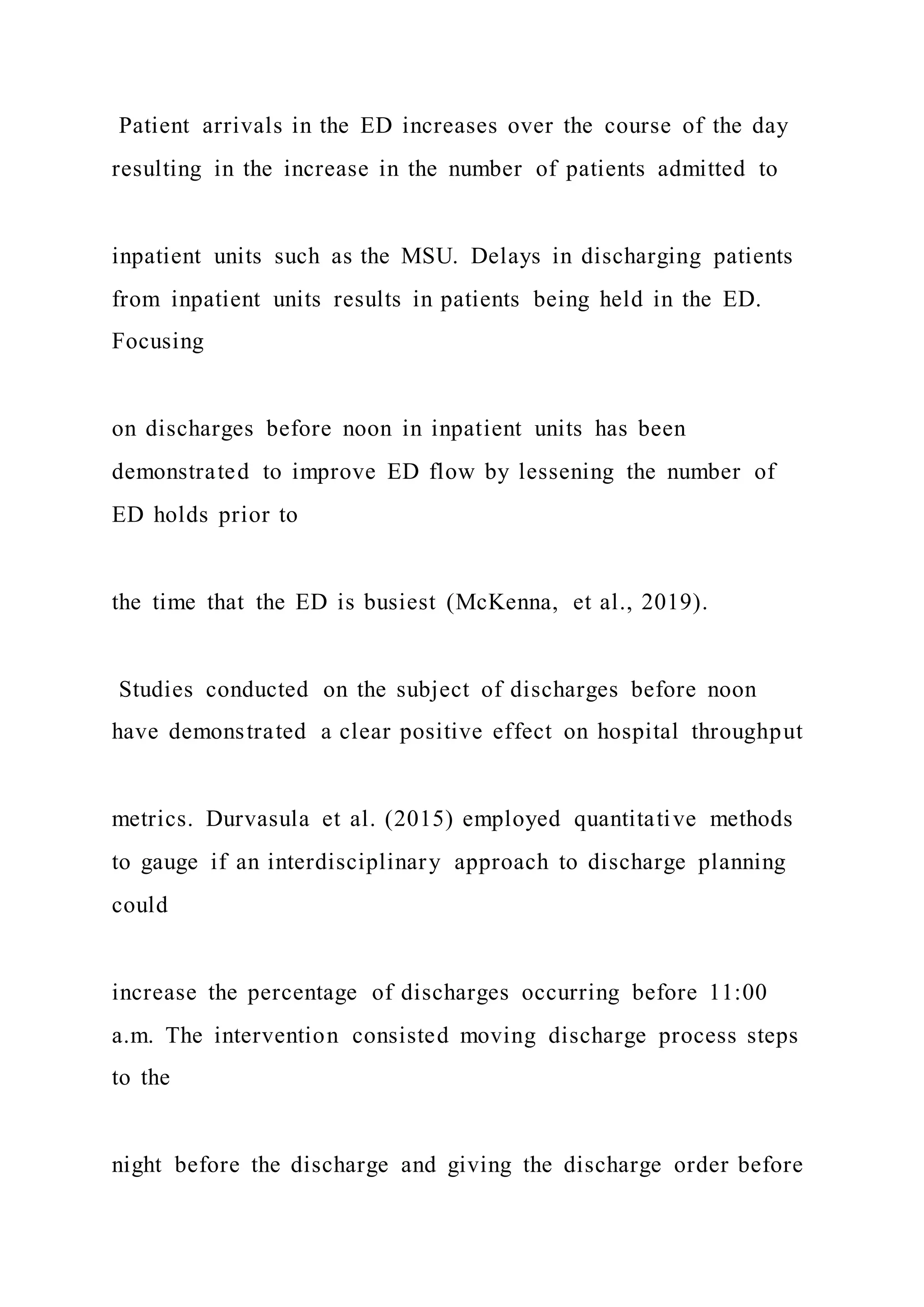
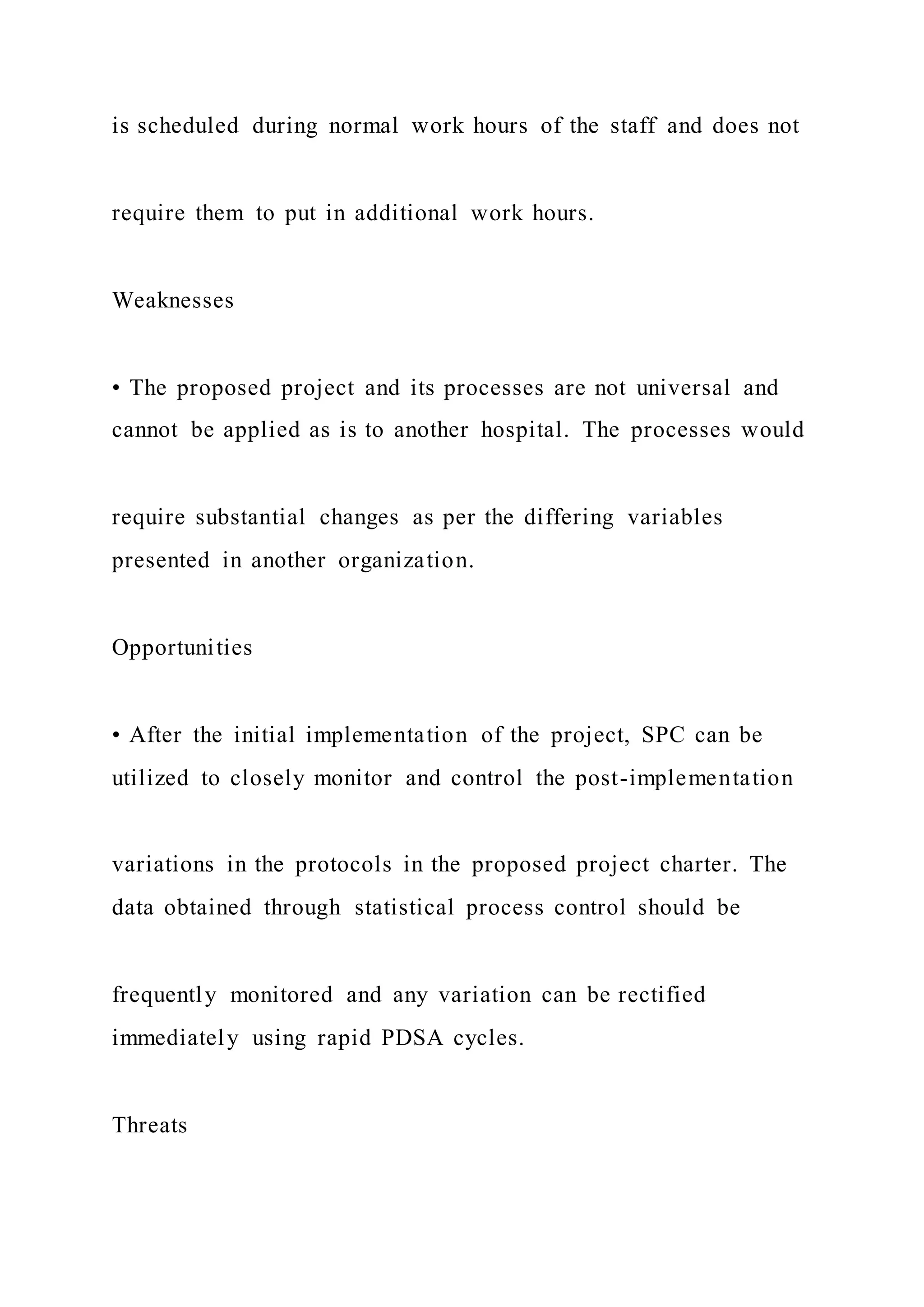
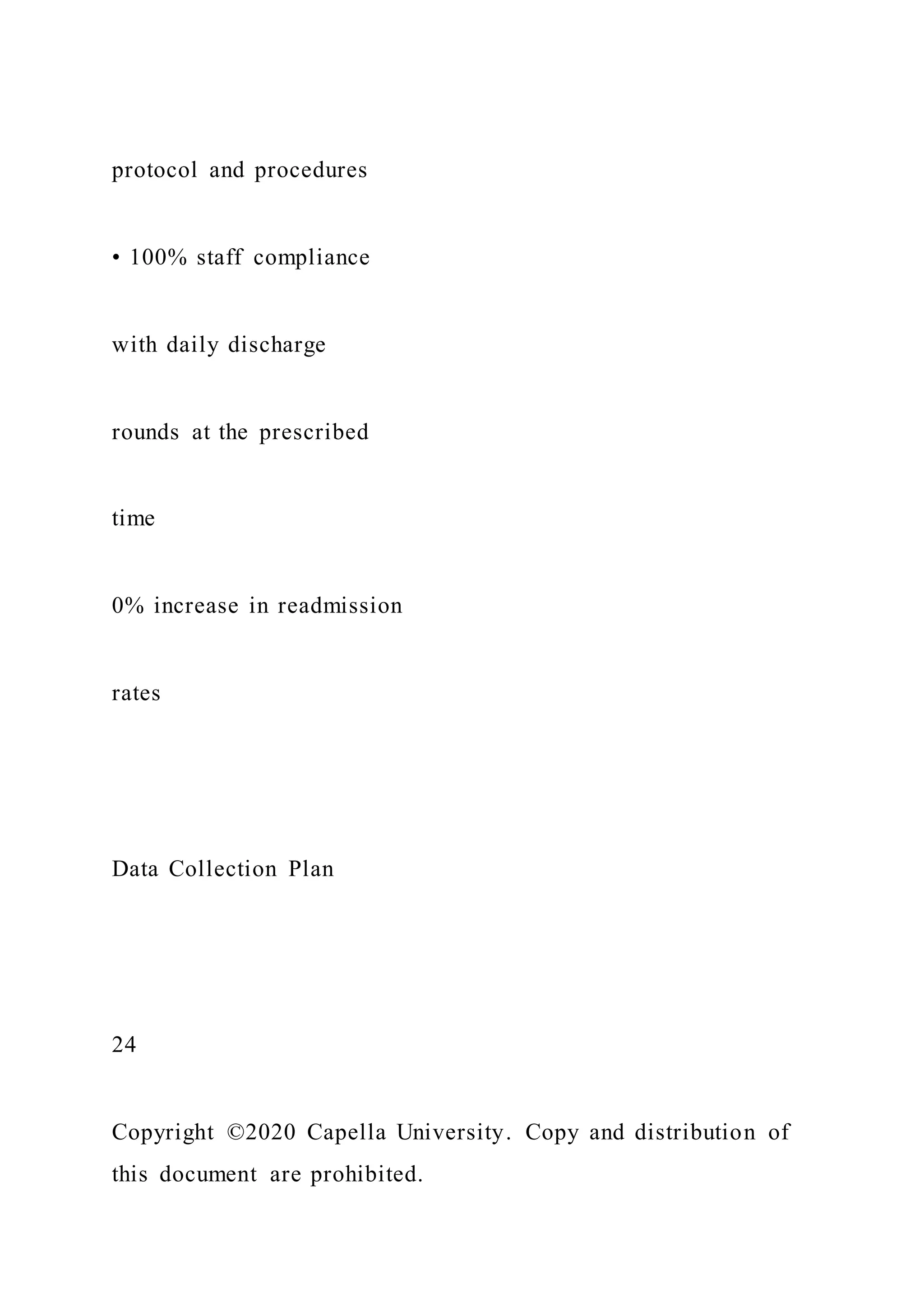
![Ethical Considerations
Taking into account PHI, HIPAA, human subject considerations,
equitable care, and IRB oversight, describe here any potential
for human rights violations. Note any vulnerable populations
involved and plans for equitable subject treatment. Describe
data security factors: how data will be accessed and stored,
including team members who will have access to personal
health data and how it will be safeguarded (such as “Only [X]
people will access the EMR”).
Constraints
List here any limits to personnel, funding, scheduling, or other
options, such as a predetermined budget, limited staff, or
deadline.
External Dependencies
If the project’s success may depend on external relationships or
resources such as personnel, funding, communication channels,
or community resources, describe them here. If there are no
external dependencies, describe internal support.](https://image.slidesharecdn.com/1doctoralprojectcharterproposalchecklistinstruct-220920053858-baf1555b/75/1-Doctoral-Project-Charter-Proposal-Checklist-Instruct-55-2048.jpg)
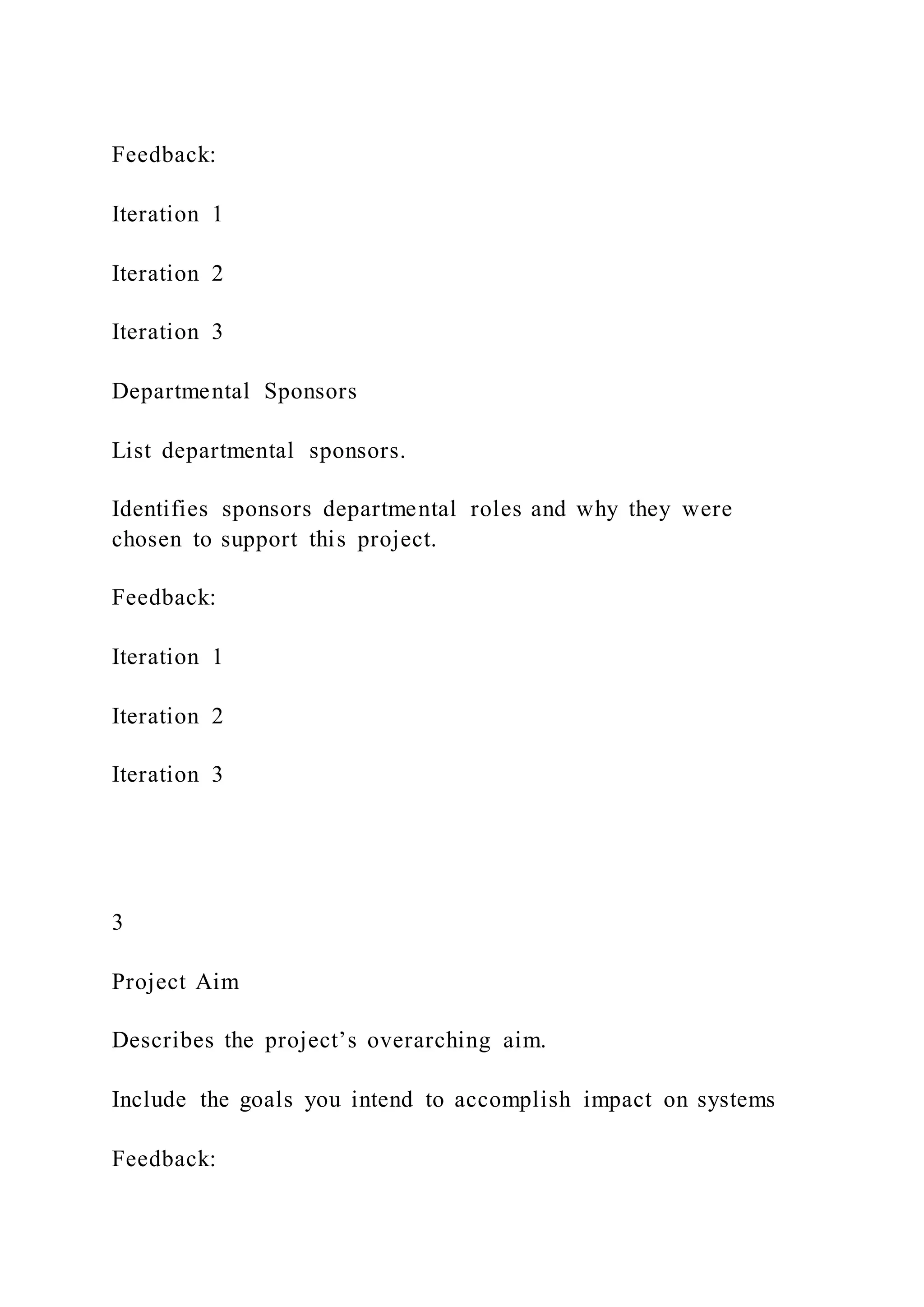
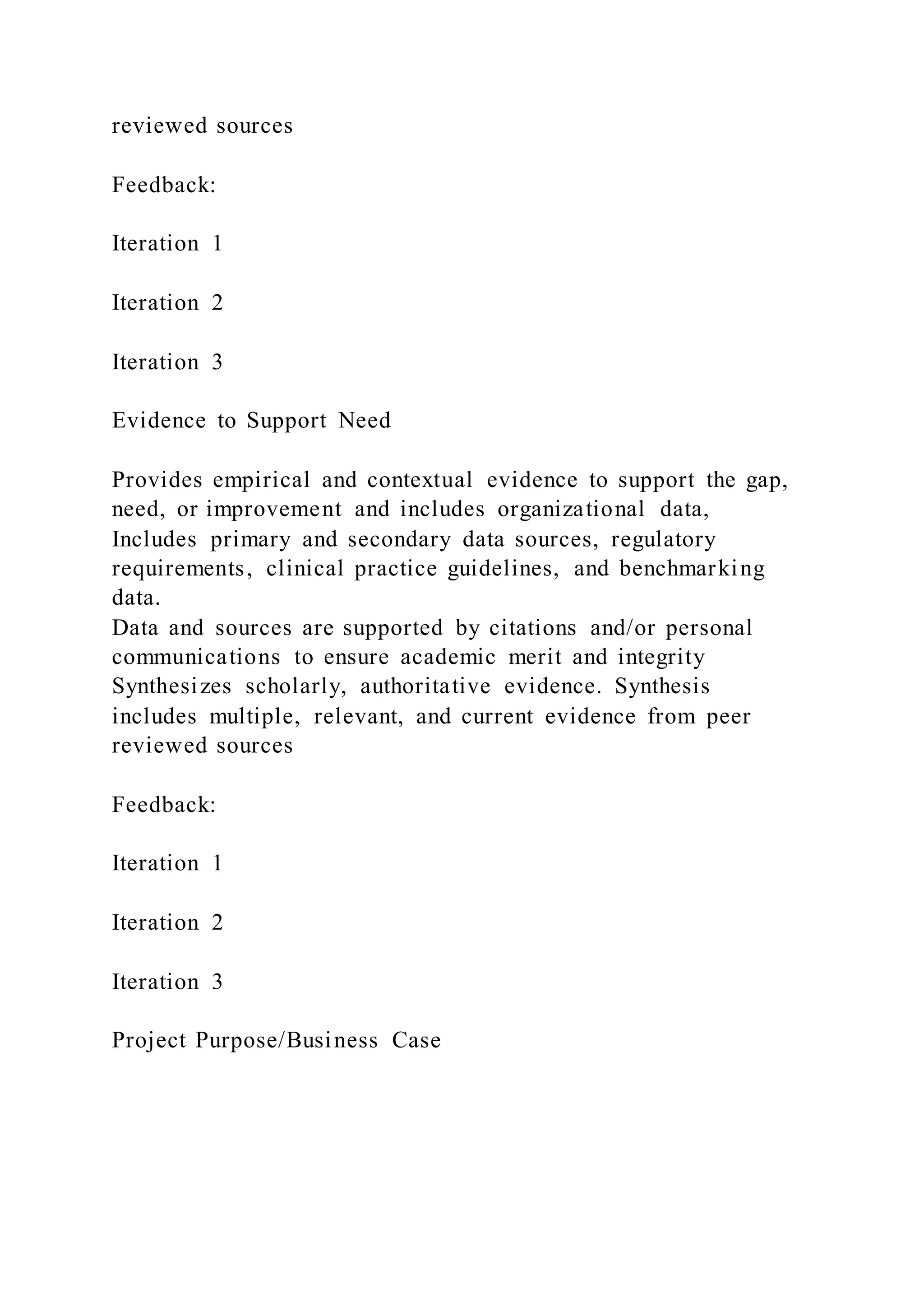
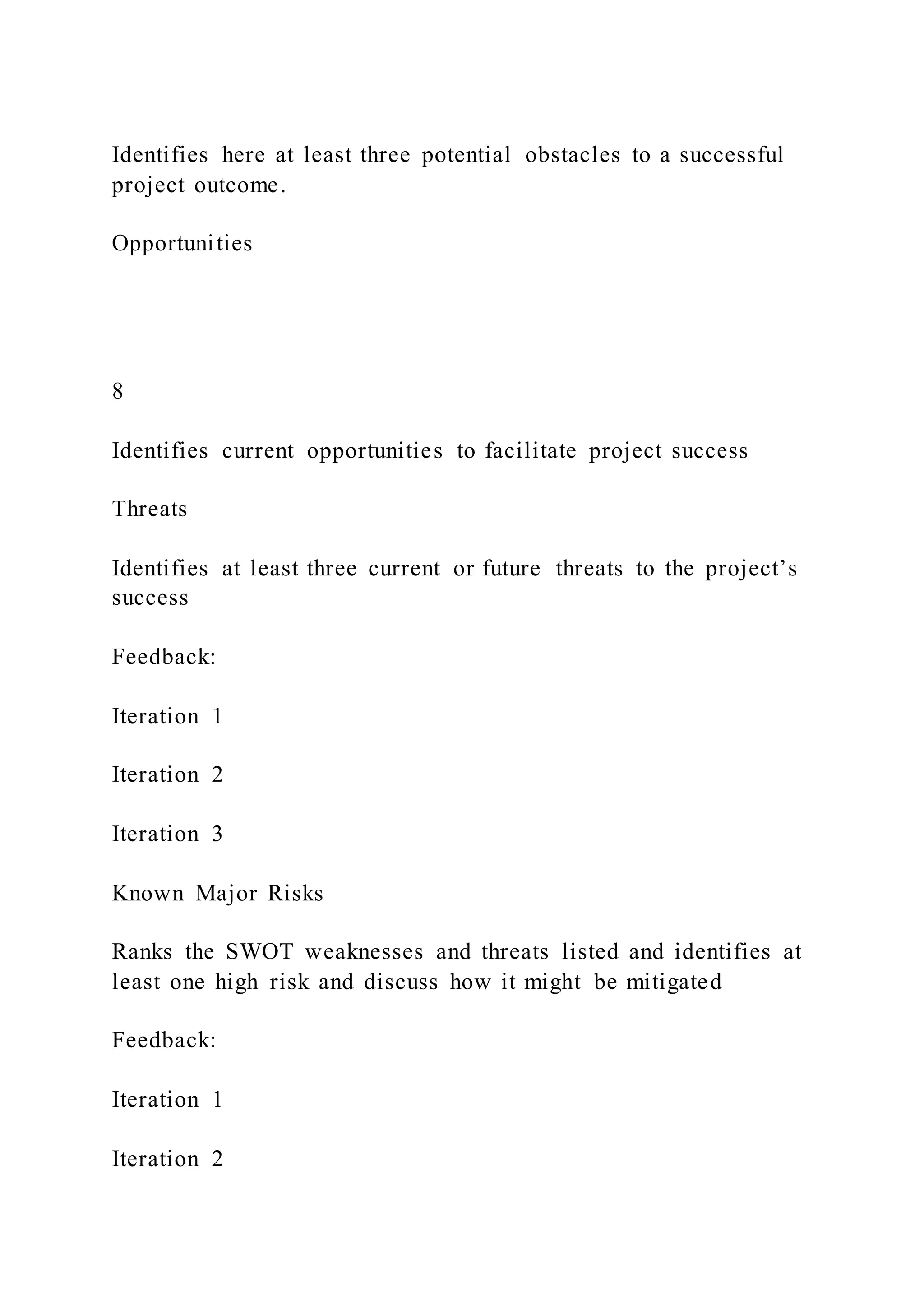
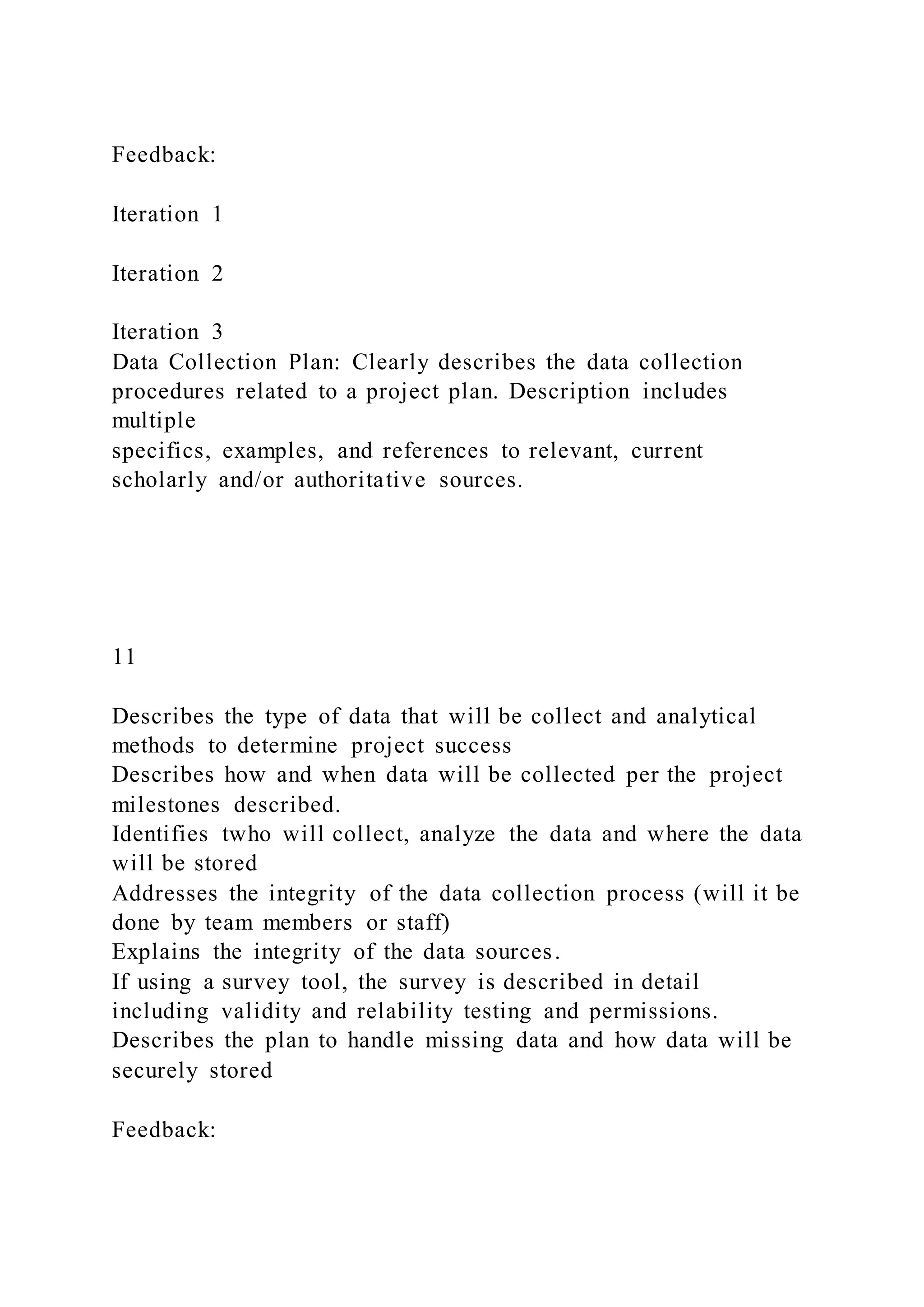
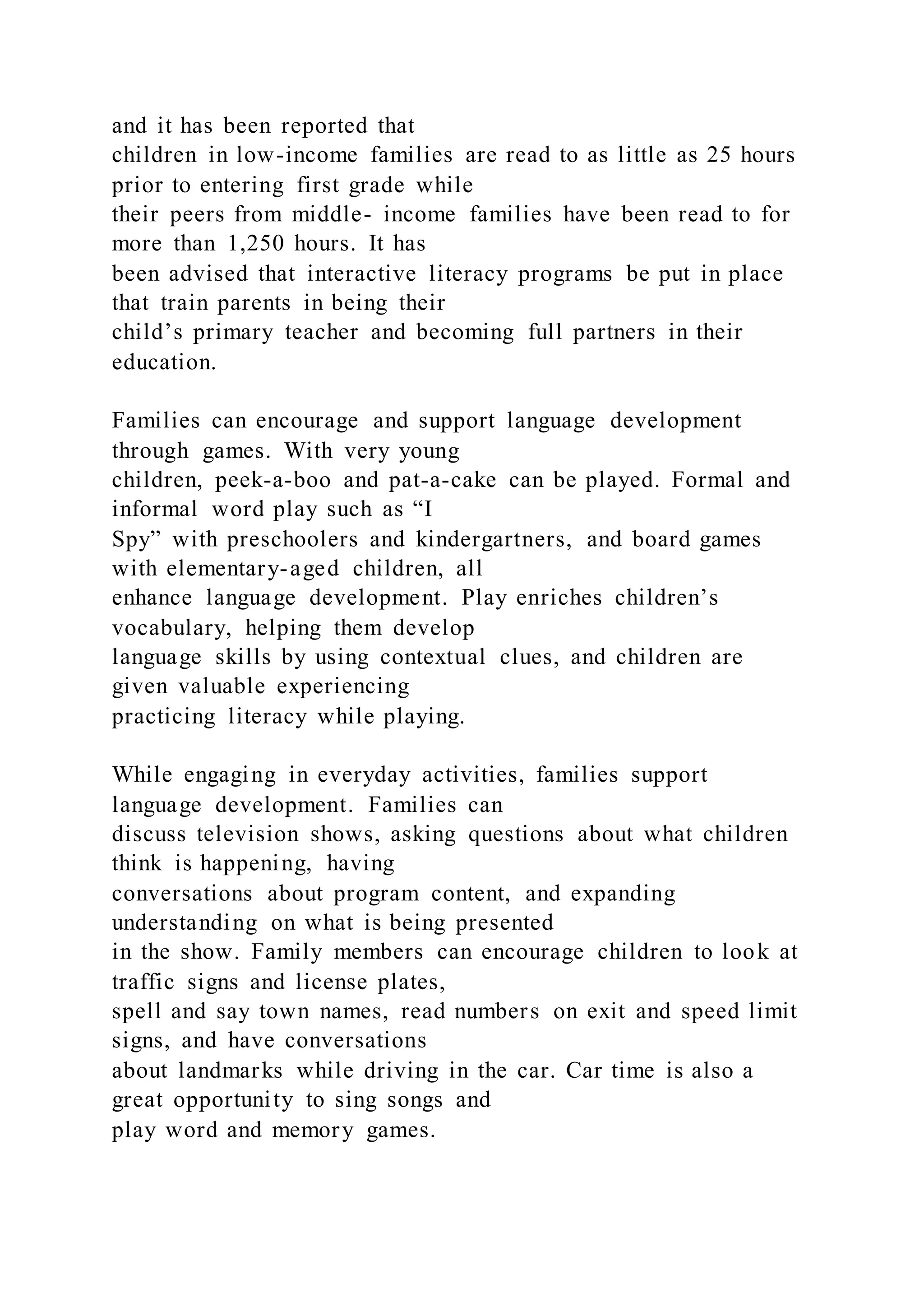
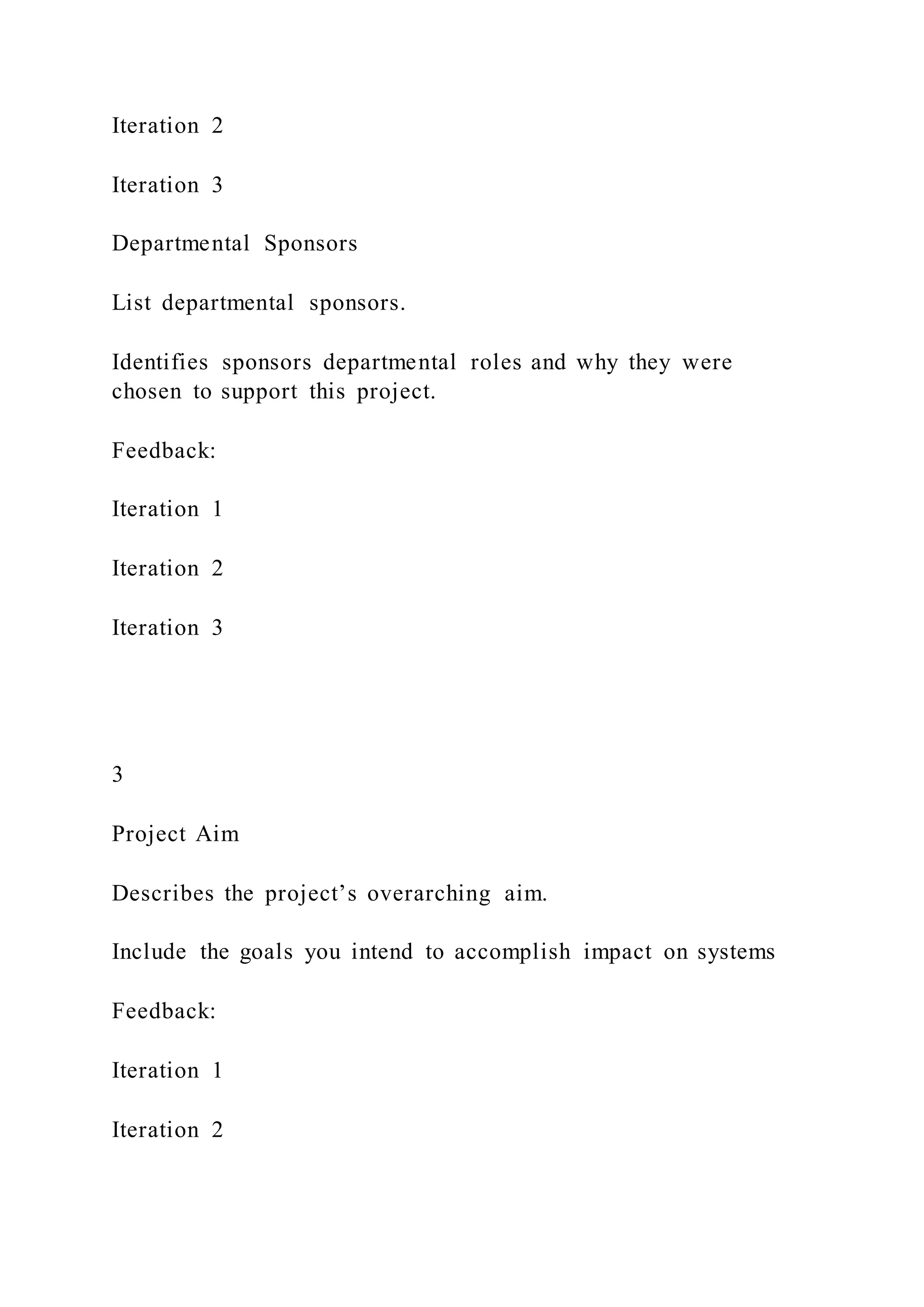
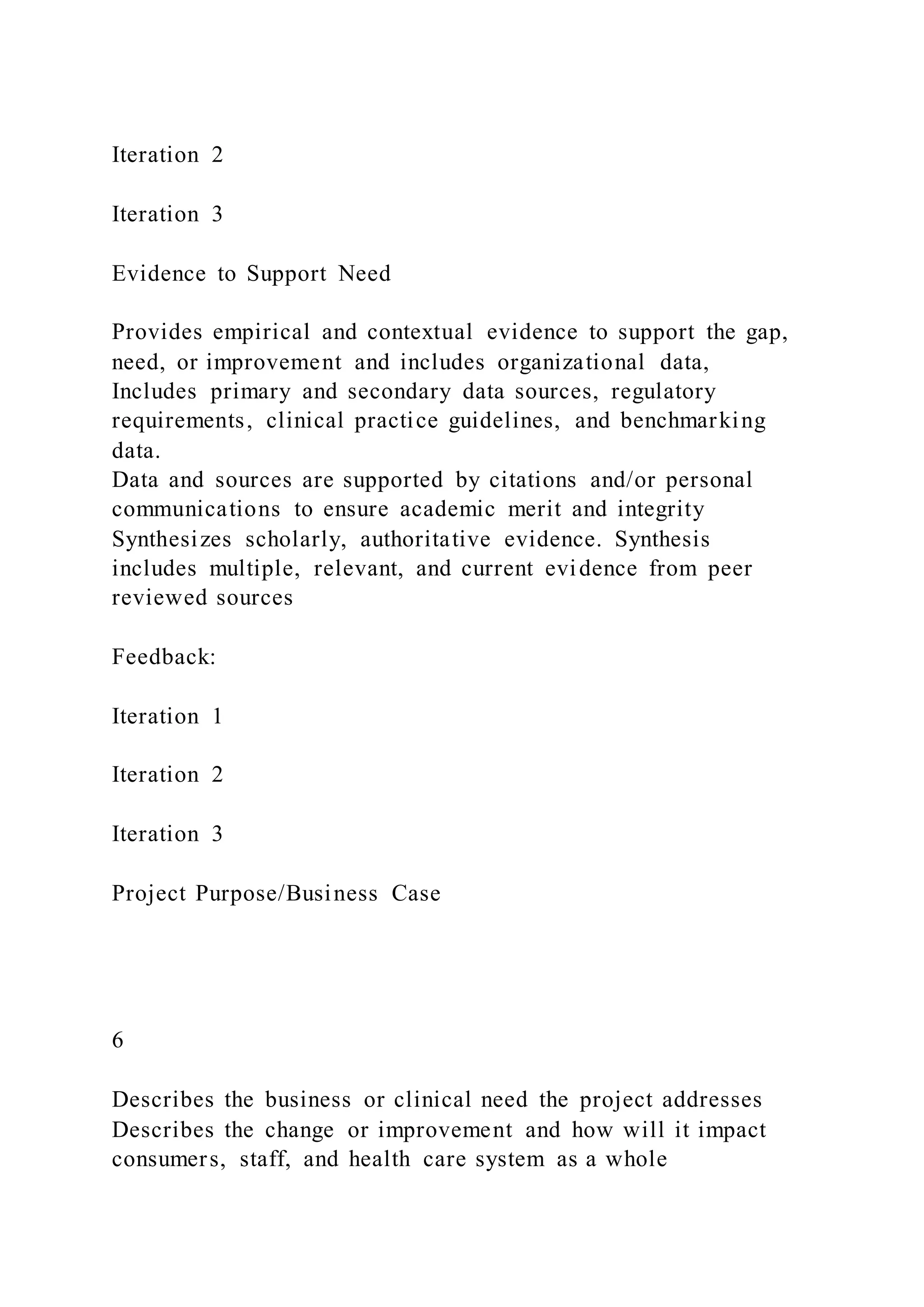
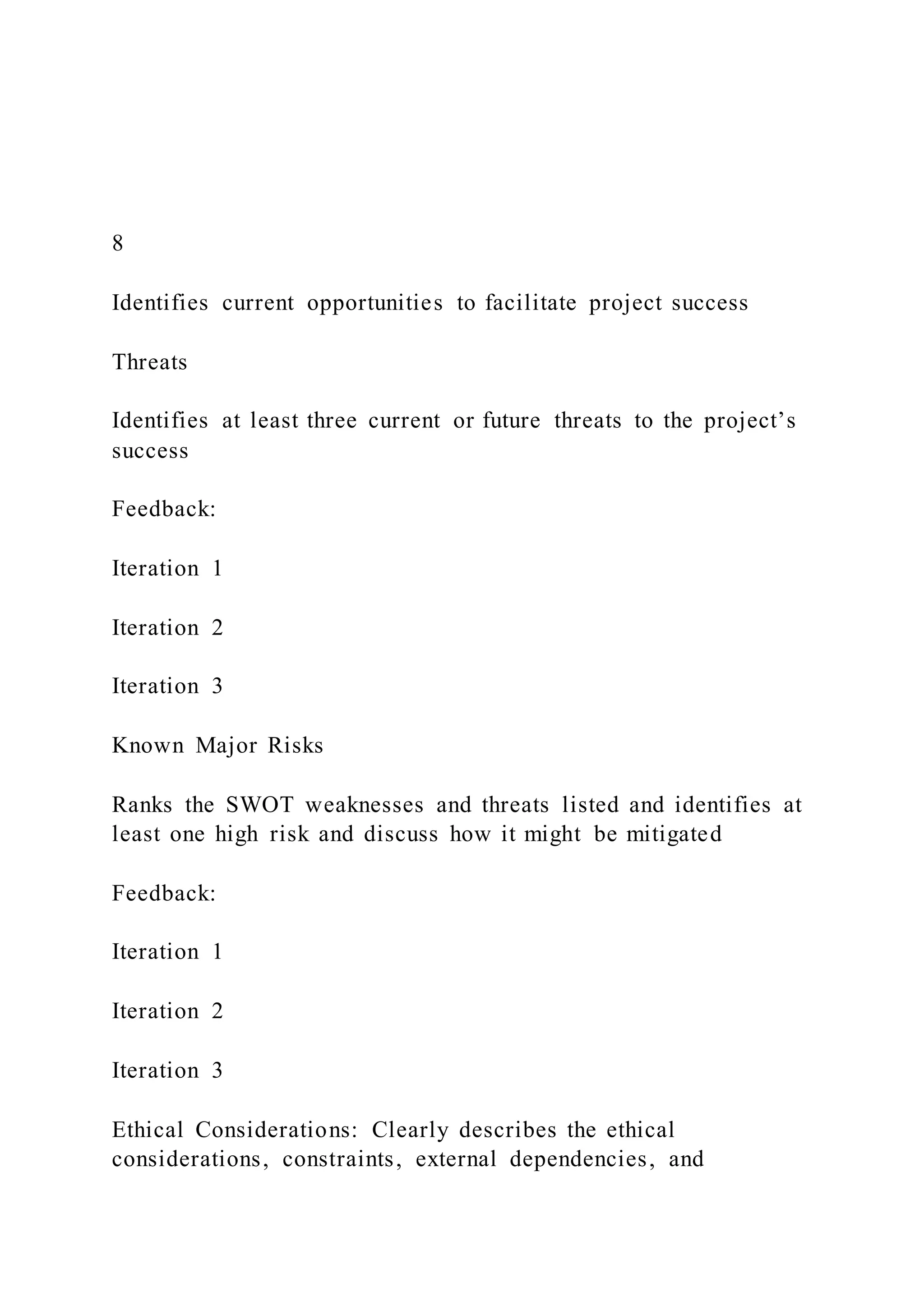
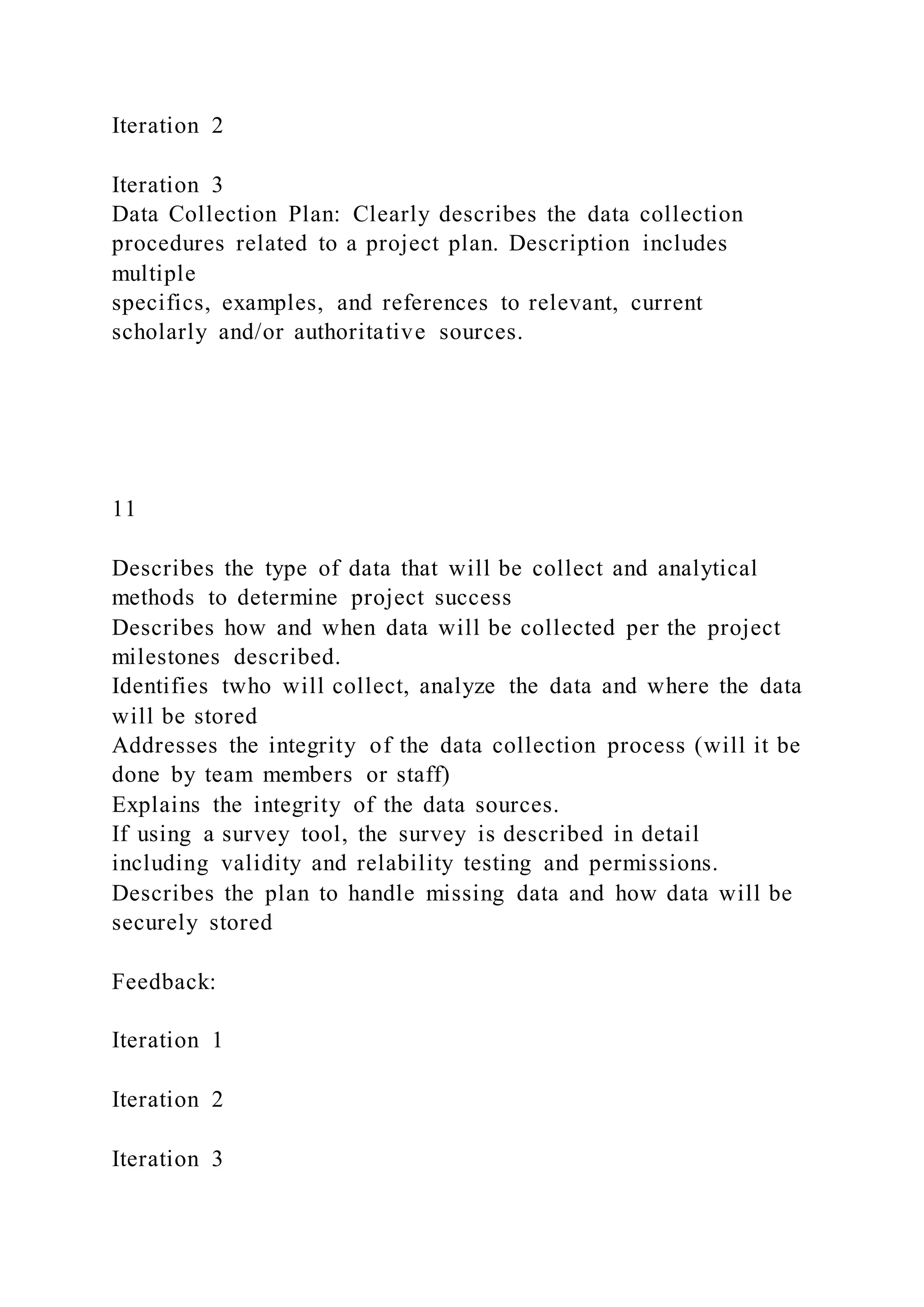
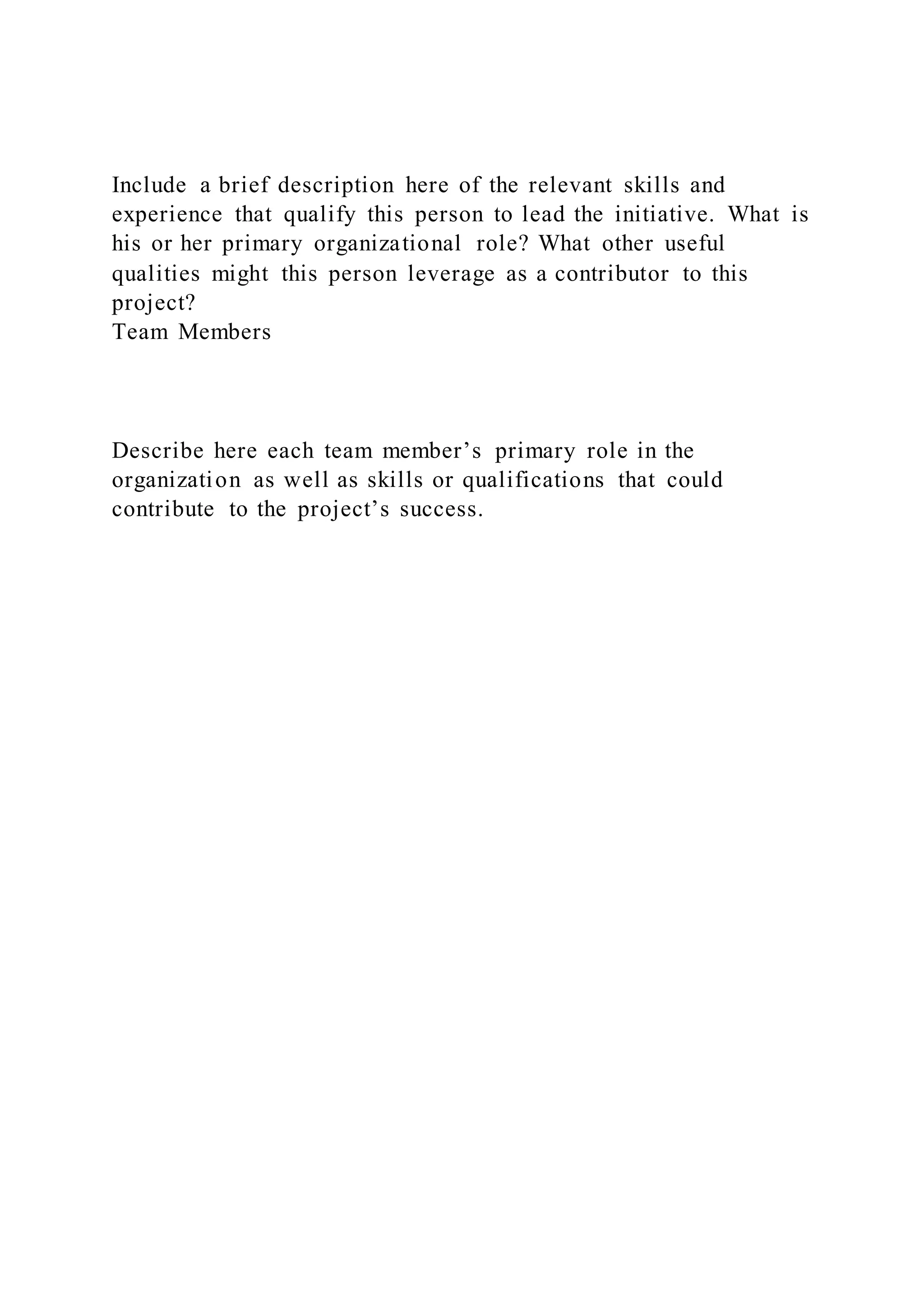
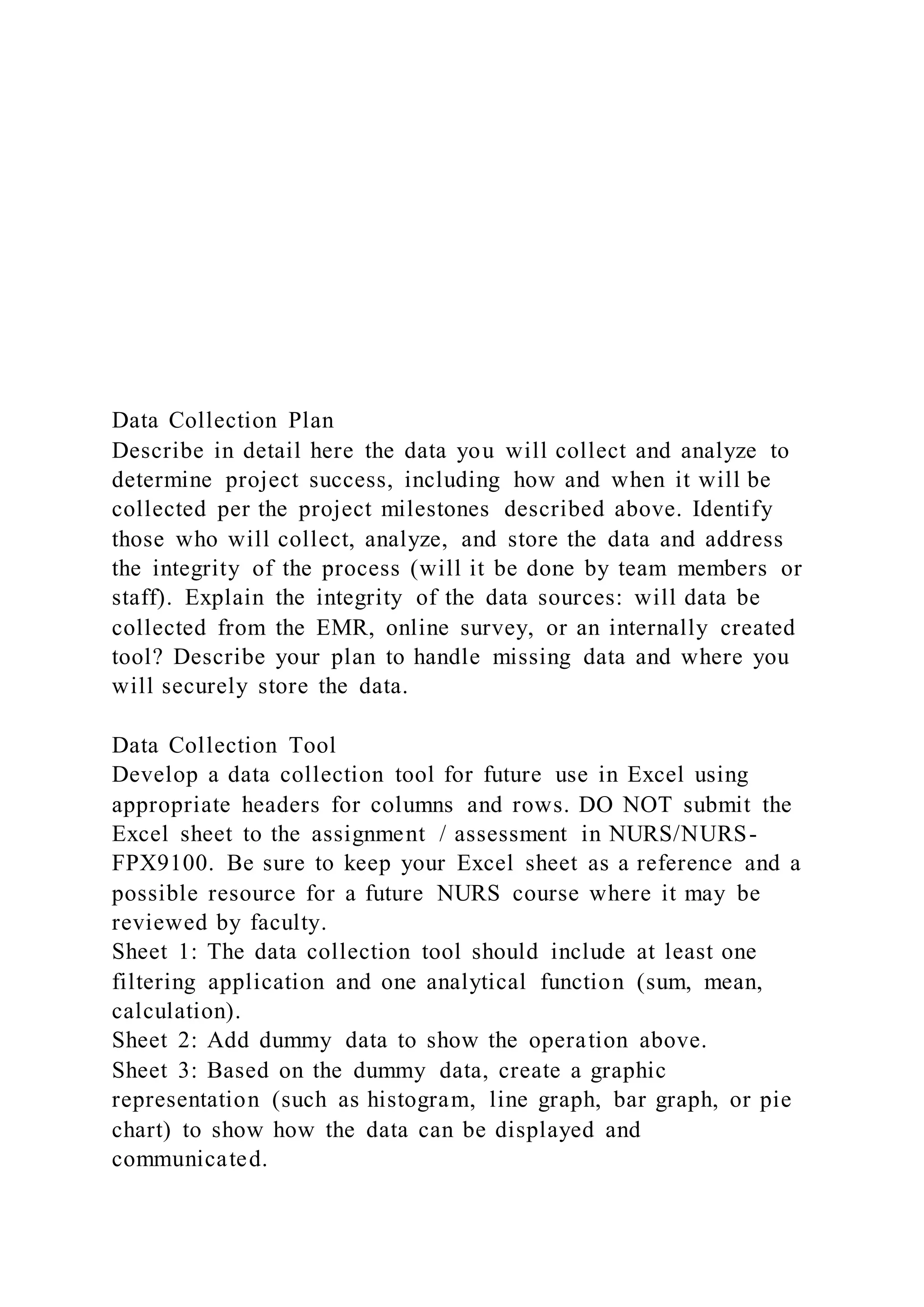
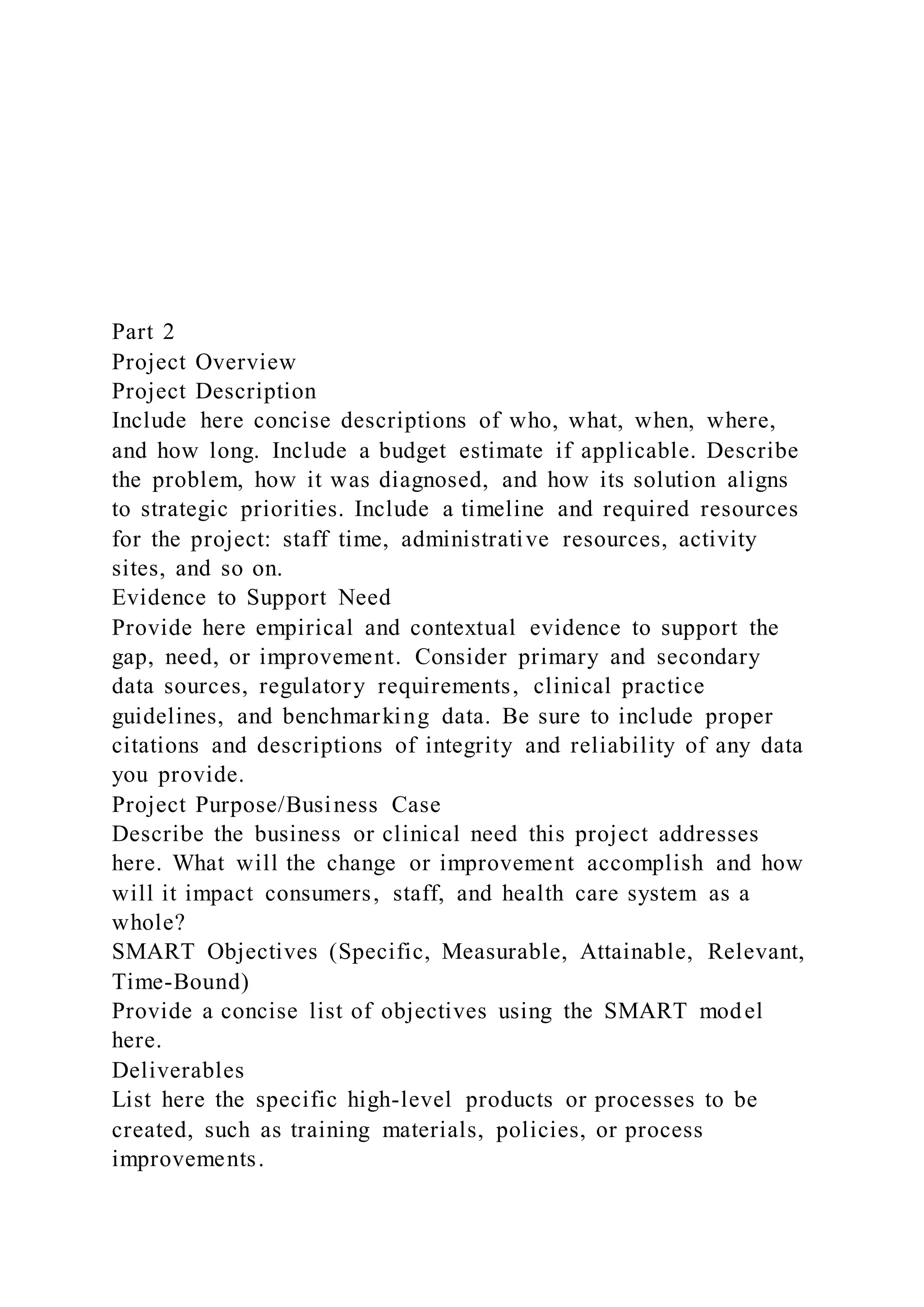
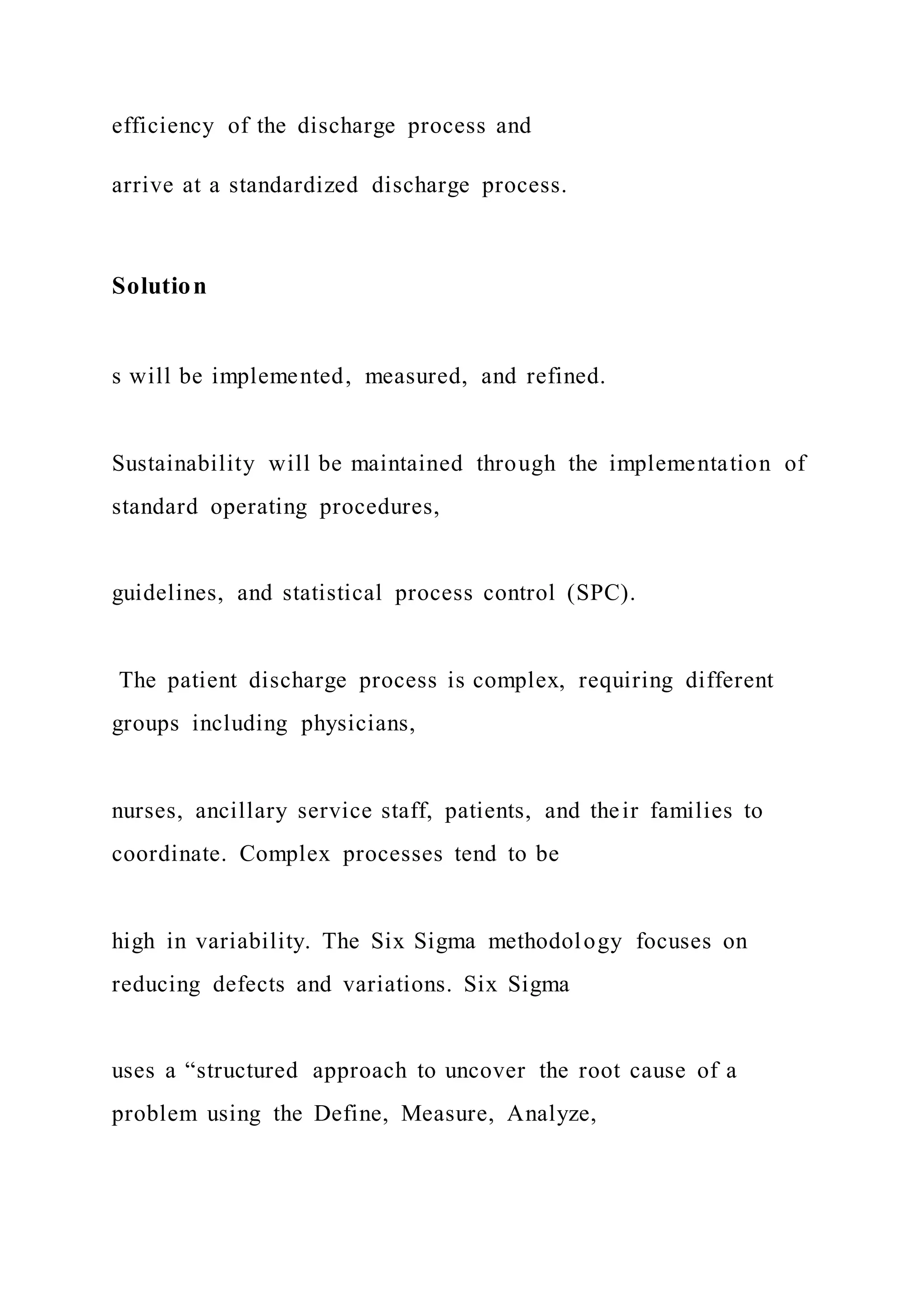
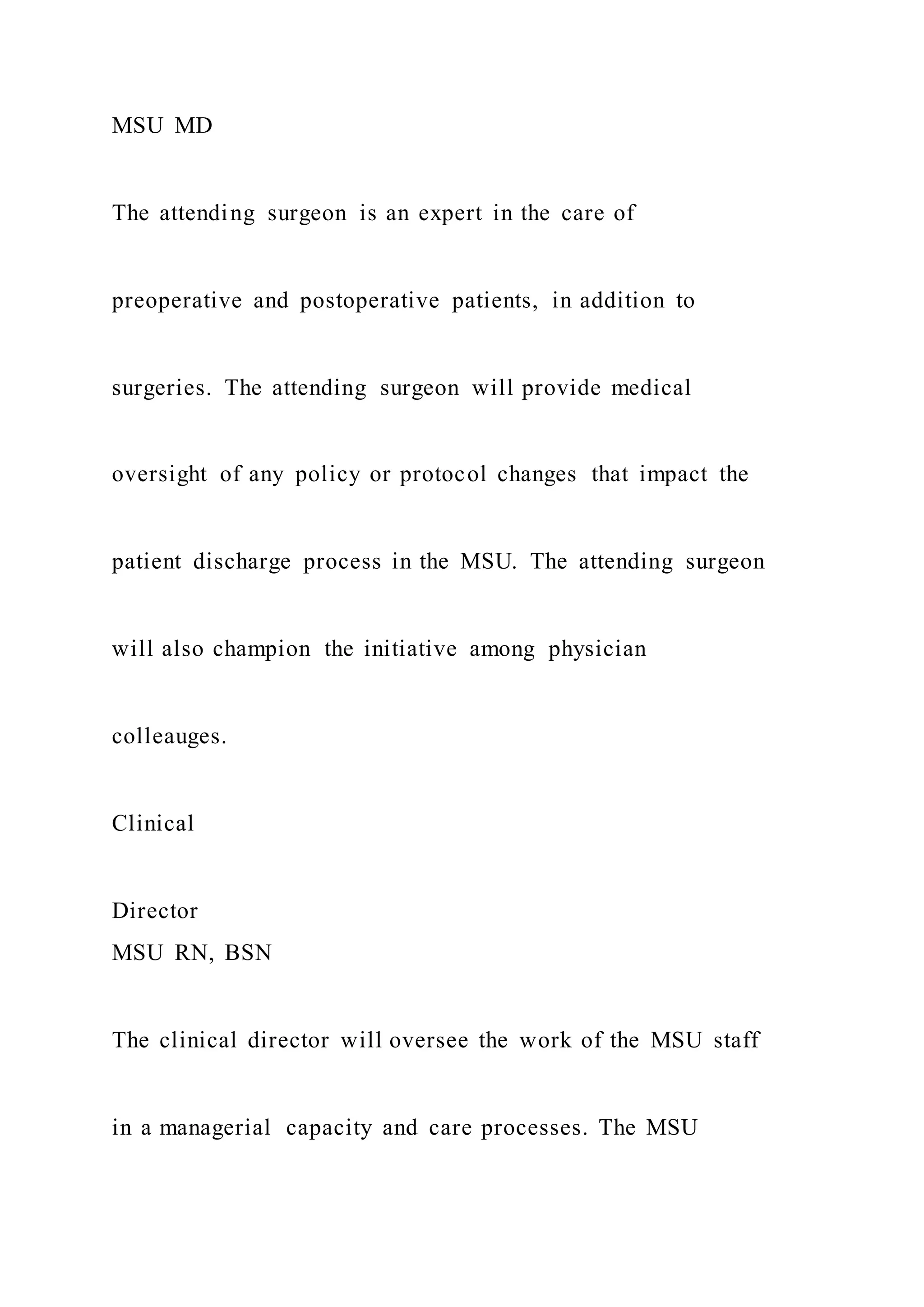
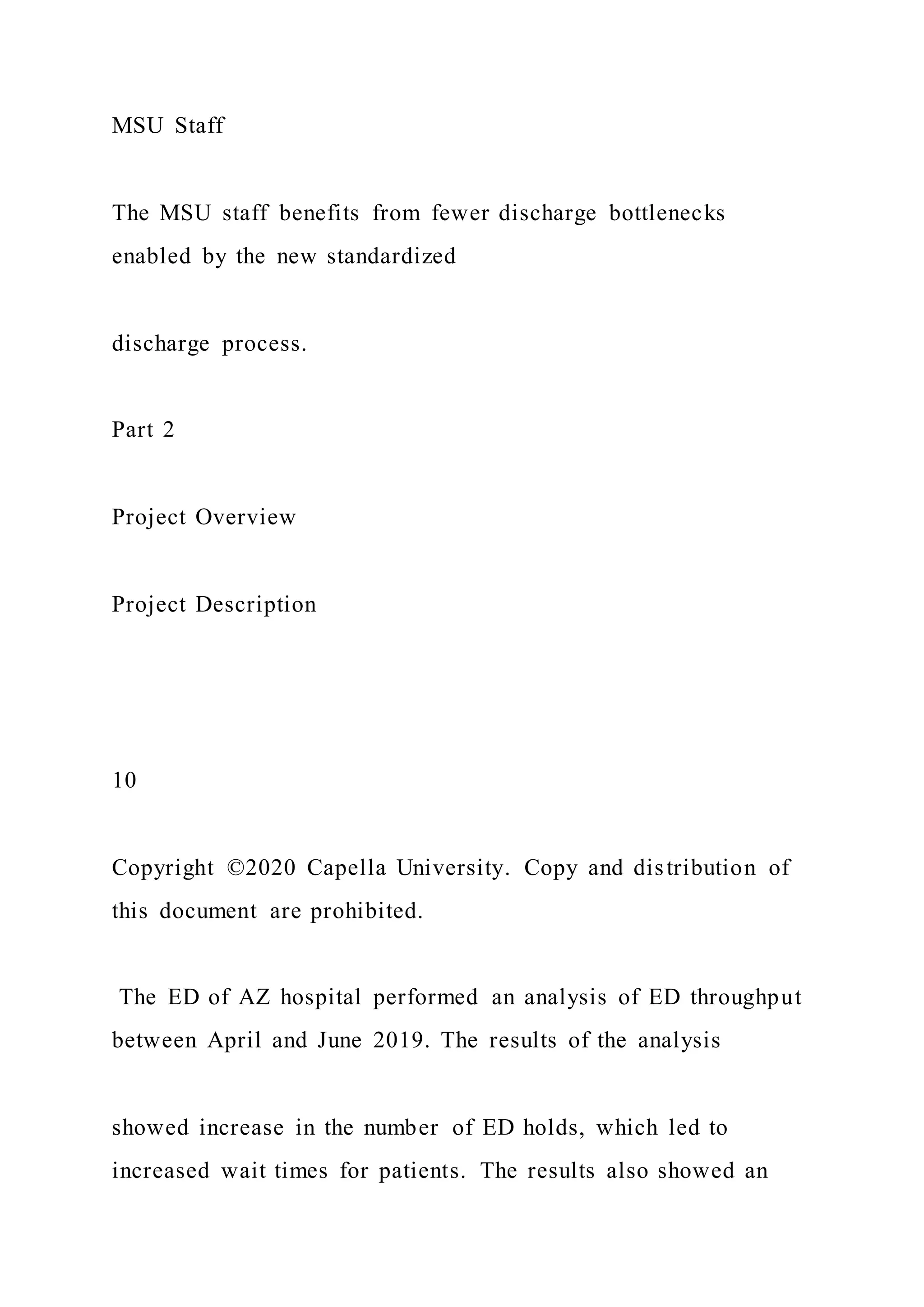
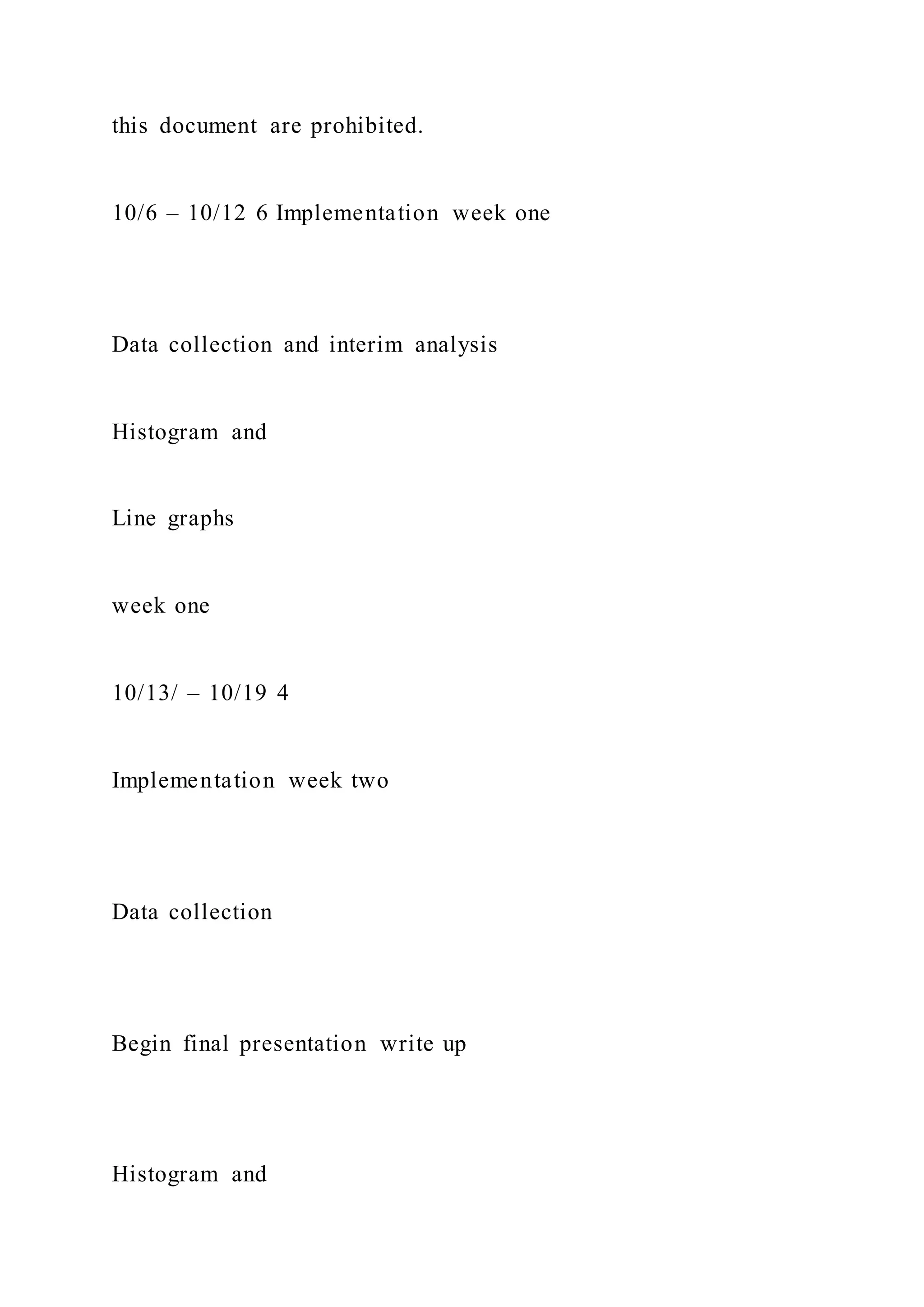
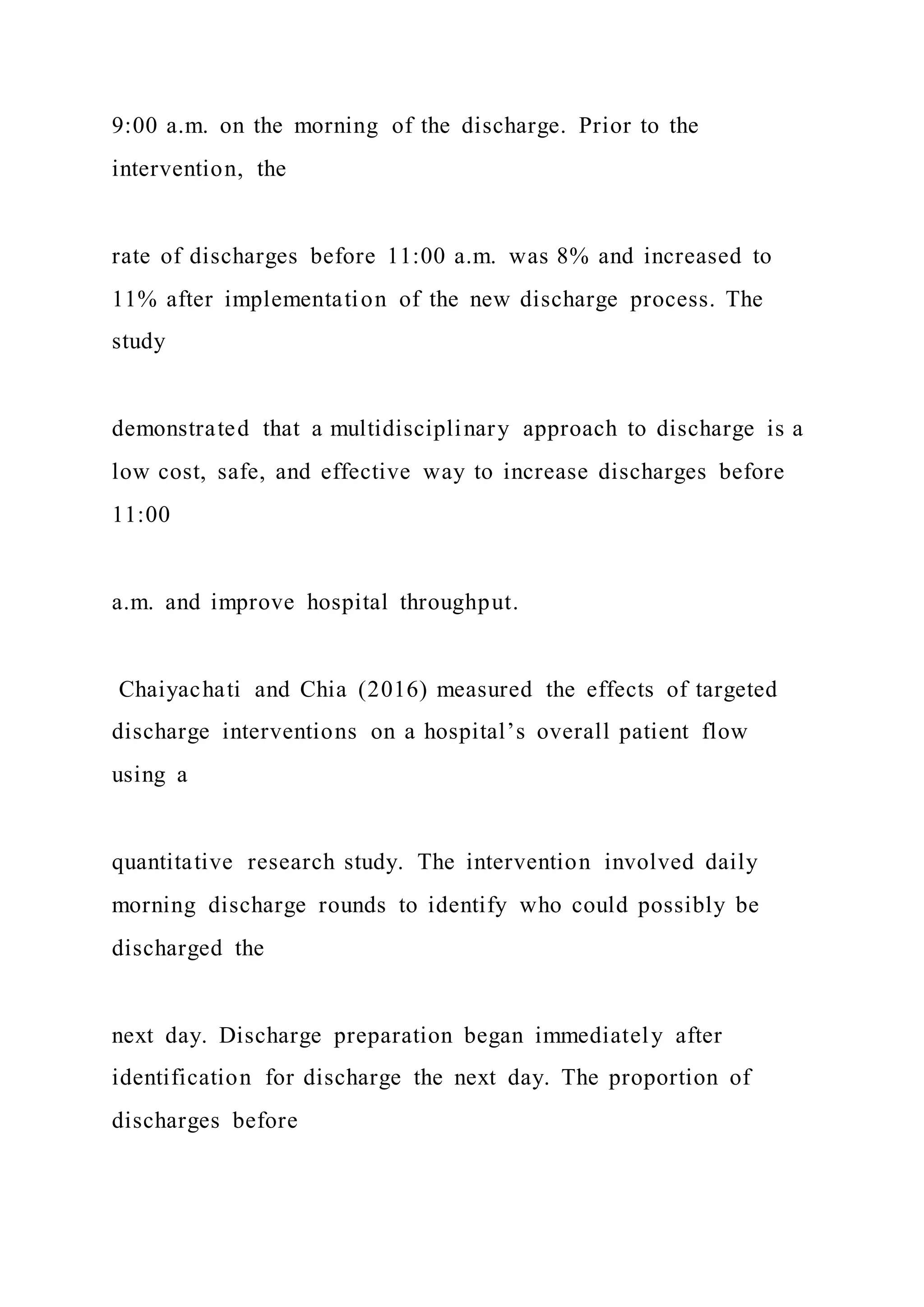
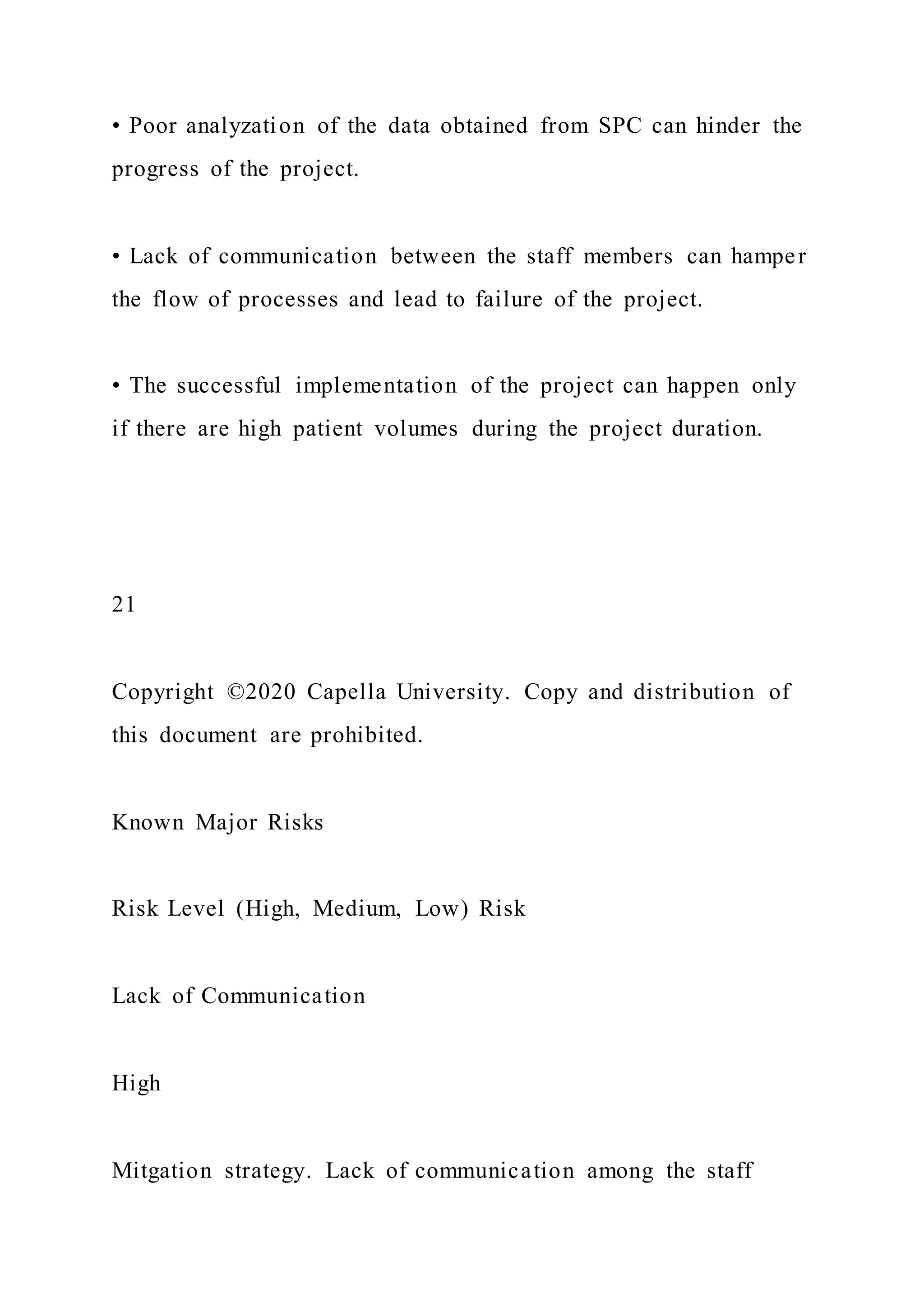
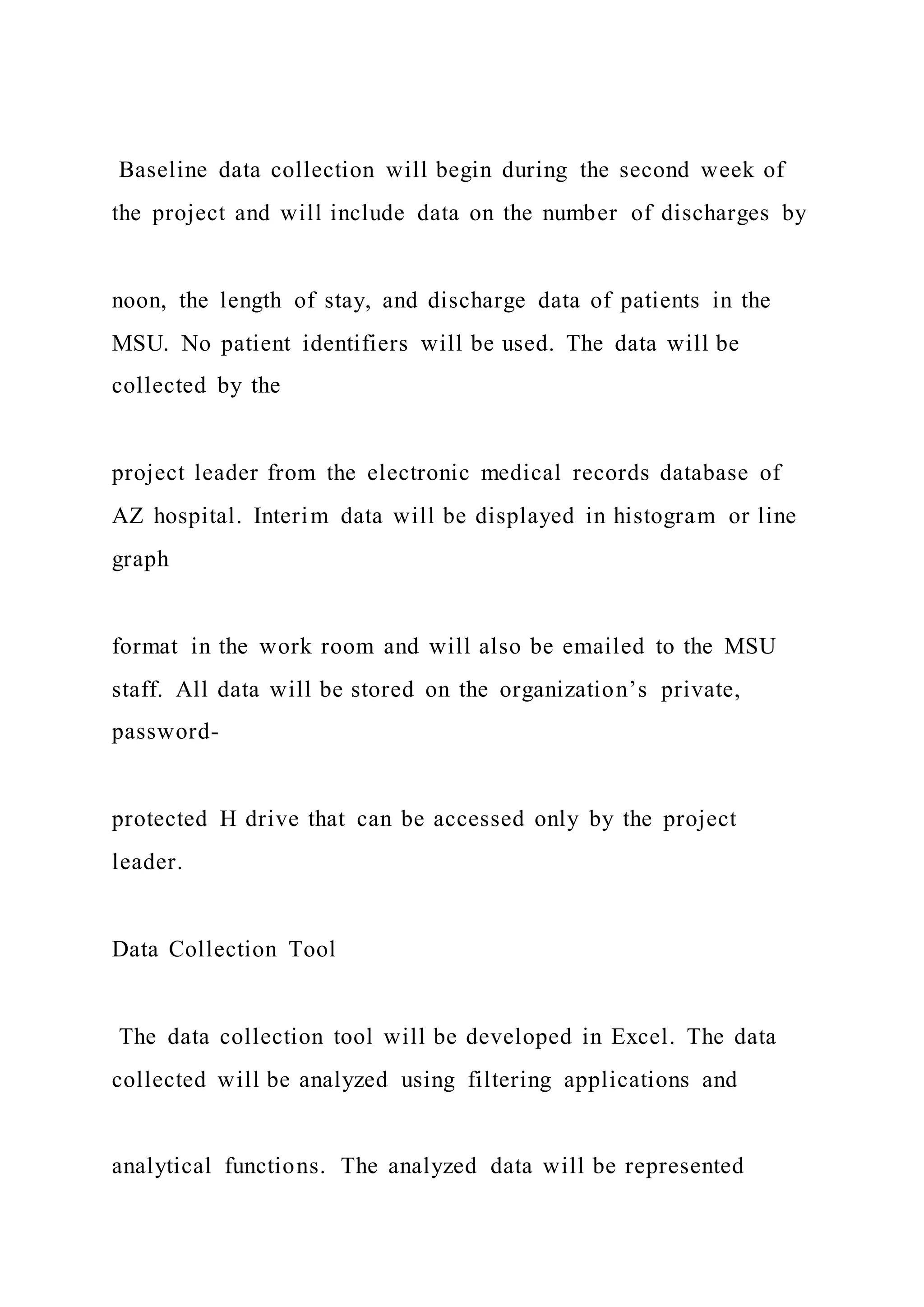
![Communication Strategy
Indicate here how the project manager will communicate to
sponsors, project team, and stakeholders. Describe the means
and frequency of communication, including meetings,
processes, and tools such as charts, wikis, and dashboards.
Proposed Outcomes
Metric
Outcome Measure
Process Measure
Countermeasure (optional)
What is being measured to determine project success
Answers specifically final outcome (“So what?”), such as [X]
percent patient satisfaction rate increase
Measures supporting final outcome such as compliance, time
motion, competency
Measures to ensure that there are no negative consequences in
other areas](https://image.slidesharecdn.com/1doctoralprojectcharterproposalchecklistinstruct-220920053858-baf1555b/75/1-Doctoral-Project-Charter-Proposal-Checklist-Instruct-56-2048.jpg)
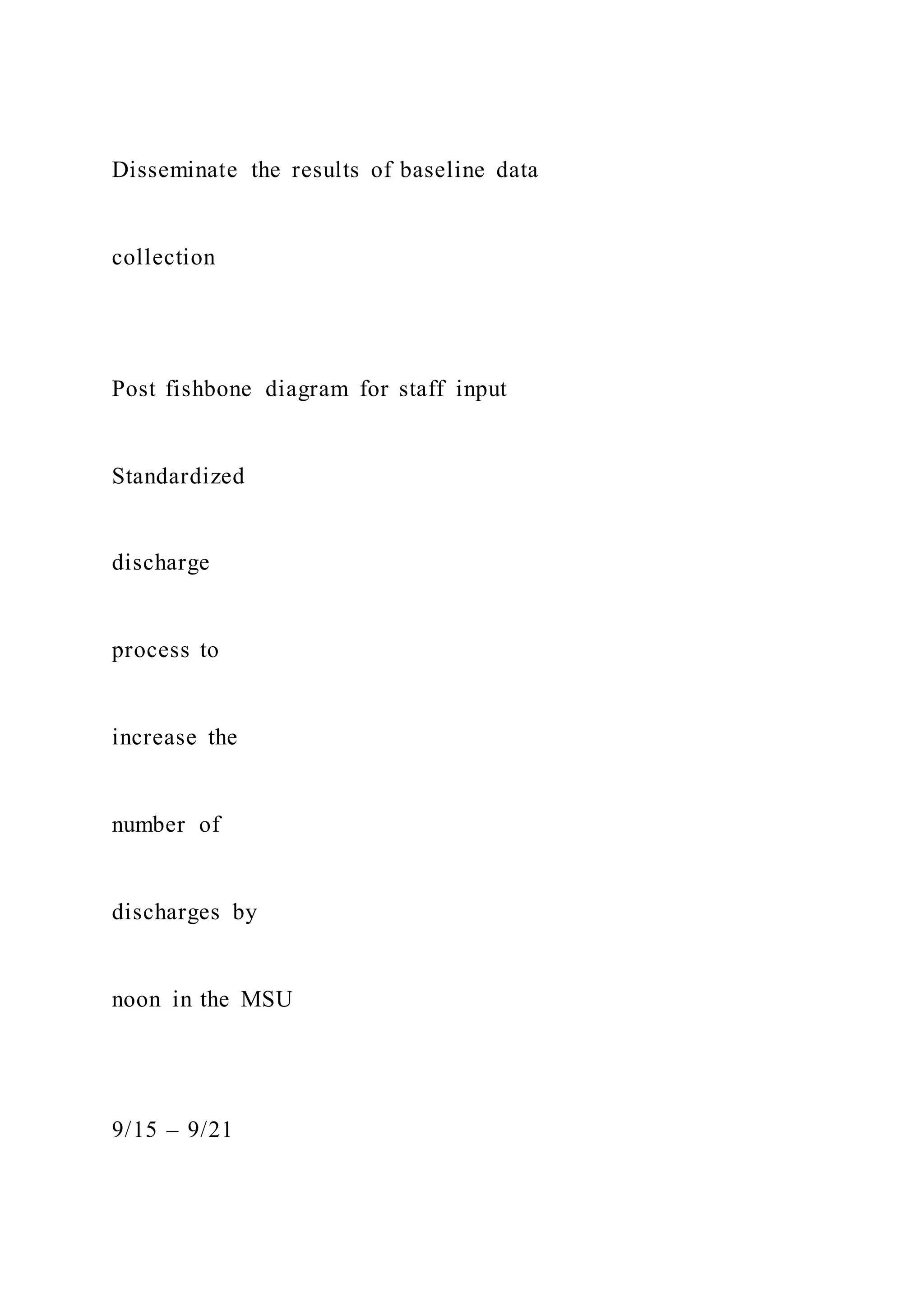
![Kaye, D. R., Richardson, C. R., Ye, Z., Herrel, L. A.,
Ellimoottil, C., & Miller, D. C. (2017). Association Between
Patient Satisfaction and Short-
Term Outcomes After Major Cancer Surgery. Annals of Surgical
Oncology, 24(12), 3486-3493.
http://dx.doi.org/10.1245/s10434-017-
6049-2
Schyve, P. M. (2009). Leadership in healthcare organizations: A
guide to joint commission leadership standards [White Paper].
https://psnet.ahrq.gov/issue/leadership-healthcare-
organizations-guide-joint-commission-leadership-standards
McKenna, P., Heslin, S. M., Viccellio, P., Mallon, W. K.,
Hernandez, C., & Morley, E. J. (2019). Emergency department
and hospital crowding:
causes, consequences, and cures. Clinical and Experimental
Emergency Medicine, 6(3), 189-195.
http://dx.doi.org/10.15441/ceem.18.022](https://image.slidesharecdn.com/1doctoralprojectcharterproposalchecklistinstruct-220920053858-baf1555b/75/1-Doctoral-Project-Charter-Proposal-Checklist-Instruct-110-2048.jpg)