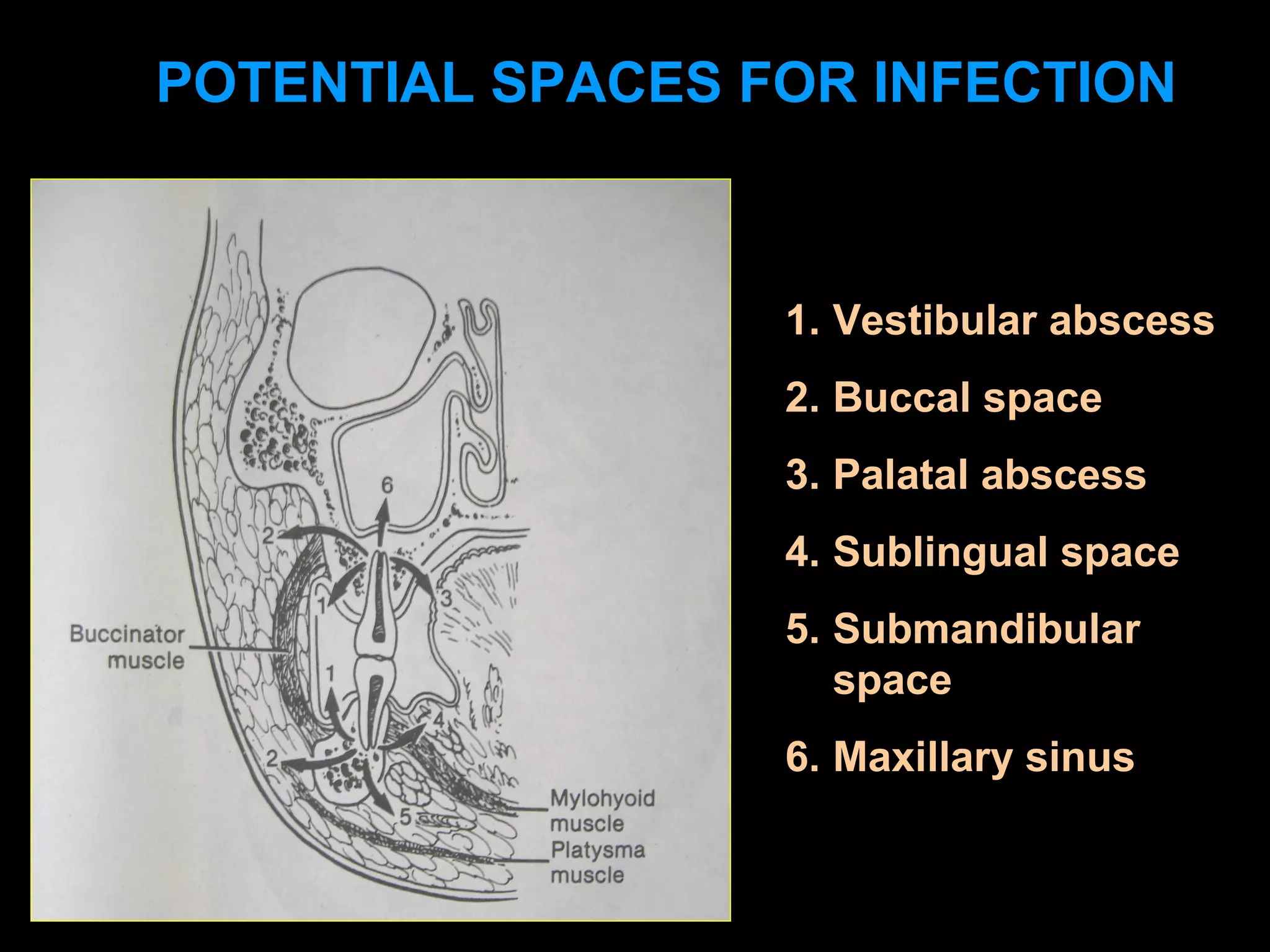
This document discusses potential spaces in the head and neck region where infections can develop from dental sources, and provides guidance on treating these infections. It outlines several key spaces that can become infected, including the buccinator space, sublingual space, submandibular space, and pterygomandibular space. Dangerous complications are described such as Ludwig's angina and cavernous sinus thrombosis. The document recommends empiric antibiotic therapy, incision and drainage of infected spaces, culture and sensitivity testing to identify the causative organism, focused antibiotic treatment, and removal of the infection source (such as teeth) for managing these infections.