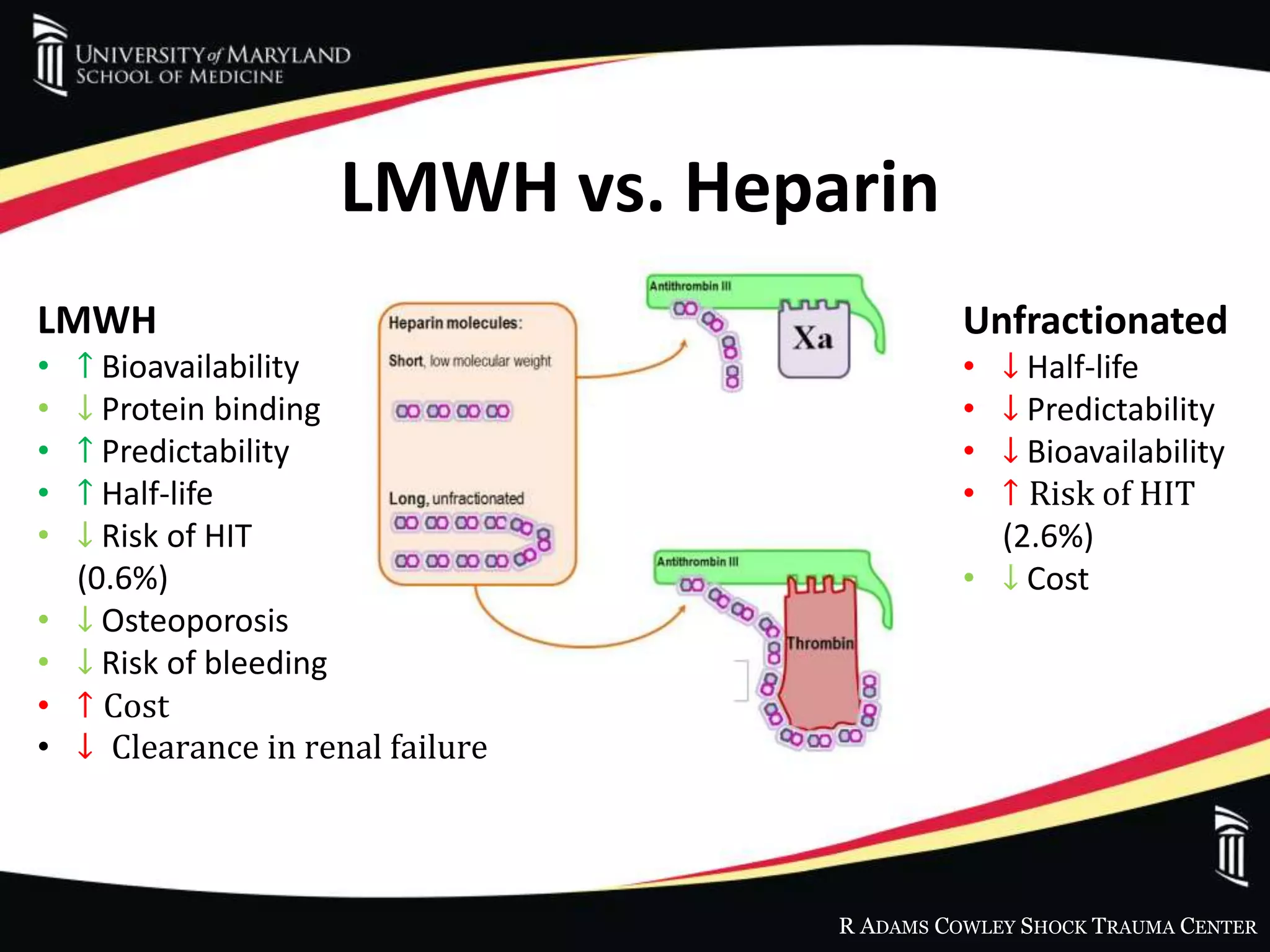
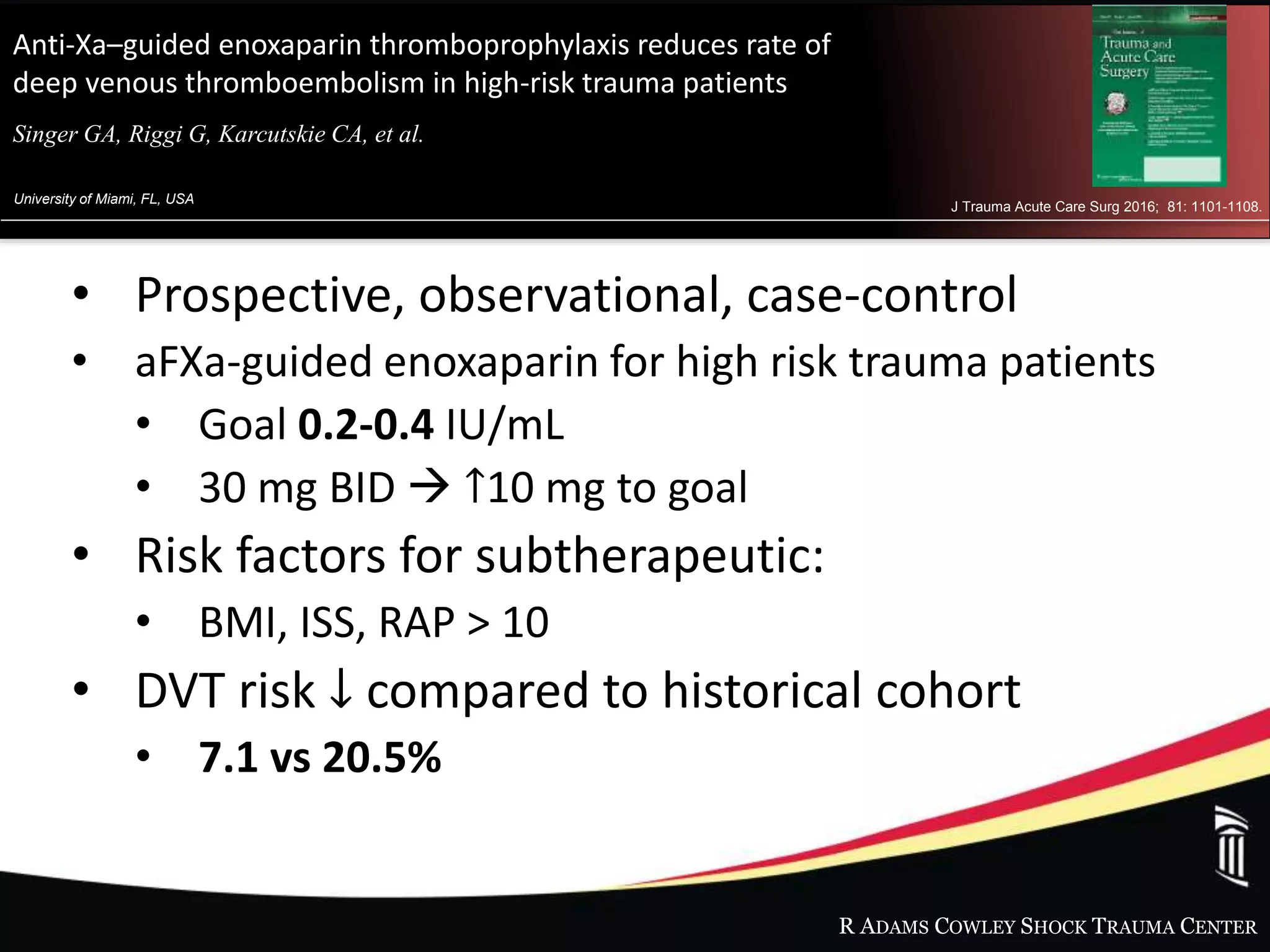
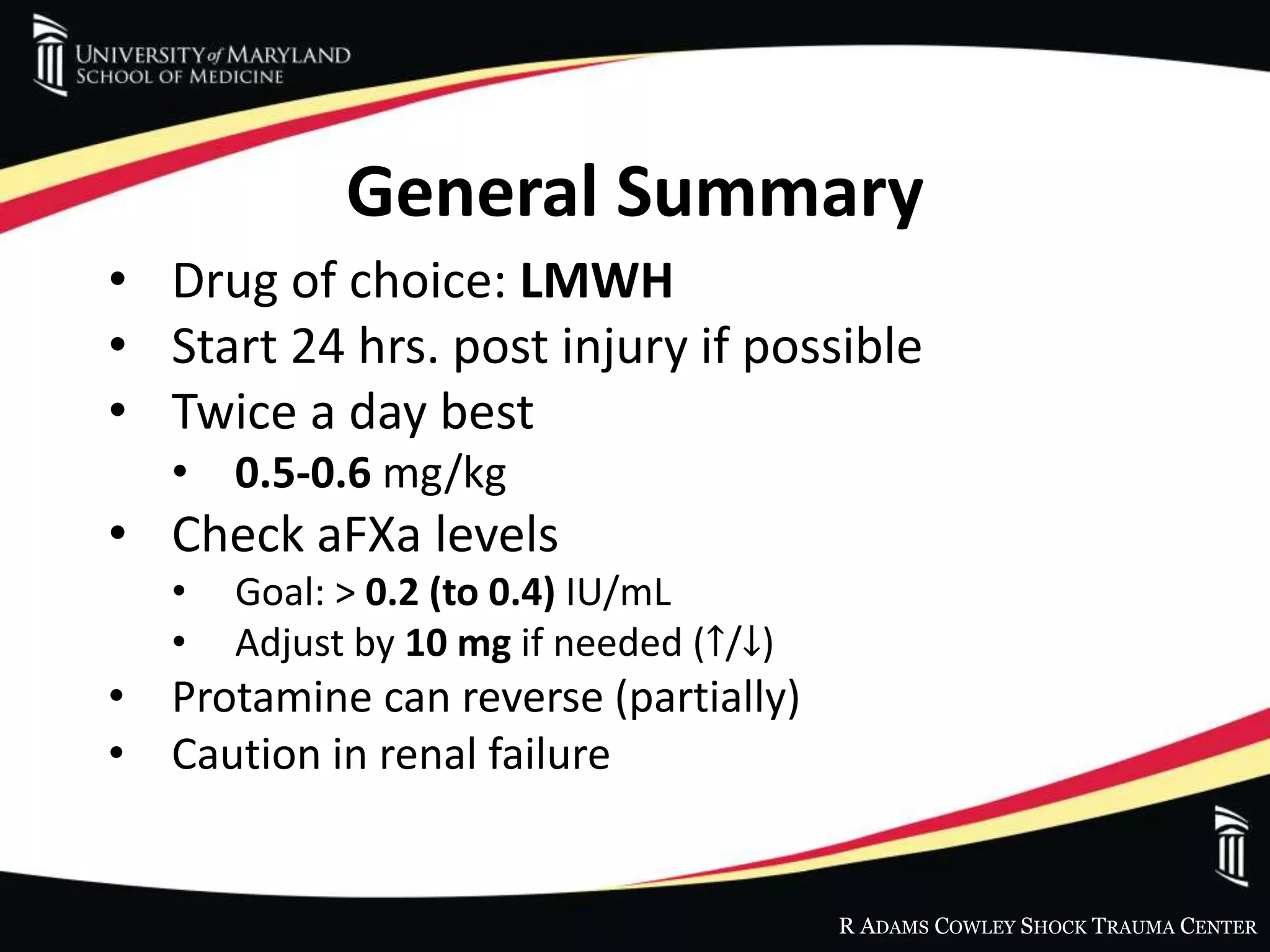
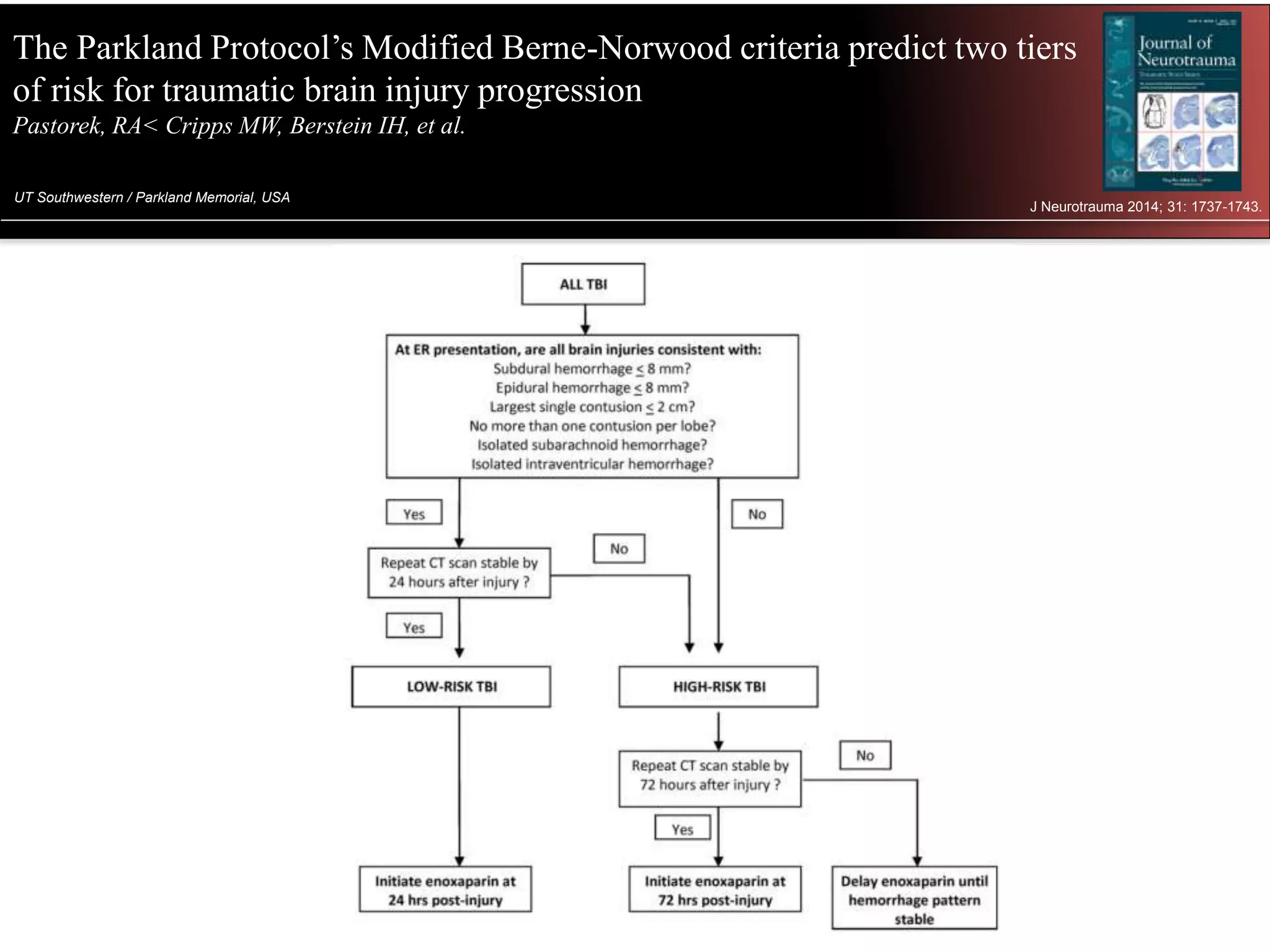
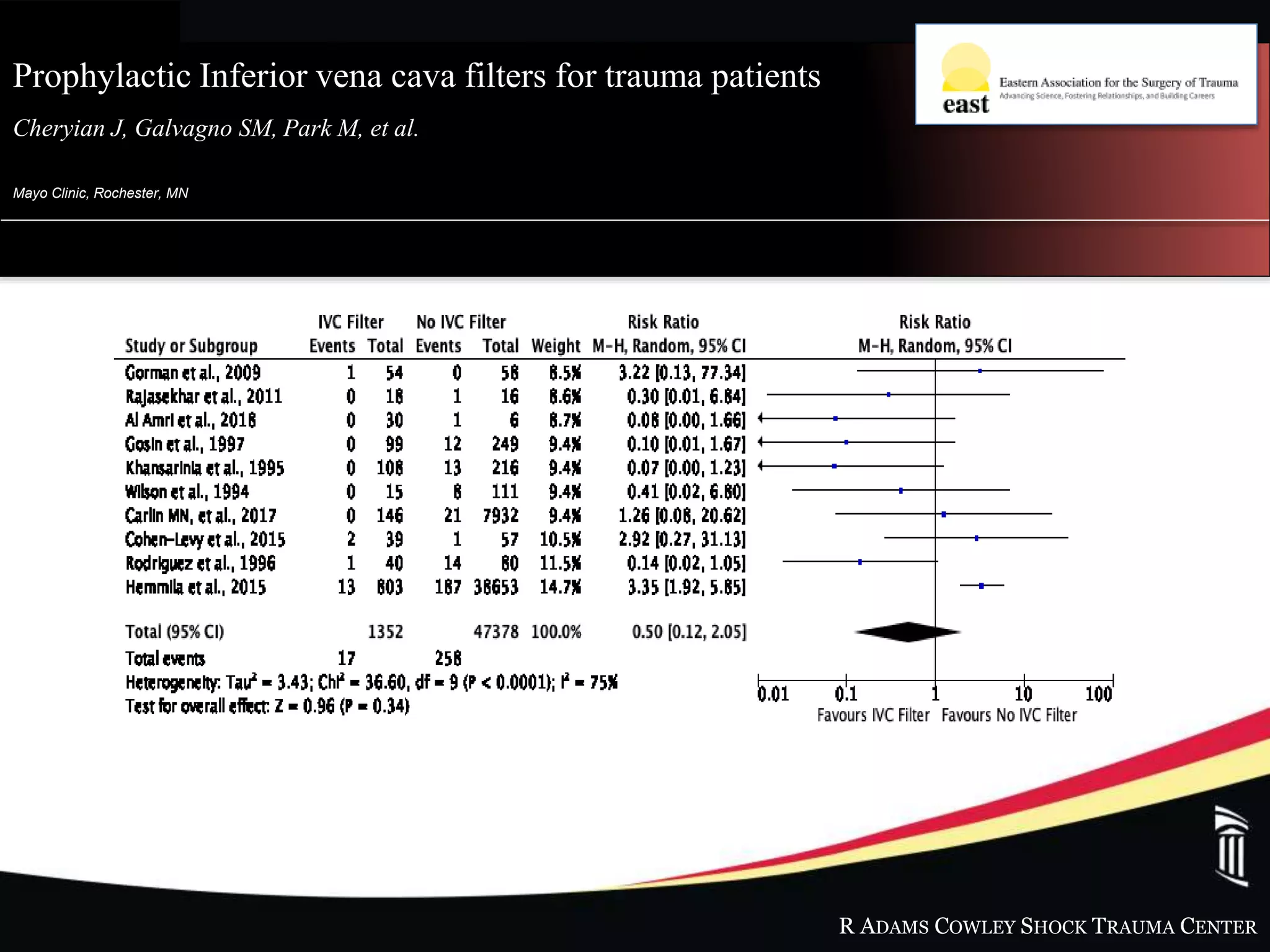
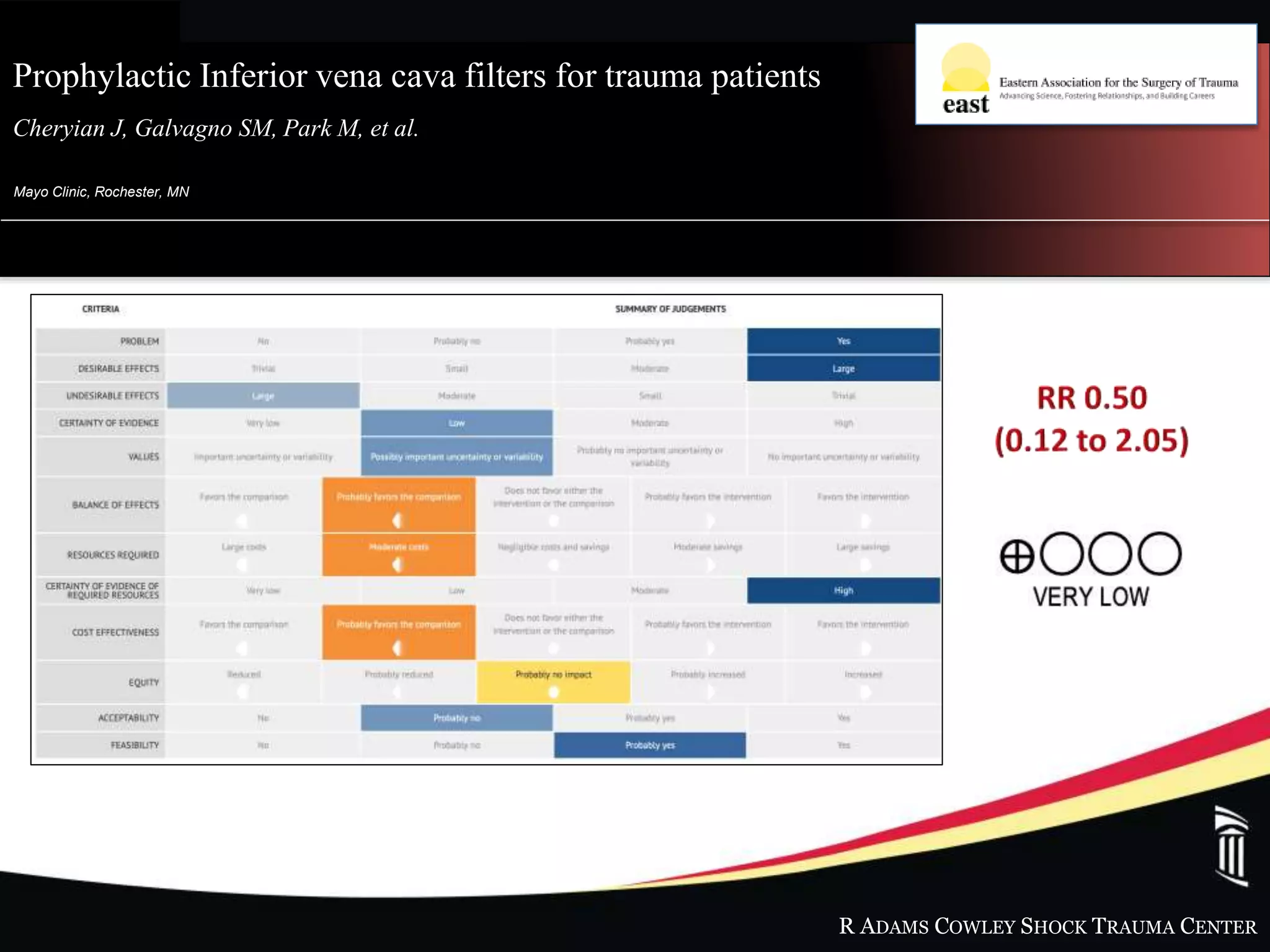
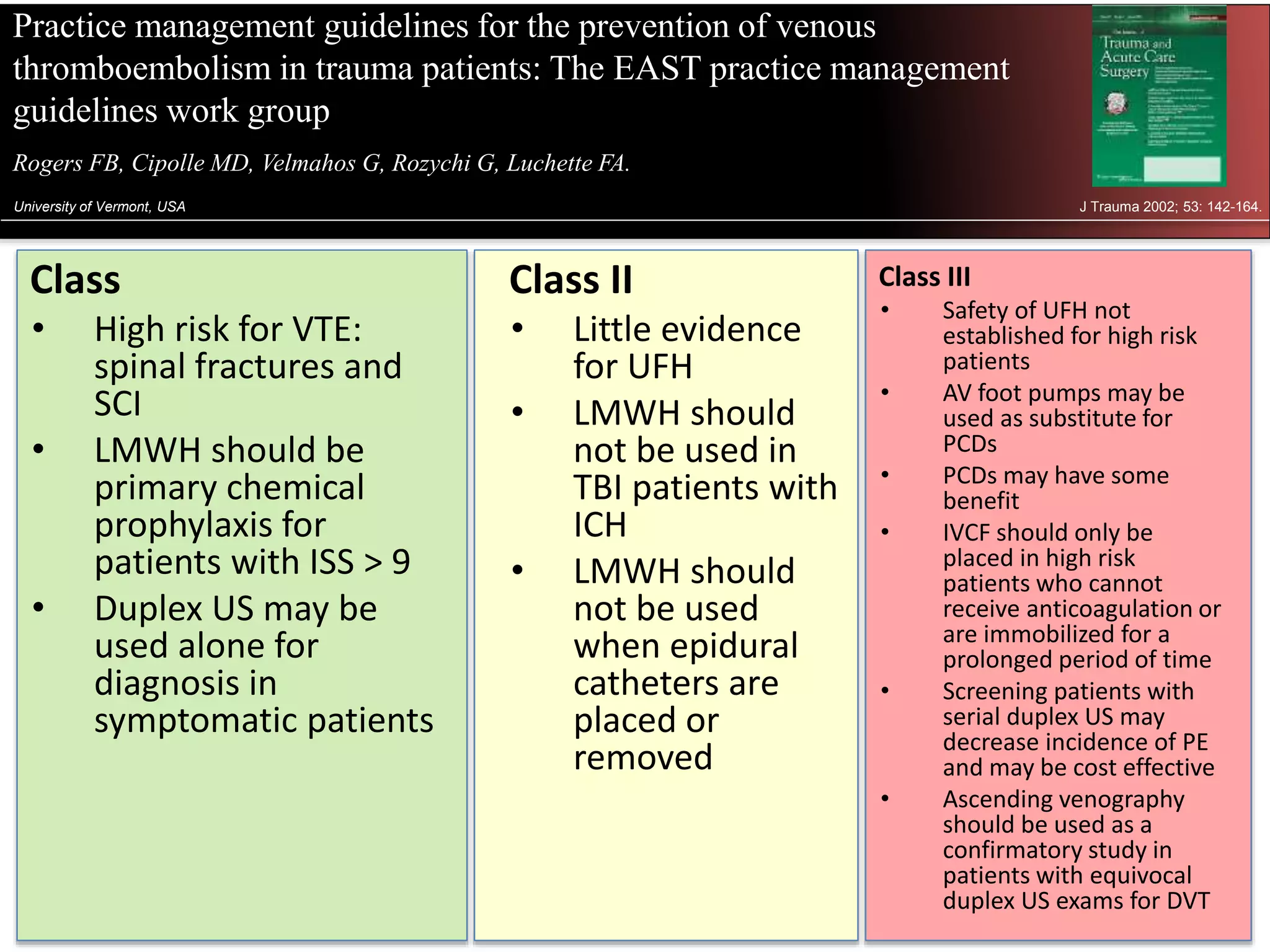
The document discusses thromboembolism (VTE) in trauma patients. It provides information on the incidence, pathophysiology, and risk factors for VTE. It reviews evidence on pharmacological prophylaxis including low molecular weight heparin (LMWH), optimal dosing guided by anti-Xa levels, and concerns about use in traumatic brain injury (TBI) and renal dysfunction. Other prevention modalities like inferior vena cava filters are discussed. Overall, LMWH is recommended for prophylaxis when possible but monitoring anti-Xa levels and adjusting dosing based on patient risk factors and renal function.