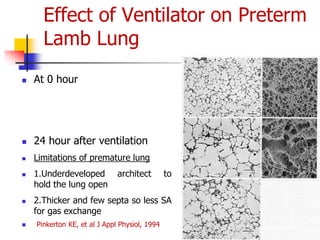
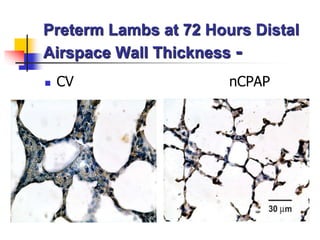
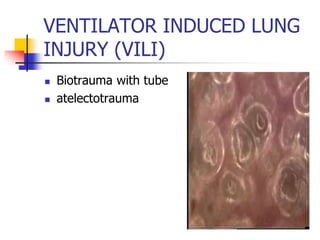
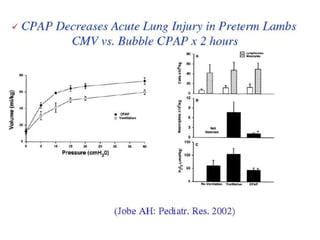
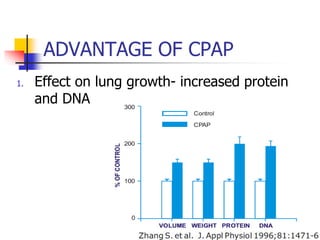
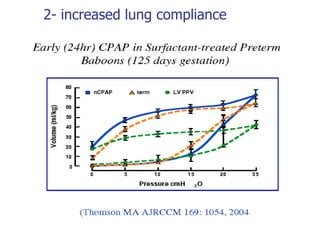
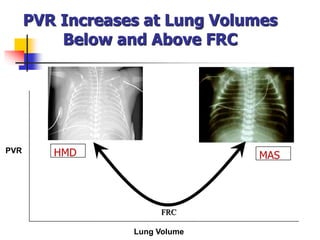
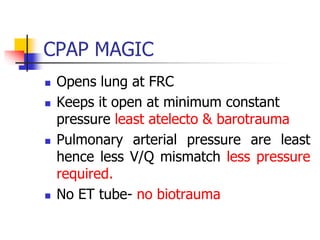
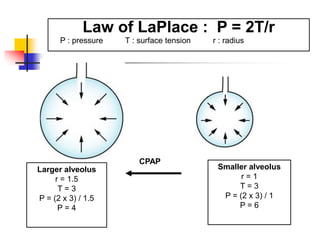
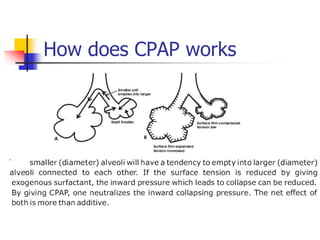
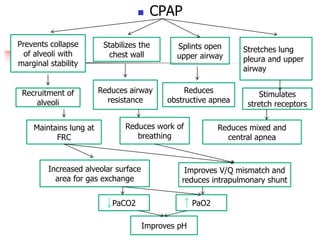
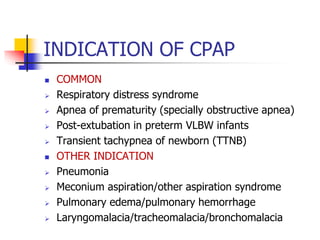
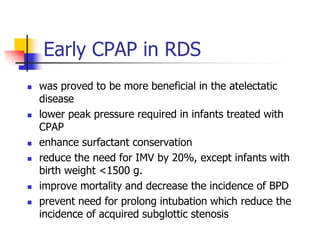
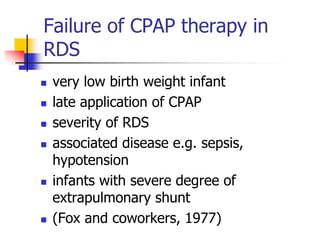
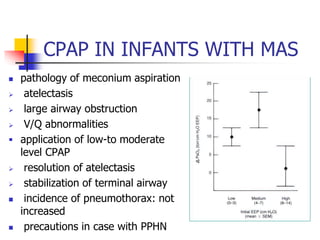
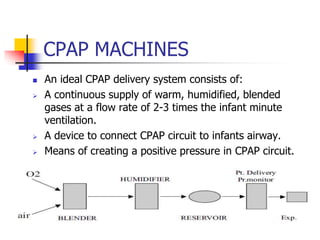
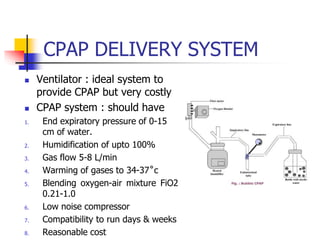
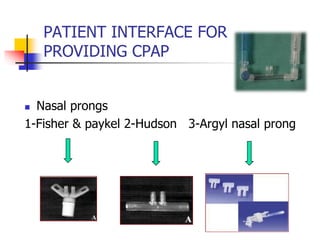
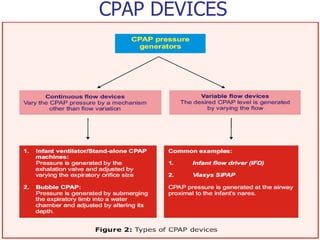
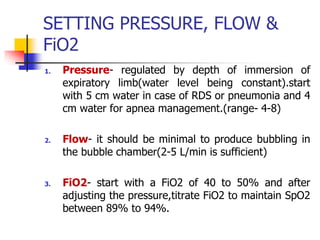
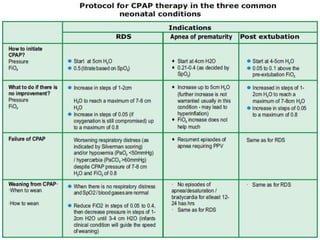
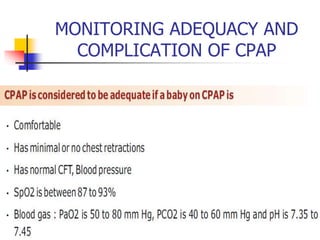
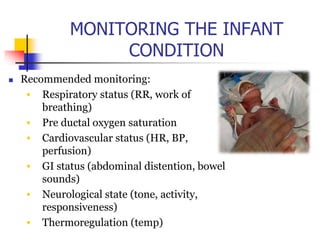
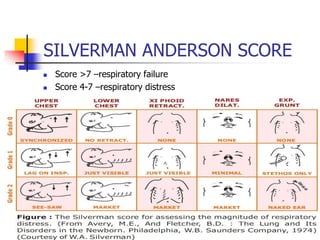
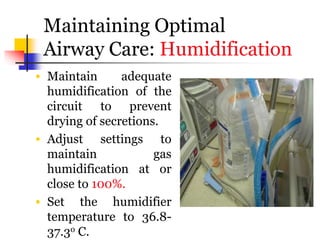
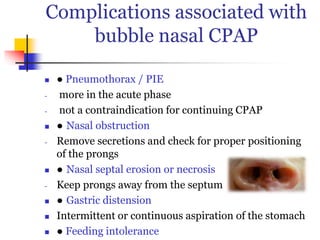
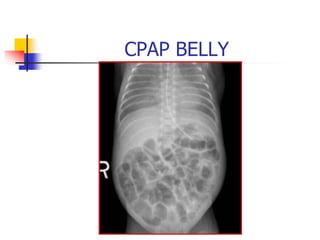
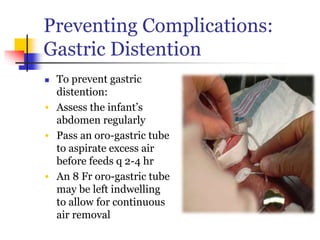
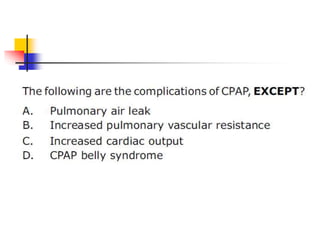
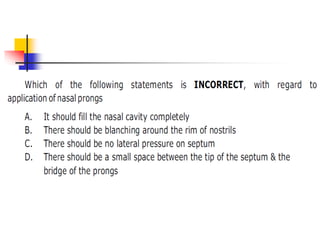
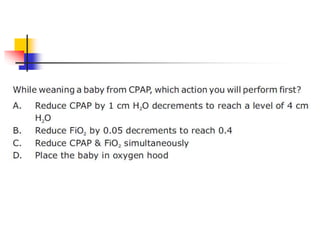
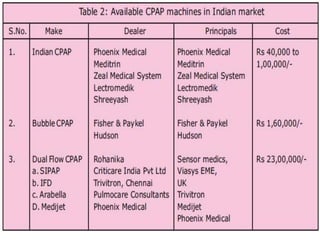
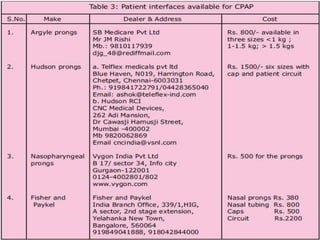
The document discusses Continuous Positive Airway Pressure (CPAP) therapy, which maintains positive transpulmonary pressure to improve lung function and gas exchange in spontaneously breathing infants. It outlines the history, physiology, indications, advantages, contraindications, and monitoring of CPAP, highlighting its effectiveness in treating respiratory distress syndrome and apnea of prematurity. The document also addresses the complications associated with CPAP therapy and provides guidelines for optimal settings and patient care.