The document provides information on HIV/AIDS, including:
1. HIV was first identified in 1981 and there have been two major strains identified, HIV-1 and HIV-2.
2. HIV is transmitted through bodily fluids and can be transmitted sexually or through contact with infected blood.
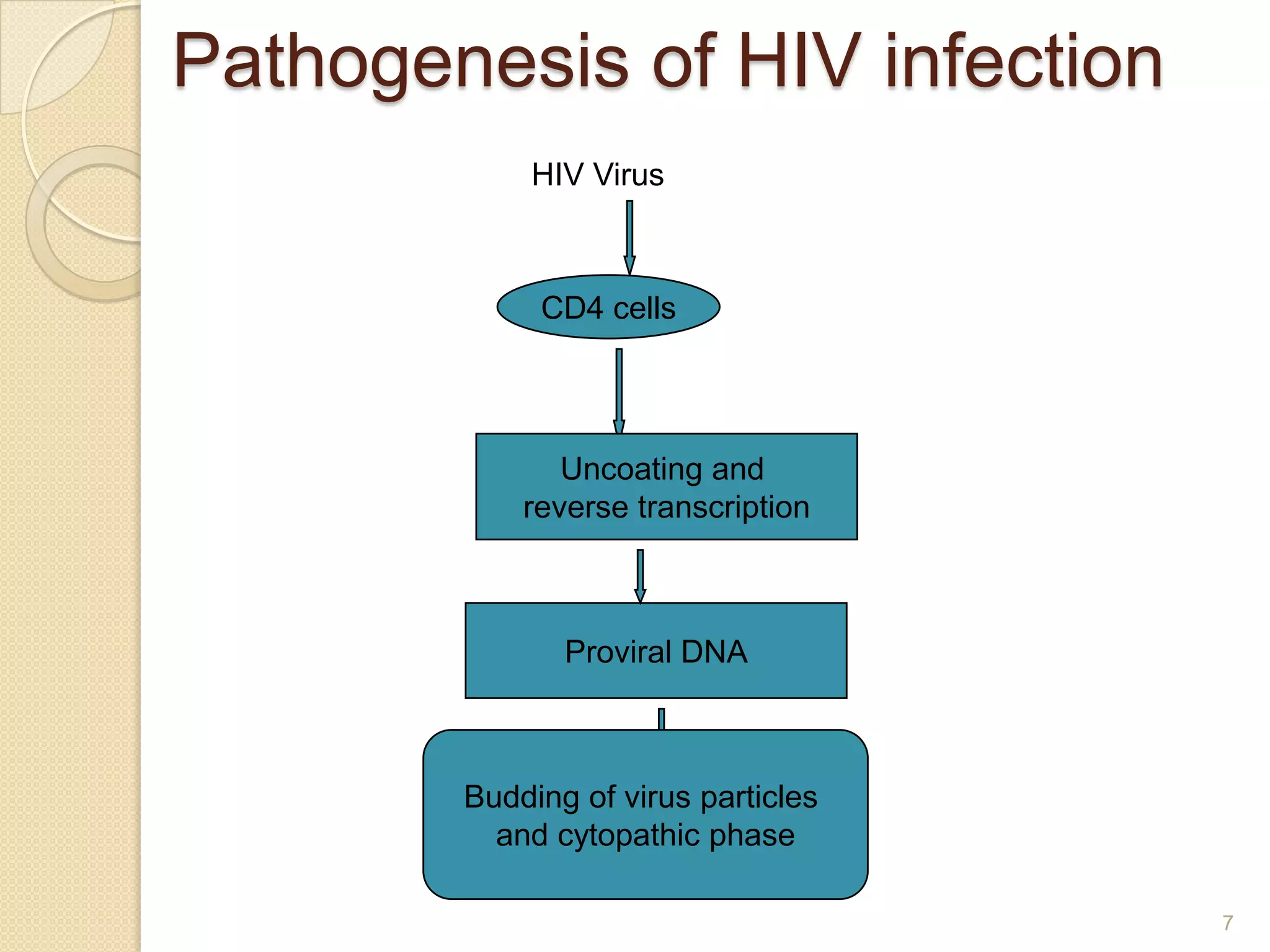
3. There are three phases of HIV infection eventually resulting in AIDS if not treated. Antiretroviral treatment can suppress the virus and prevent AIDS.