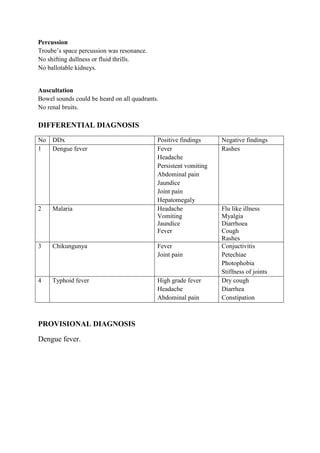
This patient presented with fever, sore throat, joint pain, vomiting and hepatomegaly. Based on her symptoms and physical exam findings, the provisional diagnosis was dengue fever. Dengue virus is transmitted via mosquito bites and causes an immune response that can damage blood vessels and organs. The management focused on supportive care like fluid replacement to prevent complications from dehydration. Tests like complete blood count and ELISA were recommended to confirm the diagnosis.