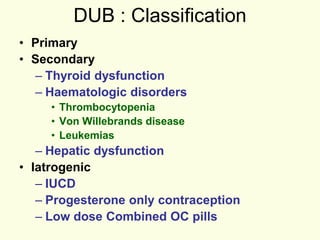
This document discusses dysfunctional uterine bleeding (DUB), its classification, causes, and pathophysiology. It begins by defining DUB as abnormal uterine bleeding without identifiable organic disease. DUB is classified as primary or secondary to conditions like thyroid dysfunction. The document then covers characteristics of normal menstruation versus abnormal bleeding patterns like menorrhagia, hypomenorrhea, and others. It details the role of hormones in the normal menstrual cycle and how imbalances can lead to DUB, discussing mechanisms like estrogen withdrawal, breakthrough, and progesterone breakthrough bleeding. The document concludes by outlining several mechanisms through which DUB can occur, such as hyper-estrogenic states and impaired haemostatic and re-epithelialization