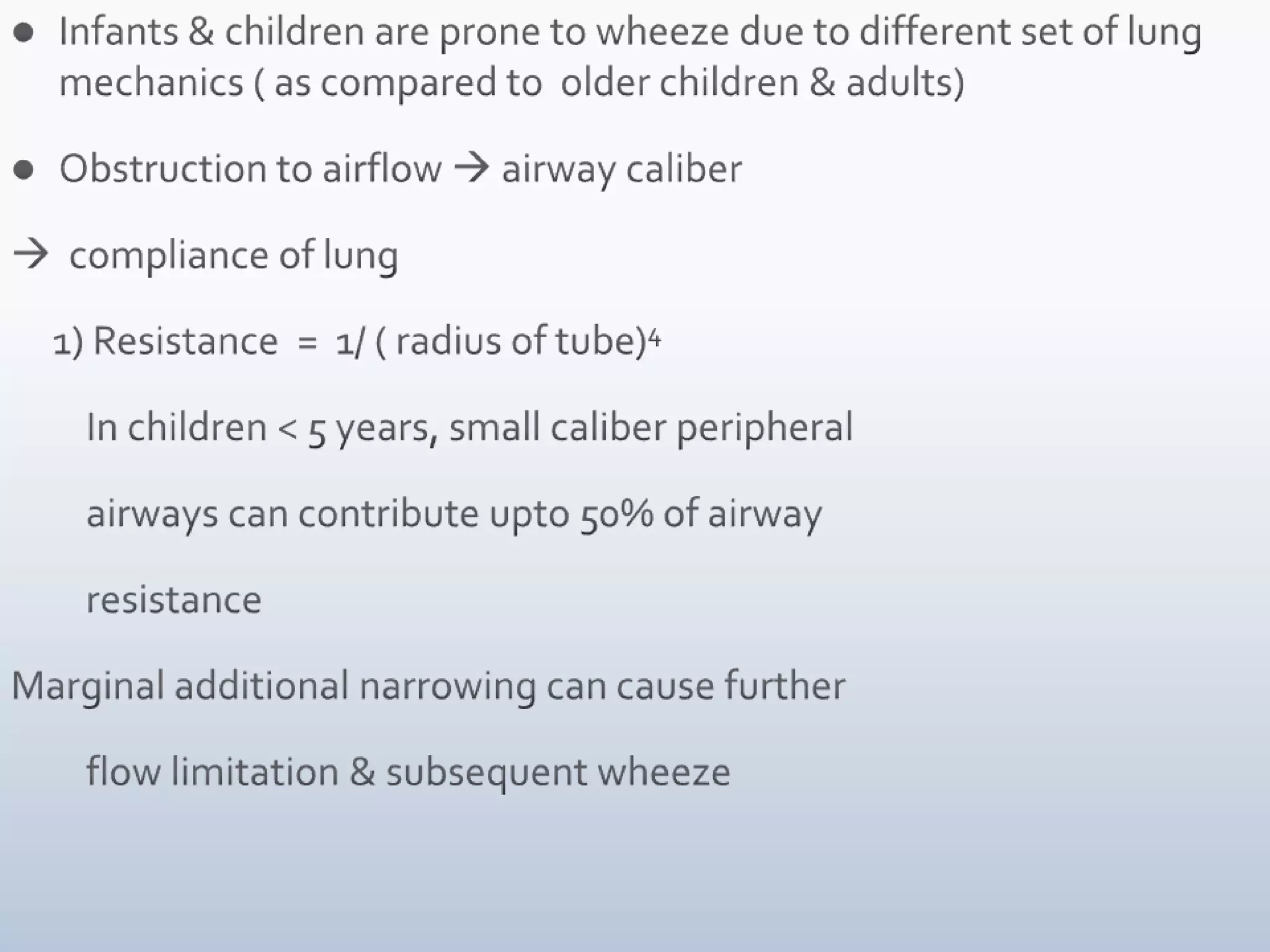
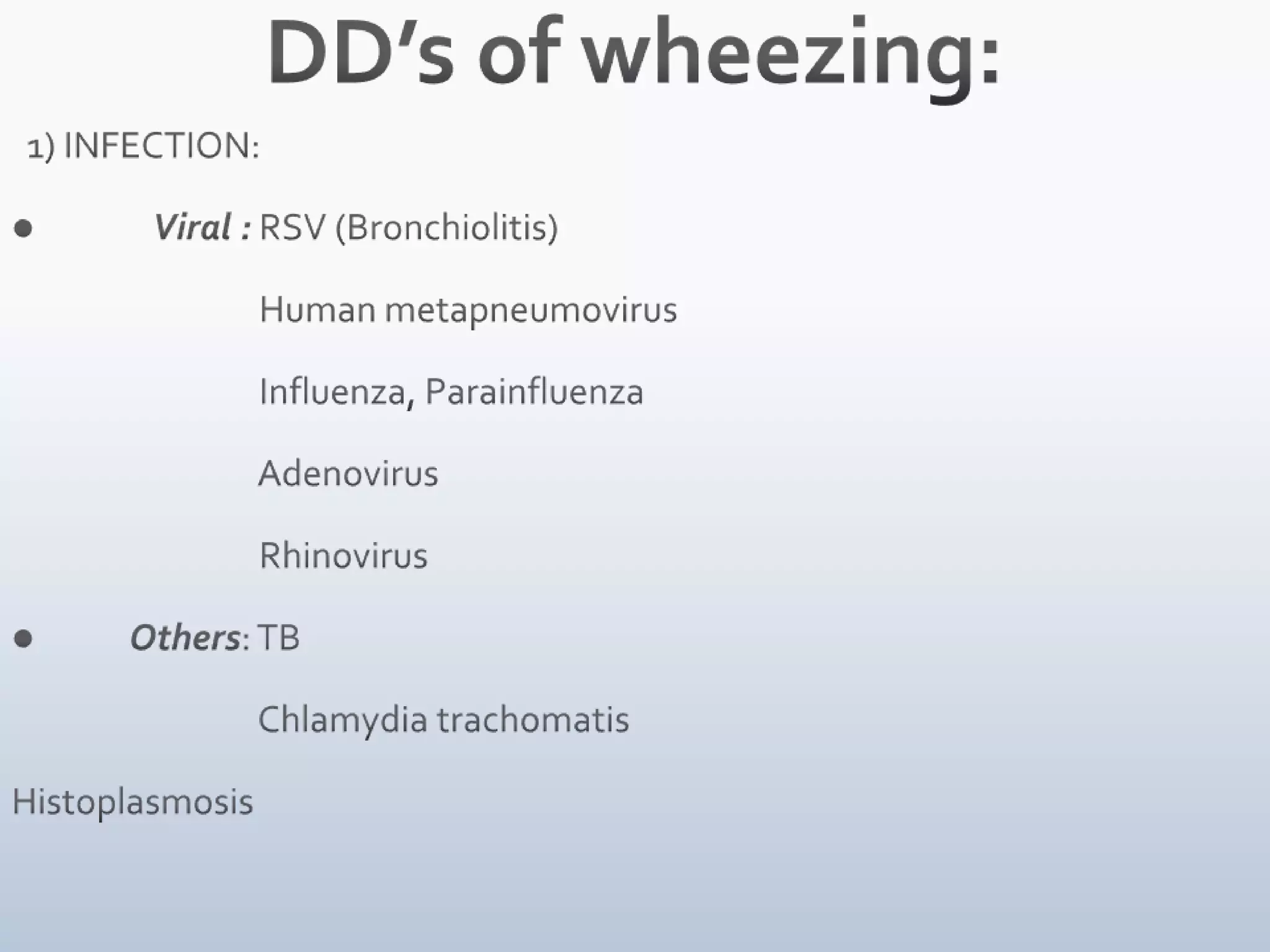
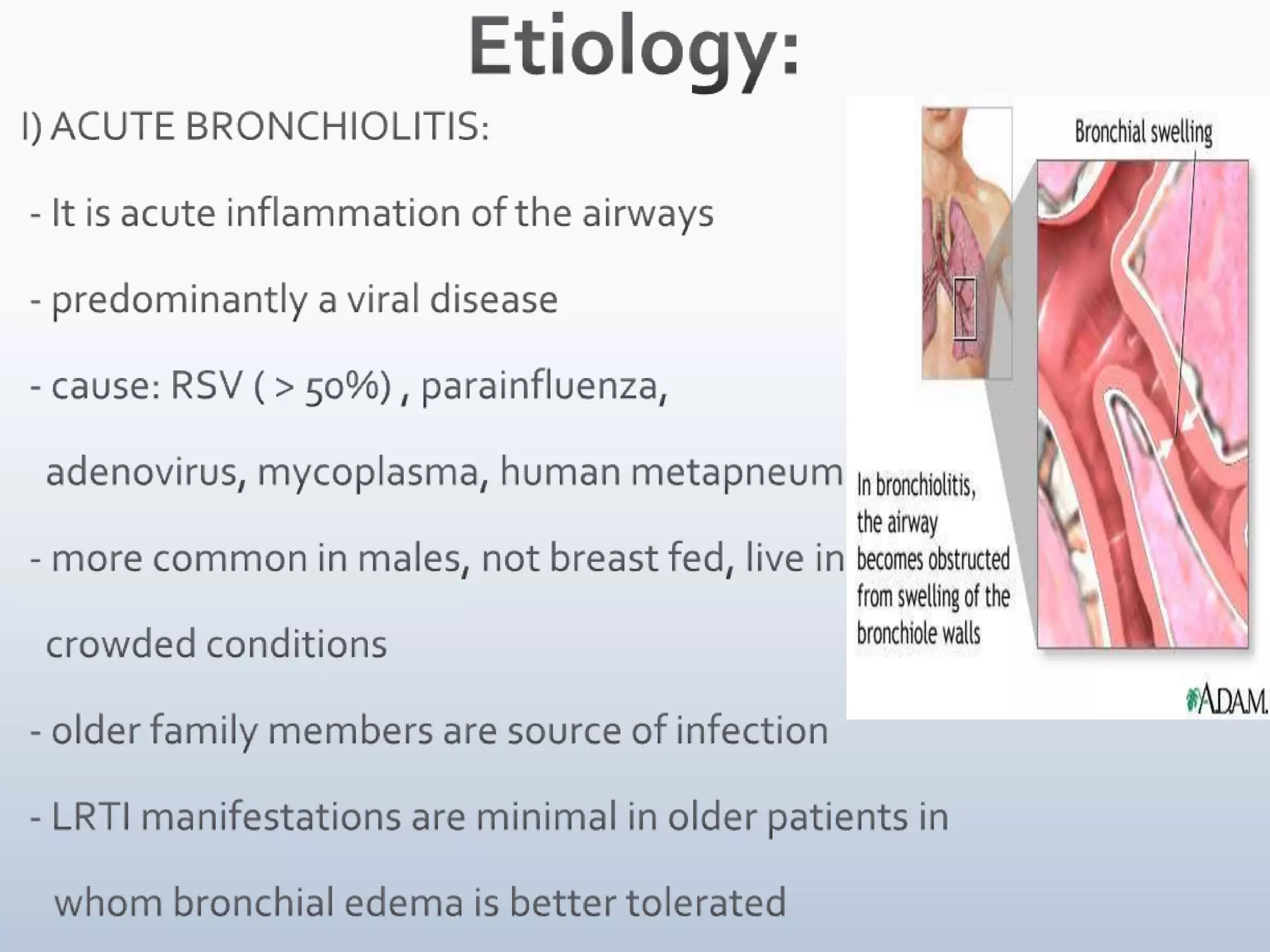
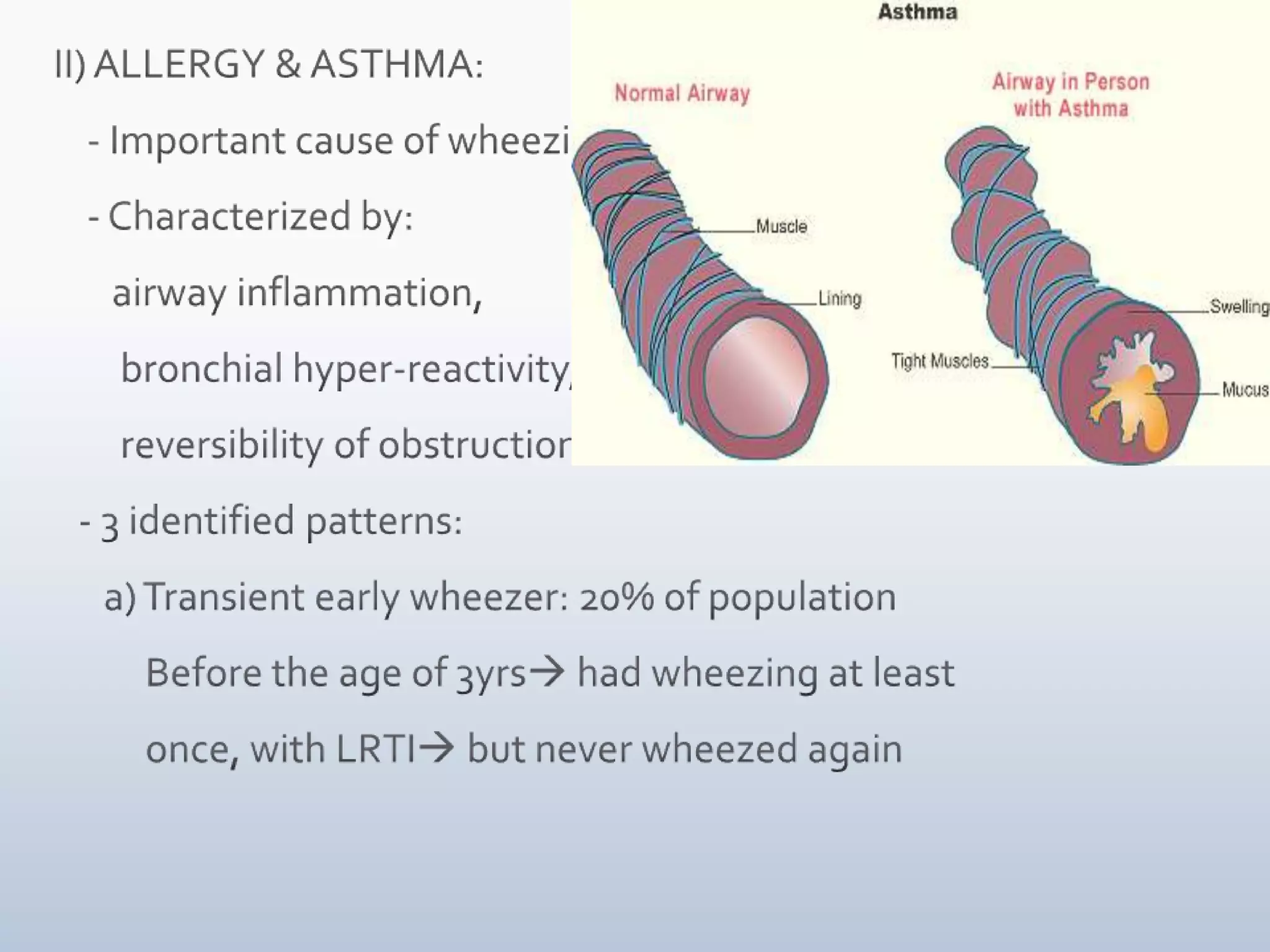
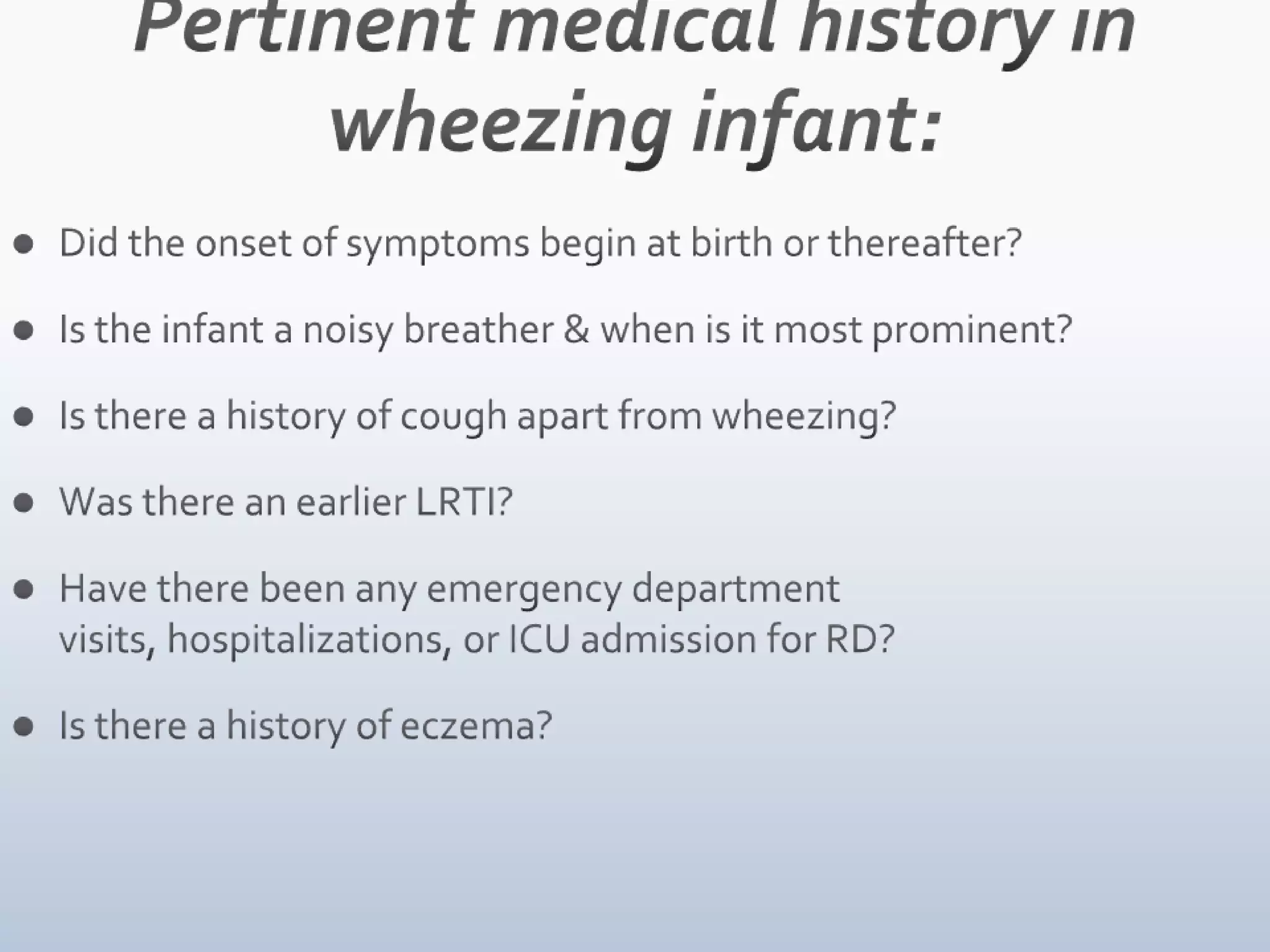
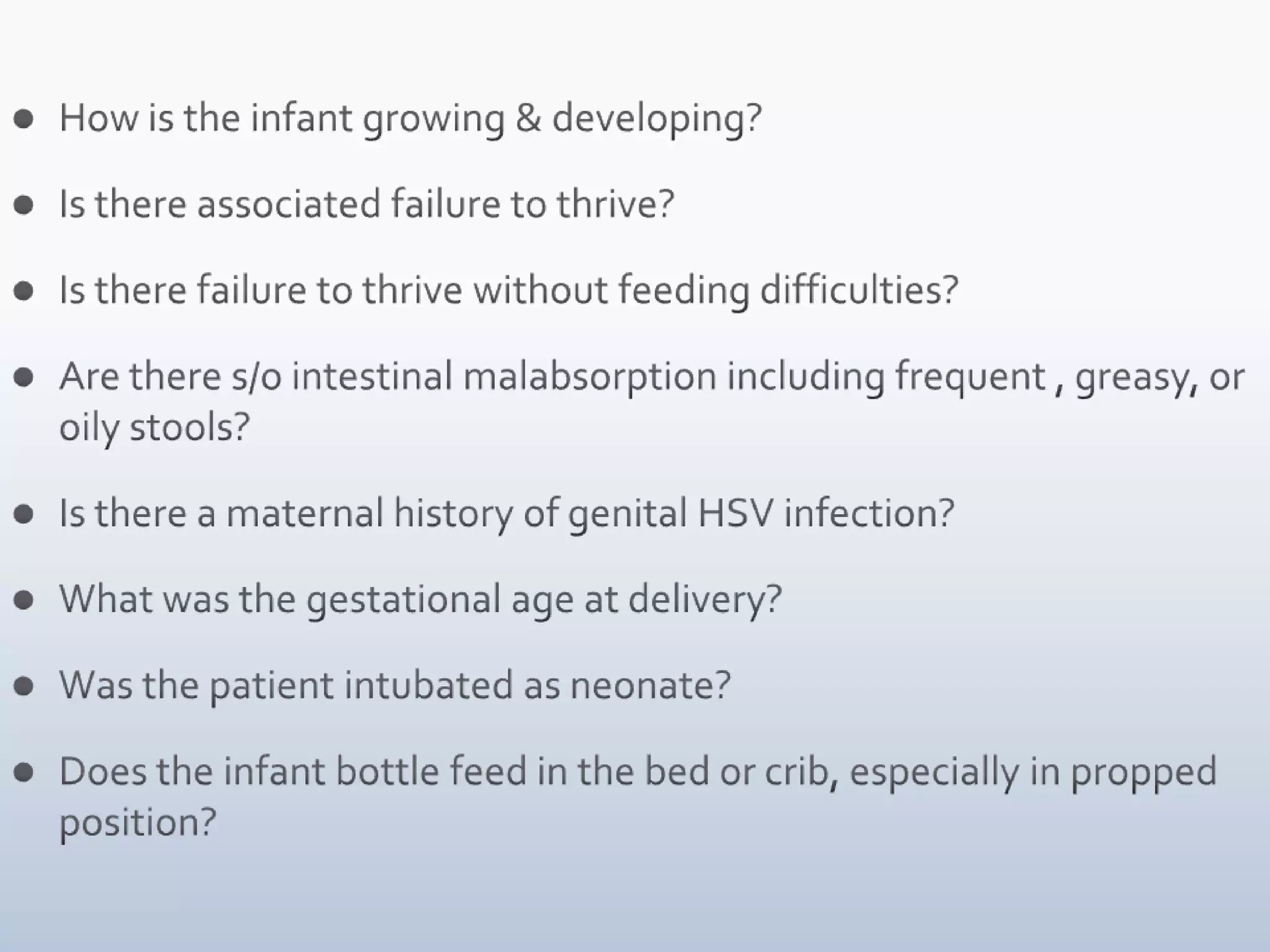
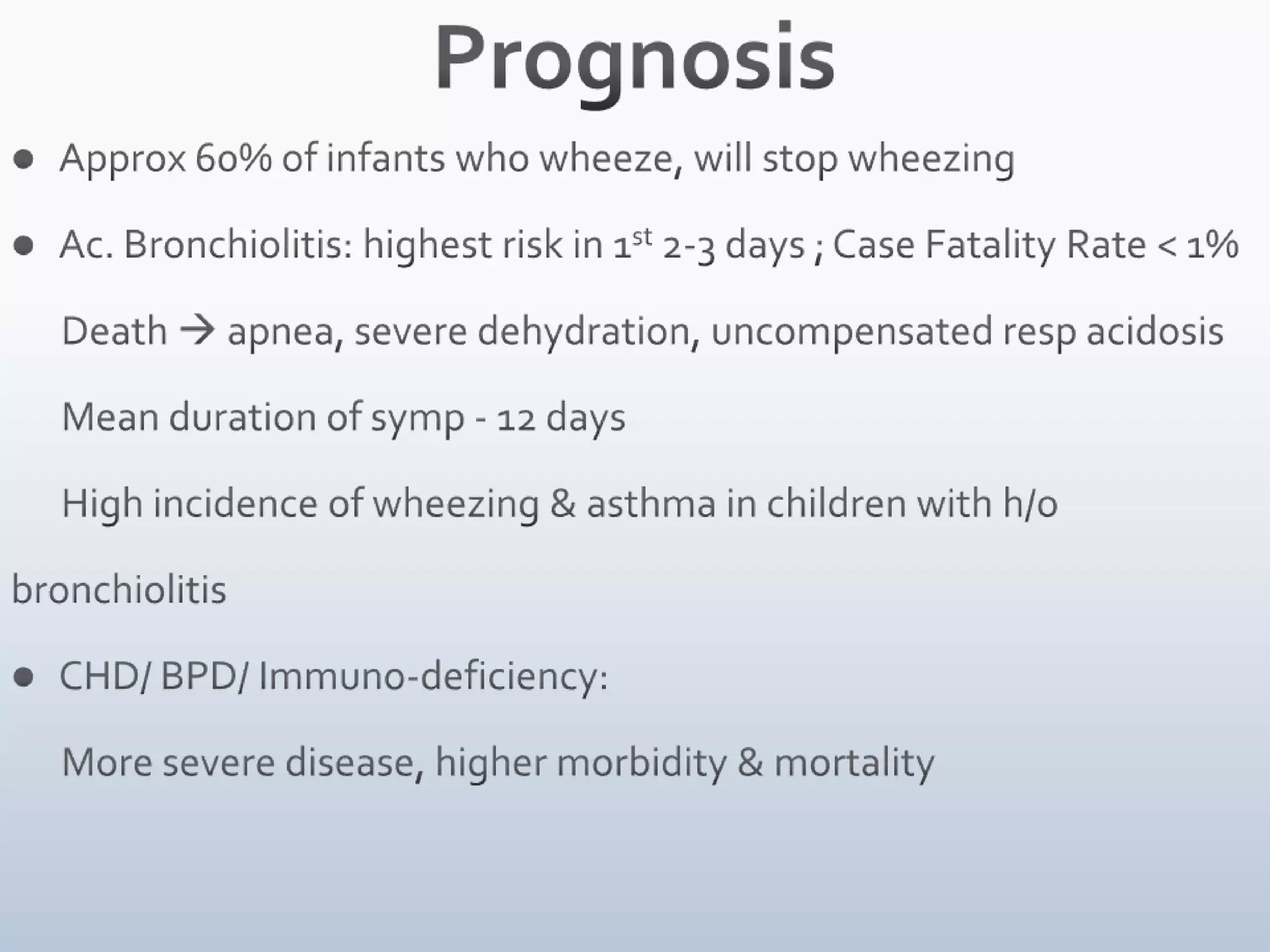
Wheezing in children can have many causes. It is often due to viral infections like RSV bronchiolitis in infants, which causes inflammation and narrowing of the small airways. Asthma is another common cause and presents with recurrent wheezing episodes. Younger children are more prone to wheezing due to their small airway size and lung mechanics. A thorough history, physical exam, and diagnostic testing can help identify the underlying condition causing wheezing to guide treatment.