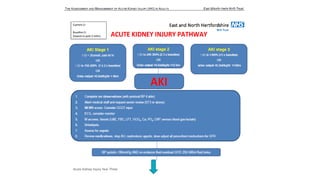
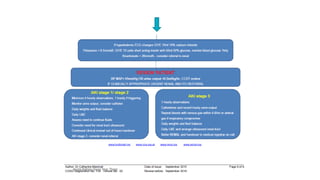
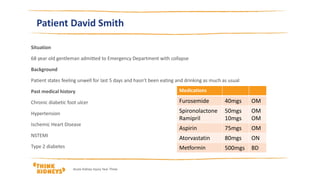
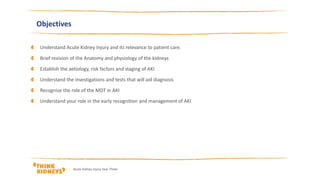
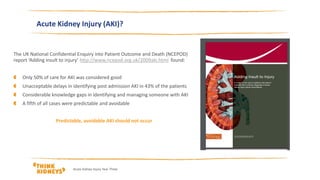
This document provides an overview of acute kidney injury (AKI) for undergraduate nurses. It defines AKI, discusses risk factors and causes, and outlines steps for identifying, managing, and referring patients with AKI. Key points include:
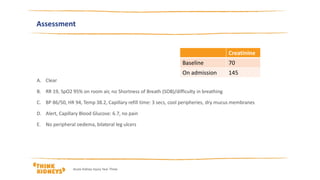
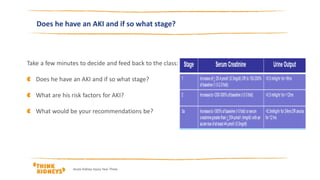
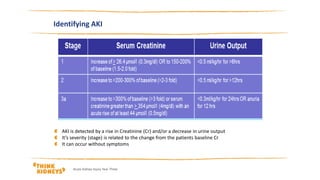
- AKI is a spectrum of injury that can lead to renal failure if unrecognized. It is identified by rises in creatinine and decreases in urine output.
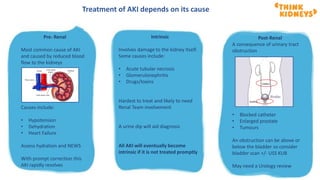
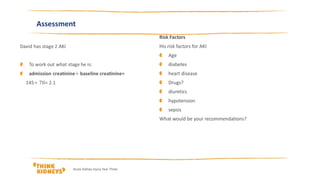
- Patients with chronic conditions, sepsis, hypotension, or those on certain medications are at higher risk. Causes include reduced renal blood flow (pre-renal), direct kidney damage (intrinsic), or urinary tract obstruction (post-renal).
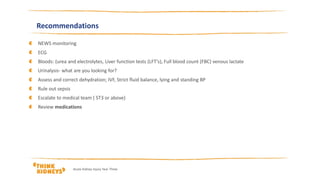
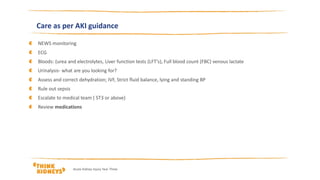
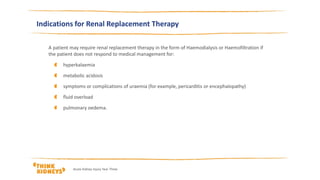
- For patients with AKI, nurses should monitor vital

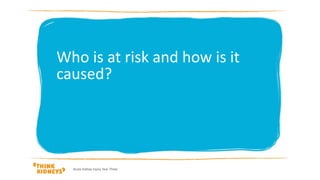
![chronic kidney disease
heart failure
liver disease
diabetes
history of acute kidney injury
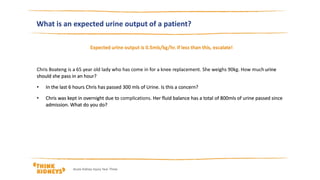
oliguria (urine output less than 0.5 ml/kg/hour)
Hypovolaemia
Sepsis
deteriorating early warning scores
(NICE Guideline NG148, 2019)
Acute Kidney Injury Year Three
Risk factors
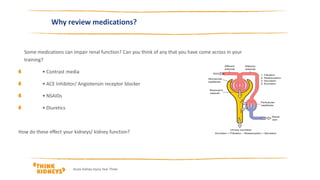
Drugs can also affect kidney function, these
include:
NSAIDs,
angiotensin-converting enzyme [ACE]
inhibitors,
angiotensin II receptor antagonists [ARBs] and
diuretics within the past week, especially if
hypovolaemic
use of iodinated contrast agents
symptoms or history of urological obstruction, or
conditions that may lead to obstruction
Age 65 years or over
Are any of your patients at risk??](https://image.slidesharecdn.com/ugnursesyearthreefinalreviewedoct2020-201020104915/85/Undergraduate-nurses-year-three-FINAL-reviewed-October-2020-12-320.jpg)