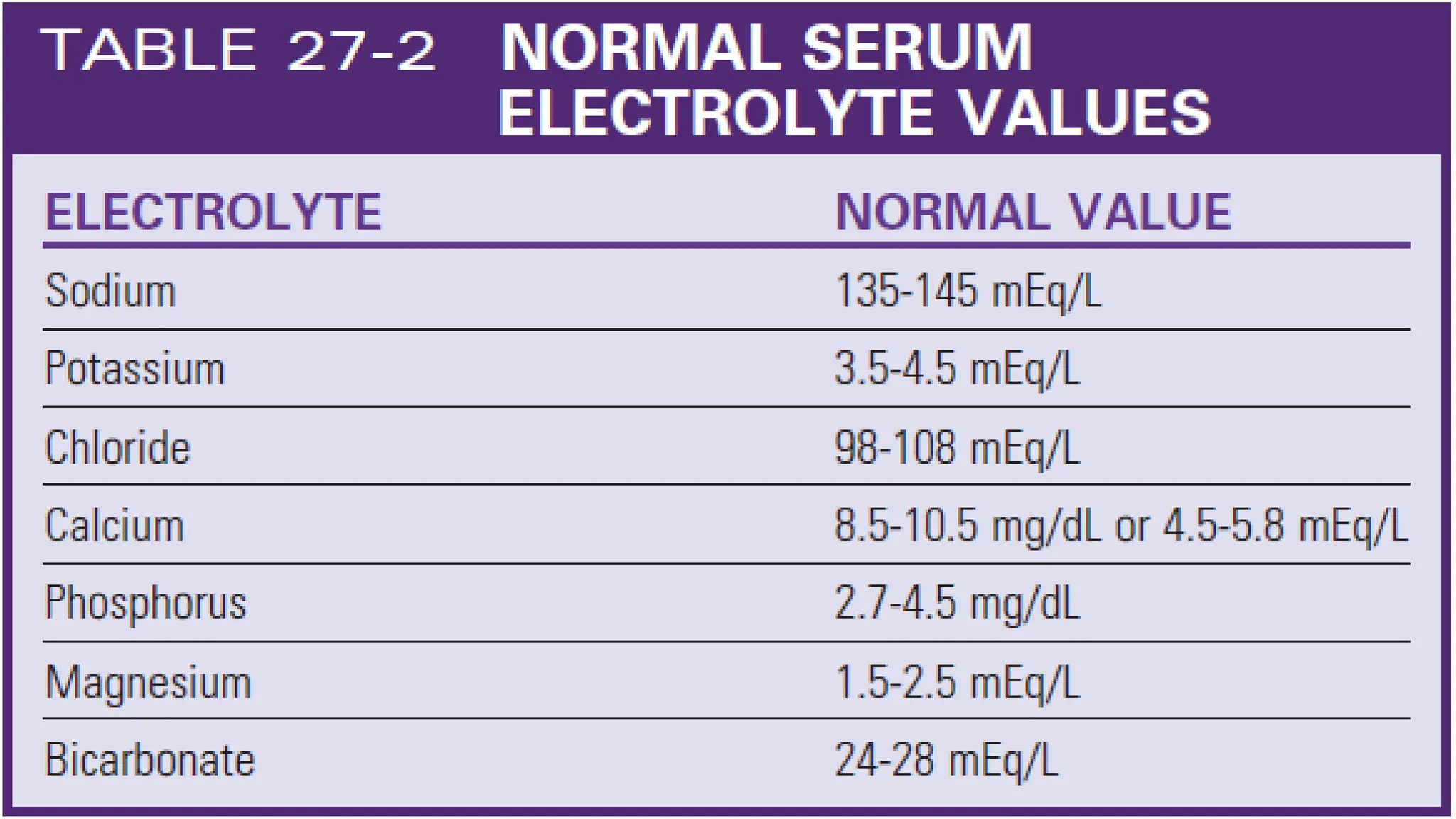
This document discusses acute kidney injury (AKI), including defining AKI, explaining the causes and pathophysiology, differentiating between the three types (prerenal, intrarenal, postrenal), describing diagnostic tests and clinical manifestations, discussing management, and listing nursing diagnoses. It provides objectives for understanding AKI, its causes, urine production in AKI, and differentiating between types of AKI based on history, exams, labs, and tests. Critical topics covered include the effects of critical illness, heart failure, respiratory failure, sepsis, and trauma on AKI as well as management strategies focused on fluid balance, electrolytes, nutrition, and renal replacement therapy.