Necrotising periodontal diseases
- 2. • Introduction: • Necrotizing ulcerative gingivitis (NUG) , necrotizing ulcerative periodontitis(NUP), necrotizing stomatitis (NS) are the most severe inflammatory periodontal disorders caused by plaque bacteria. • They are rapidly destructive & debilitating & represents various stages of same disease process (Horning & Cohen 1995). 1986 – Necrotizing ulcerative gingivoperiodontitis 1989 – NUP ( World workshop of Clinical Periodontics ) 1999 – Classification of Periodontal Diseases – NUG & NUP , included under the broader classification of Necrotizing Ulcerative Periodontal Diseases
- 3. A distinction between these diseases has not always been made in the literature
- 4. • Ulceromembranous gingivitis • Trench mouth (Pickard 1973) • Vincent’s gingivostomatitis • Phagedenic gingivitis • Fusospirallary periodontitis • Plaut-Vincent stomatitis
- 5. • Fourth century BC, Xenophon mentioned that Greek soldiers were affected with “sore mouth” and foul-smelling breath • In 1778, John Hunter described the clinical findings and differentiated ANUG from scurvy and chronic destructive periodontal disease • ANUG occurred in epidemic form in the French army in the 19th century
- 6. • In 1886, Hersch, a German pathologist, discussed some of the features associated with the disease such as enlarged lymph nodes, fever, malaise and increased salivation • In 1890s, Plaut and Vincent described the disease and attributed its origin to fusiform bacilli and spirochetes
- 7. NUG often occurs in groups in an epidemic form. During world war I & II “ epidemics “ broke out among the allied troops. Epidemic like outbreaks have also occurred among civilian populations. In developing countries, the prevalence of NPD is higher than in the industrialized countries, & the disease frequently affects the children. In India, 54- 68 % of NPD cases occurred in children below 10 yrs of age.( Migliani& Sharma 1965; Pindborg et al 1996). NUG occurs at all ages, with the highest incidence reported between ages 20 & 30 yrs & ages 15 -20 yrs.
- 8. • The disease seems to occur slightly more among HIV infected individuals. Studies among groups of HIV infected individuals have revealed prevalence of NPD between 0 & 27.7%. (Holmstrup & Westergaard1994; Reichart et al 2003). • NP was found in 1% of 200 HIV seropositive individuals (Riley et al 1992) & the prevalence may not in fact, differ from much of the general population ( Drinkard et al 1991 );This is particularly true after introduction of antiretroviral therapy. HAART resulted in decline of incidence & prevalence of oral conditions associated with HIV • Among HIV+ individuals, NPD is more in intravenous drug abusers than non-intravenous drug abusers. ( Ranganathan et al, 2012)
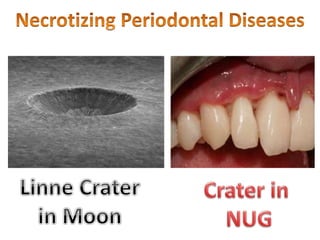
- 9. Clinical features - Oral signs • NG – an inflammatory destructive gingival condition, characterized by ulcerated and necrotic papilla and gingival margins. Punched out crater like depressions at the crest of the interdental papillae is a characteristic feature. • The surface of the craters is covered by a gray pseudomembranous slough. The sloughed material has little coherence and is composed of fibrin, necrotic tissue, RBC,WBC, Bacteria. • Linear erythema demarcating marginal necrosis and the relatively unaffected zone • In some cases the lesions are denuded of the surface pseudomembrane, exposing the gingival margin which is red, shiny, & hemorrhagic. The characteristic lesion may progressively destroy the gingiva & underlying periodontal tissues.
- 10. Initial punched out lesion
- 11. • Spontaneous gingival hemorrhage or pronounced bleeding after the slight stimulation are characteristic clinical signs. • A characteristic & pronounced foetor ex ore is often associated with this disease . Although it is not always very noticeable. • Increased salivation. • The palatal/lingual gingiva Is less frequently involved than the facial gingiva • Frequently gingiva of partially impacted tooth are also affected.
- 12. In NUP: Progression of the interproximal lesion often results in destruction of the interdental alveolar bone. Sequestrum formation: necrosis of a small or large part of the alveolar bone, which is denoted as sequestrum. The bone fragment is initially immovable, later on it becomes loose. Sequestrum involves interproximal as well as facial or palatal cortical bone. Involvement of the alveolar mucosa : NS In severe malnutrition or immunocompromised individual as in HIV, the necrotic process progresses beyond the mucogingival junction affecting the alveolar mucosa. It may result in extensive denudation of the bone – leading to major sequestration – with the development of oroantral fistula and osteitis.
- 13. Oral Symptoms • The lesion is extremely sensitive to touch, & the patient may often complains of a constant radiating, gnawing pain that is often intensified by eating spicy or hot foods & chewing. • There is metallic foul taste & an excessive amount of pasty saliva.
- 14. Extra oral & systemic signs & symptoms In mild & moderate stages of disease Local lymphadenopathy & slight elevation in temperature. In severe cases High fever, increased pulse rate, leucocytois, loss of appetite & general lassitude. Systemic reactions are more severe in children. Insomnia, constipation, gastro-intestinal disorders, headache, & mental depression sometimes accompany the condition. In very rare cases, severe squeal such as gangrenous stomatitis & noma have been described.
- 15. CLINICAL COURSE OF THE DISEASE BY PINDBORG et al Stage 1: Erosion of only tip of interdental papilla Stage 2: marginal gingiva affected and complete loss of interdental papilla Stage 3: Involving attached gingiva Stage 4: Exposure of bone
- 16. Stages of oral necrotizing disease – by Horning & Cohen • Stage 1- necrosis of the tip of the interdental papilla. • Stage 2- necrosis of entire papilla • Stage 3- necrosis extending to the gingival margin. • Stage 4- necrosis extending to the attached gingiva. • Stage 5– necrosis extending to labial & buccal mucosa. • Stage 6- necrosis exposing alveolar bone. • Stage 7– necrosis perforating skin of cheek.
- 17. ETIOLOGY It includes, • Role of microorganism • Role of host response • Predisposing factors includes 1. Local predisposing factor 2. Systemic predisposing factor
- 18. ROLE OF BACTERIA • Plaut & Vincent introduced the concept that NUG is caused by specific bacteria ; fusiform bacillus & spirochetal organism. • Loesche et al described a predominant constant flora & a variable flora associated with NUG. The constant flora is composed of prevotella intermedia, treponema sp, selenomonas sp, & fusobacterium sp. The variable flora consists of heterogeneous array of bacterial types. • The bacteriologic findings have been supported by immunologic data from Chung et al. - reported increased antibody titers for spirochetes & P.intermedia in NUG patients compared with titers in those with chronic gingivitis & healthy controls.
- 19. • Borrelia, gram positive cocci, b-hemolytic streptococci & Candida albicans have been isolated from the lesions of HIV associated NUP.(Reichart & Schiodt 1989). • It has also been proposed that human cytomegalovirus may play a role in the pathogenesis of NPD. (Sabiston 1986).
- 20. Pathogenic potential of microorganism • An important aspects in the pathogenesis is the capacity of the microorganism to invade the host tissues. • Among the bacteria isolated from necrotizing lesions, spirochetes & fusobacterium can in fact invade the epithelium. (Heylings 1967). • The spirochetes can also invade the vital connective tissue (Lisgarten 1965). • The pathogenic potential is further substantiated by the fact that both fusobacterium & spirochetes can liberate endotoxins (Kristoffersen et al).
- 21. • Gram negative bacteria liberate endotoxins in close contact with connective tissue. Endotoxins may produce tissue destruction both by direct toxic effects & indirectly by activating & modifying tissue responses of the host.(Wilton & Lehner 1980) • Indirectly endotoxins contribute to tissue damage in several ways; – They can function as antigens & elicit immune reactions. – They can activate compliment directly through the alternative pathway & thereby liberate chemotoxins.
- 22. • Fusobacterium & Spirochetes are found in moderate numbers of other oral diseases, as well as in apparently healthy mouths suggests that predisposing factors are essential to the development of NUG. • The disease has never been produced experimentally in either human beings or animals simply by oral inoculation of materials from lesion in patients with disease. (Schwartz & Grossman). • King also attempted to produce disease in his own mouth by inoculation of infected material but he was unsuccessful even after traumatizing gingiva & the organism promptly disappeared. • But he did show characteristic signs of ANUG however after he became ill with several colds, a short time later.
- 23. ROLE OF HOST RESPONSE • Regardless of whether specific bacteria are implicated in the etiology of NUG, the presence of these organism is insufficient to cause the disease. • The role of an impaired host response in NUG has long been recognized. • It is particularly evident for HIV-infected patients that the disease is associated with diminished host resistance; among other predisposing factors, the basic mechanism may include altered host immunity. • Changes in leukocyte function & the immune system have been observed.(Johnson & Engle et al)
- 24. • NUG is not found in well nourished individuals with a fully functional immune system. All the predisposing factor for NUG is associated with immunosuppresion. • Cohen et al described a depression in host defense mechanism particularly in PMN. • Total leukocyte count have been found to be similar for patients & controls. Patients with NG shows marked depression in polymorphonuclear leukocyte chemotaxis & phagocytosis as compared with control individuals. • Reduced proliferation of peripheral blood lymphocytes has also been found in those patients. • It was also suggested that elevated levels of blood steroids may account for the reduced chemotactic & phagocytic responses.
- 25. LOCAL PREDISPOSING FACTORS • It includes poor oral hygiene, preexisting gingivitis , injury to gingiva, & smoking • It may also occur in disease free mouth, it most often occurs superimposed on preexisting chronic gingival disease & periodontal pockets. • Areas of gingiva traumatized by opposing teeth in malocclusion – may predispose to NUG. • Pindborg et al – 98% of his patients with NUG were smokers & that the frequency of disease increases with an increase exposure to smoke.
- 26. Systemic predisposing factors • It includes – nutritional deficiency (malnutrition), – debilitating diseases, – fatigue caused by chronic sleep deficiency, – psychological stress, – immunodeficiency, – other health habits like alcohol & drug abuse.
- 27. MALNUTRITION • Malnutrition results in lowered tissue resistance - most common public health problem affecting children who are most often affected by NPD. (Enwonwu 1985, 1994). • Malnutrition is characterized by marked tissue depletion of the key antioxidant nutrients, & impaired acute phase reactions to the infections. This is due to impairment in the production & cellular action of cytokines. • Malnutrition – defective mucosal integrity, hormonal imbalance. • Malnutrition usually involves concomitant deficiencies of several essential macro & micronutrients, & therefore has the potential to adversely influence the prognosis of periodontal infections. (Enwonwu 1994).
- 28. Debilitating disease • Debilitating systemic disease may predispose the patient to the development of NUG. • It includes chronic disease ( eg. Syphilis, cancer), severe gastrointestinal disorders such as ulcerative colitis, blood dyscracias (anemia , leukemia) & acquired immunodeficiency syndrome. • Nutritional deficiency resulting from debilitating disease may be an additional pre disposing factor. • Ulceronecrotic lesions appear in the gingival margins of hamsters exposed to total body irradiation.(Mayo J et al)
- 29. PSYCHOSOMATIC FACTORS Psychological factors appear to be important in the etiology of NUG. The disease often occur with association with stressful situation (Induction in to armed forces, examination periods, emotional disorders, patients feeling inadequate at handling life situations). Cohen – Cole et al – psychiatric disturbance and the impact of negative life events may lead to activation of hypothalamic- pituitary adrenal axis resulting in elevation of cortisol levels. Reduced gingival microcirculation & salivary flow - depressed neutrophil & lymphocyte functions which facilitate bacterial invasion & damage.(Johnson et al)
- 30. • The mechanisms whereby psychological factors create or predispose to gingival damage have not been established, but alterations in digital & gingival capillary response suggestive of increased autonomic nervous activity have been demonstrated in patients with ANUG.
- 31. Smoking • The relationship between tobacco usage & NPD appears to be complex. • Smokers in general poorer oral hygiene than the non smokers. • Smoking could lead to increased disease activity by influencing host response & tissue reactions. As examples, smokers have depressed numbers of T- helper lymphocytes, & tobacco smoke can also impair chemotaxis and phagocytosis of oral & peripheral phagocytes.( Lannan et al 1992, Selby et al 1992) • Nicotine- induced secretion of epinephrine resulting in gingival vasoconstriction – possible mechanism by which smoking may influence tissue susceptibility.( Bergstrom & Preber 1986)
- 32. HIV infection • HIV infection attacks the T- helper cells of the body, causing drastic change in the T-helper (CD4+)/T-suppressor(CD8+) ratio with severe impairment of the host resistance to infection. • Depleted T- helper lymphocyte counts correlate closely with the occurrence of NG as demonstrated in the study of 390 US HIV seropositive soldiers (Thompson et al 1992). • In HIV-positive patients, NPD are more frequent and show faster progression, although no differences have been detected between the characteristics of the disease in HIV-negative and HIV-positive patients. It has been suggested that HIV-positive patients have a higher tendency for recurrence and a diminished response to both mechanical and/or pharmacological periodontal treatment Novak Mj (1999)
- 33. HISTOPATOLOGICAL FEATURE Histopathologically, NG lesions is characterized by ulceration with necrosis of epithelium & superficial layers of the connective tissue & an non specific inflammatory reaction. The surface epithelium is destroyed & replaced by a meshwork of fibrin, necrotic epithelium, PMNs & various types of microorganism. This appears clinically as the surface pseudomembrane. Below this necrotic pseudomembrane, the epithelium is edematous, & the individual cells exhibit varying degrees of hydropic degeneration.
- 34. • The underlying connective tissue is extremely hyperemic with numerous engorged capillaries & dense infiltration of PMNs. This acutely inflamed zone appears clinically as the linear erythema. • Numerous plasma cells may appear in the periphery of the infiltrate. This is interpreted as an area of established chronic gingivitis on which acute lesion is superimposed.
- 35. RELATION OF BACTERIA TO THE CHARACTERISTIC LESION • The light microscope & the electron microscope have been used to study the relationship of bacteria to the characteristic lesion of NUG. LISGARTEN(1965) described the following four zones which blend with each other & may not all be present in every case; • Zone1 – bacterial zone • Zone 2 – neutrophil rich zone • Zone 3 – necrotic zone • Zone 4 – zone of spirochetal infiltration
- 36. Electron micrograph demonstrating phagocytosing (N)neutrophil close to the surface of a sequestrum, numerous spirochetes and rods.
- 37. DIAGNOSIS • The diagnosis of NG, NP, NS is based on clinical findings as described above. • The histopathology of the necrotizing disease is not pathognomonic of NG & biopsy is not certainly indicated. • Bacterial studies are useful in the differential diagnosis of NUG & specific infections of oral cavity.
- 38. Diagnostic essentials for NUG • Lesions are painful. • Lesions are gingival ulcers, punched out crater like of interdental papilla & may involve marginal gingiva. • Non essential clinical features of NUG the absence which does not preclude the diagnosis of NUG • Pseudomembrane of sloughed necrotic debris & bacteria covering the ulcerated area. • Foetor ex ore. • Fever, malaise & lymphadenopathy
- 39. Differential diagnosis • Herpetic gingivostomatitis • Desquamative gingivitis • Streptococcal gingivostomatitis • Apthous stomatitis • Candidiasis • Agranulocytosis • Gonococcal gingivostomatitis • Tuberculous gingival lesion
- 40. Important characteristics for differential diagnosis between NPD & PHG NPD PHG Etiology Bacteria Herpes simplex virus Age 15-30 Frequently children Site Interdental papilla. Rarely outside the gingiva Gingiva and entire oral mucosa Symptoms •Ulcerations and necrotic tissue and a yellowish –white plaque •Fetor ex ore •Moderate Fever may occur •Multiple vesicles which disrupt, leaving small round fibrin covered ulcerations •Fetor ex ore •Fever Duration 1-2 days if treated 1-2weeks Contagious - + Immunity - Partial Healing Destruction of periodontal tissue remains No permanent destruction
- 41. TREATMENT • The treatment of necrotizing periodontal disease is divided into two phases, 1)acute phase treatment 2)maintenance phase treatment ACUTE PHASE TREATMENT • The aim is to eliminate the disease activity as manifest by ongoing tissue necrosis developing laterally & apically. • It is also to avoid pain & general discomfort which may severely compromise food intake.
- 42. FIRST VISIT • General examination of the patient • The oral cavity is examined for the characteristic feature of NUG, its distribution & possible involvement of oropharyngeal region. • Oral hygiene is evaluated with special attention to the presence of pericoronal flaps, periodontal pockets & local factors. • History taking – H/o present illness, diet, socio-economic background, diet, smoking, chances of HIV infection, stress, profession. Treatment during initial visits includes, • It is mainly confined to the acutely involved areas • After application of topical anesthetics, the pseudomembrane & non attached surface debris is removed using a moistened cotton pellet.
- 43. • After the area is cleansed with warm water supragingival calculus is removed using ultrasonic scalers. • Subgingival scaling & curettage is contraindicated at this time. • Procedures such as extractions or periodontal surgery are postponed until the patient has been symptom free for 4 weeks, to minimize the likelihood of exacerbating the acute symptoms. • Patients with moderate or severe NUG & local lymphadenopathy or systemic signs or symptoms are placed on an antibiotic regimen.
- 44. • First Choice : Metronidazole(250 mg) * TID (Loesche et al 1982) • Other antibiotics such as Amoxycillin(500mg) in every 6 hours for 10 days or erythromycin (500mg every 6 hrs) are used. • The adjunctive use of metronidazole in HIV associated NPD is reported to be extremely effective in reducing acute pain & promoting rapid healing.(Scully et al). • Topical application of antibiotics is not indicated in the treatment of NPD because intralesional bacteria are frequent &topical application does not results in sufficient intralesional concentration of antibiotics.
- 45. • Hydrogen peroxide & other oxygen releasing agents also have a long standing tradition in the treatment of NPD. • Hydrogen peroxide (3%) is used for debridement in necrotic areas & as a mouth rinse (equal portions 3% H2O2 & warm water). • Favorable effects of hydrogen peroxide may be due to mechanical cleaning,& the influence on anaerobic bacterial flora of the liberated oxygen. (Macphee & Cowley 1981). • Further adjunctive local Oxygen therapy of NPD showed a more rapid clinical restitution with less periodontal destruction than in a group without oxygen therapy. (Gaggl et al 2006)
- 46. Twice daily rinsing with a 0.2% chlorhexidine solution is a very effective adjunct to reduce plaque formation, when particularly tooth brushing is not performed. It also assists self performed oral hygiene during the first weeks of treatment. Appropriate treatment alleviates symptoms with in few days.(5 days) Physical rest advised. Brushing instructions Second visit Systematic subgingival scaling should be continued with increasing intensity as the symptoms subside. Correction of restoration margins Polishing of restorations & root surfaces should be completed after healing of ulcers. When ulcerated areas are healed local treatment is supplemented with oral hygiene & patient motivation.
- 47. • Third Visit: • Approximately 5 days after 2nd visit • Patient counseling : Nutrition, Smoking cessation • H2O2 rinse discontinued • CHX maintained for 2-3 weeks • Maintenance Therapy Suspected seropositive NPD patients, who are unaware of their serostatus , should be referred to the physicians.
- 48. Supportive systemic treatment • In addition to systemic antibiotics, supportive treatment consists of copious fluid consumption & administration of analgesics for relief of pain. • Bed rest is necessary for the patients with systemic complication such as high fever, malaise, anorexia & general debility.
- 49. Nutritional supplements The rationale for the nutritional supplements in the treatment of NUG is based on the following; • 1) lesions resembling those of the ANUG have been produced experimentally in animals with nutritional deficiencies. • 2) isolated clinical studies report fewer recurrences when local treatment of NUG is supplemented with vitamin B & vitamin C. (Linghorne WJ et al) • And hence nutritional supplements may be indicated along with local treatment to ward off deficiencies of these vitamins.
- 50. MAINTENANCE PHASE TREATMENT On further visits, • When the acute phase treatment has been completed, necrosis & acute symptoms in NPD have disappeared. • The formerly necrotic areas are healed & the gingival craters are reduced in size, although some defects usually persists. • Bacterial plaque accumulates & therefore may predispose to recurrences of NPD or to further destruction because of a persisting chronic inflammatory process or both. • These sites therefore requires surgical correction.
- 51. • Shallow craters can be removed by simple gingivectomy, while the elimination of deep defects may require flap surgery. • Treatment of NG is not completed until all gingival defects have been eliminated & optimal conditions for future plaque control have been established. • Elimination of predisposing factors is also very important to prevent recurrences.
- 52. Persistent or recurrent cases • Adequate local therapy with optimal home care will resolve most cases of NUG. If it persists despite therapy or recurs , the patient should be revaluated with the focus on the following factors, • Reassessment of differential diagnosis to rule out the disease that resembles NUG. • Underlying systemic disease that cause immunosuppresion. • Inadequate local therapy. • Inadequate compliance
