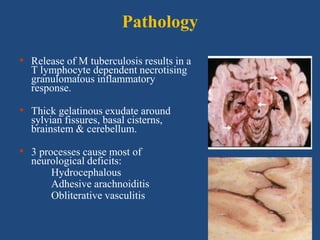
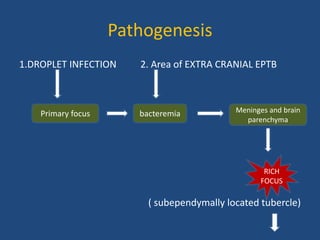
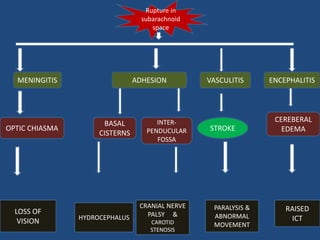
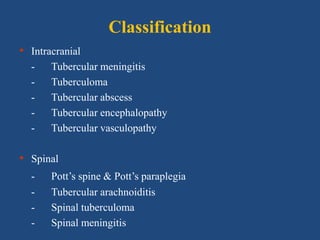
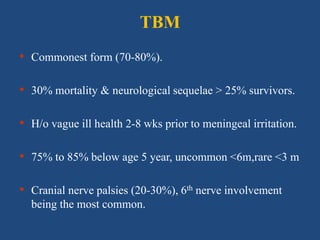
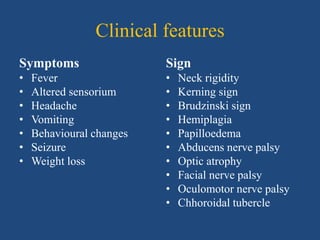
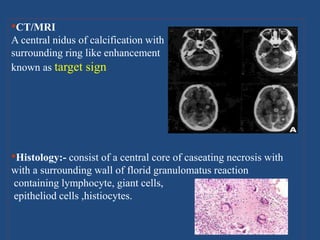
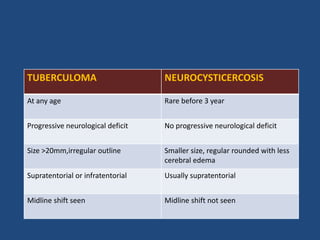
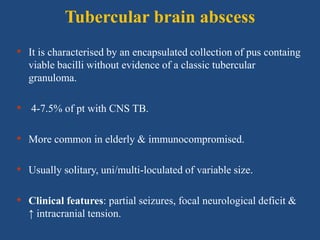
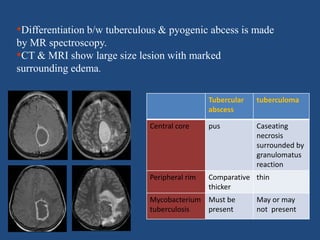
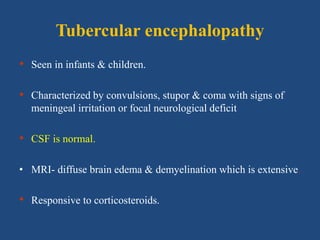
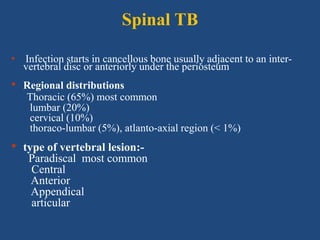
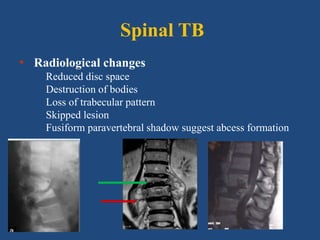
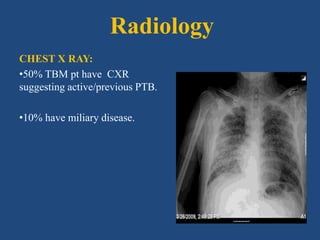
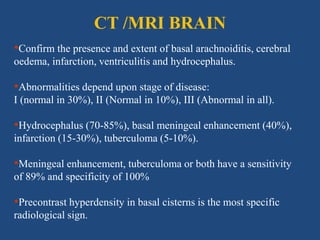
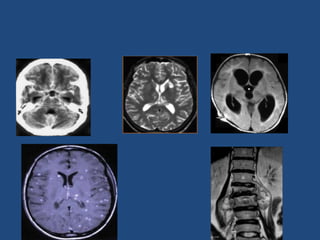
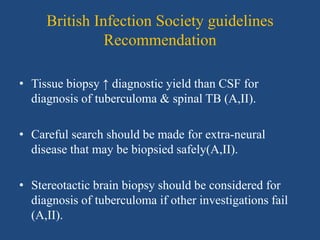
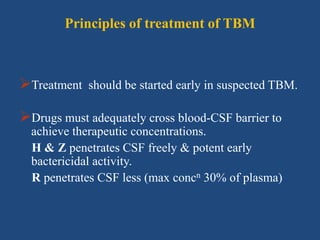
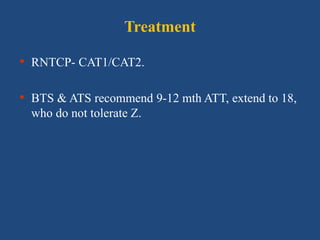
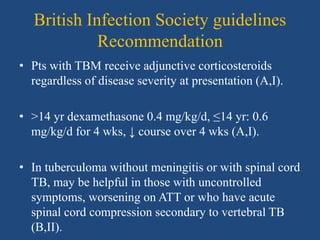
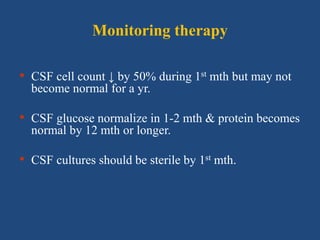
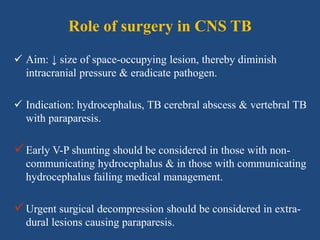
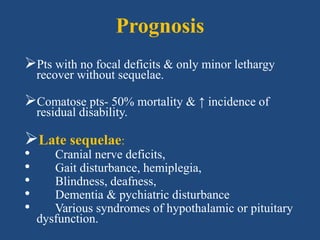
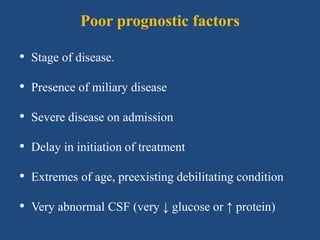
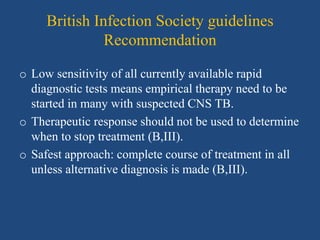
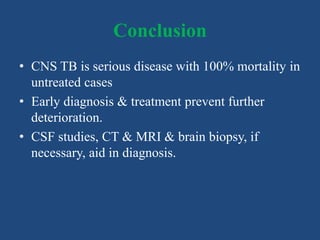
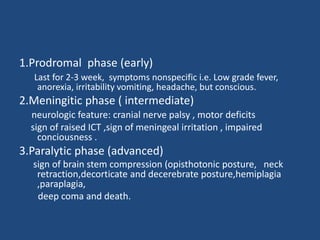
CNS tuberculosis is a severe manifestation of extrapulmonary tuberculosis, characterized by a high case fatality rate in untreated cases. The document discusses the etiology, pathogenesis, classification, diagnosis, and treatment methods for CNS tuberculosis, highlighting the critical importance of early detection and intervention. Key diagnostic techniques, clinical features, and potential complications are outlined, emphasizing the need for adjunctive steroid therapy and the role of surgery in certain cases.