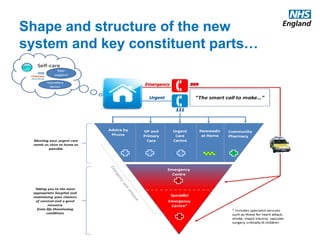
The document discusses proposals from the Urgent and Emergency Care Review in the UK to reform urgent and emergency care services. It outlines plans to provide more responsive urgent care outside hospitals, treat non-life threatening issues close to home, and ensure serious issues are treated in specialized centers. It also discusses expanding the role of community pharmacies, improving NHS 111, and creating Urgent Care Networks to better coordinate care across providers. The goal is to provide the right care, in the right place, first time for urgent and emergency patients.