States with Higher Mental Healthcare Capacity Have Lower Youth Suicide Rates
- 1. https://bibliu.com/app/#/view/books/9781259852275/epub/OEB PS/xhtml/17_baL6732X_ch03_036-055.html#page_43 Journal of Adolescent Health 70 (2022) 83e90 www.jahonline.org Original article Preventing Adolescent and Young Adult Suicide: Do States With Greater Mental Health Treatment Capacity Have Lower Suicide Rates? Evan V. Goldstein, Ph.D., M.P.P. a, Laura C. Prater, Ph.D., M.P.H., M.H.A. b, and Thomas M. Wickizer, Ph.D., M.P.H. c,* a Division of Health System Innovation & Research, Department of Population Health Sciences, University of Utah School of Medicine, Salt Lake City, Utah b Firearm Injury Prevention & Research Program, Harborview Medical Center, The University of Washington, Seattle, Washington c Division of Health Services Management & Policy, The Ohio State University College of Public Health, Columbus, Ohio Article history: Received December 30, 2020; Accepted June 17, 2021 Keywords: Gun violence; Suicide prevention; Adolescent suicide; Firearm suicide; Mental health A B S T R A C T IMPLICATIONS AND Purpose: Youth suicide is increasing at a significant rate and is the second leading cause of death for adolescents. There is an urgent public health need to address
- 2. the youth suicide. The objective of this study is to determine whether adolescents and young adults residing in states with greater mental health treatment capacity exhibited lower suicide rates than states with less treatment capacity. Methods: We conducted a state-level analysis of mental health treatment capacity and suicide outcomes for adolescents and young adults aged 10e24 spanning 2002e2017 using data from Centers for Disease Control and Prevention, U.S. Bureau of Labor Statistics, Federal Bureau of Investigation, and other sources. Multivariable linear fixed- effects regression models tested the relationships among mental health treatment capacity and the total suicide, firearm suicide, and nonfirearm suicide rates per 100,000 persons aged 10e24. Results: We found a statistically significant inverse relationship between nonfirearm suicide and mental health treatment capacity (p ¼ .015). On average, a 10% increase in a state’s mental health workforce capacity was associated with a 1.35% relative reduction in the nonfirearm suicide rate for persons aged 10e24. There was no significant relationship between mental health treatment capacity and firearm suicide. Conclusions: Greater mental health treatment appears to have a protective effect of modest magnitude against nonfirearm suicide among adolescents and young adults. Our findings under- score the importance of state-level efforts to improve mental health interventions and promote mental health awareness. However, firearm regulations may provide greater protective effects against this most lethal method of firearm suicide.
- 3. � 2021 Society for Adolescent Health and Medicine. All rights reserved. Conflicts of interest: The authors have no conflicts of interest to disclose. * Address correspondence to: Thomas M. Wickizer, Ph.D., M.P.H., Division of Health Services Management & Policy, 1841 Neil Avenue, Columbus, Ohio 43210. E-mail address: [email protected] (T.M. Wickizer). 1054-139X/� 2021 Society for Adolescent Health and Medicine. All rights reserved. https://doi.org/10.1016/j.jadohealth.2021.06.020 CONTRIBUTION The increase in youth sui- cide requires the develop- ment of more effective interventions. This study elucidates differences be- tween nonfirearm and firearm suicide to under- stand different prevention pathways. Mental health treatment capacity is important for nonfirearm suicide prevention, while firearm suicide prevention may be best addressed through firearm safety and storage policies. The U.S. is in the midst of a suicide epidemic taking the lives of almost 50,000 Americans each year, with rates increasing in every state from 1999 to 2016 [1]. Although suicide is the 10th
- 4. leading cause of death in the U.S. overall, it is the second leading mailto:[email protected] http://crossmark.crossref.org/dialog/?doi=10.1016/j.jadohealth.2 021.06.020&domain=pdf http://www.jahonline.org https://doi.org/10.1016/j.jadohealth.2021.06.020 E.V. Goldstein et al. / Journal of Adolescent Health 70 (2022) 83e9084 cause of death among adolescents and young adults aged 10e24 [1,2]. Adolescent and young adult suicides are increasing at a faster rate among young females compared to young males [3]; the firearm suicide rate among persons aged 14e24 increased by 54% since 2004 [4]. Among young adults aged 15e24, firearms, suffocation/hanging, and poisoning are the most frequently used suicide methods, respectively [5,6]. For persons younger than 15, suffocation is the most frequently used method, followed by firearms and poisoning [5]. For females aged 15%e24%, 45% of suicides were attributed to a firearm injury, 28% to suffocation, and 17% to poisoning [4]. Among males in the same age range, 53% of suicides were attributed to a firearm injury, 34% to suf- focation, and 8% to poisoning [4]. Beyond individual mortality, adolescent and young adult suicides have devastating social consequences. Among high-income countries in 2014, adoles- cent and young adult suicides accounted for an estimated loss of 406,730 years of potential life, 77% of which was attributable to the U.S., the country with the most significant adolescent and young adult suicide problem [7]. Researchers have found individual and household factors associated with the risk of suicide among adolescents and
- 5. young adults. At the household level, family discord and parental divorce are associated with increased risk of adoles - cent suicide [3]. Access to firearms in the home is associated with higher suicide rates [8], while greater social support and public welfare expenditures appear to have a protective effect [9]. Suicide rates are higher among male youth compared to female youth, but suicidal ideation is more common among female youth [10]. Male adolescents are also more likely than females to use firearms in lethal suicide attempts [3]. White adolescents have experienced higher suicide rates than nonwhite adolescents [10], despite recent rising rates among black youth [11]. Those who report same-sex sexual orientation are also at greater risk for suicide [12]. Mental illness, especially depression, has been associated with increased risk of adoles - cent suicide [13]. Unfortunately, many suicides occur prior to uncovering mental illness [14], making the suicide attempt the first sign of distress. With firearms accounting for so many U.S. suicide deaths, many public policy efforts have focused on limiting access to firearms through state-level regulatory restrictions. In general, the academic literature demonstrates that stricter firearm laws, such as policies aimed at regulating the supply of firearms through background checks and mandatory waiting periods before firearm issue, are associated with lower firearm fatality rates [15,16]. Evidence predating the recent spike in adolescent suicides demonstrated that child access prevention laws reduced the rate of youth firearm suicide, and offered some protective effect on firearm suicide for older members within the household by limiting access to firearms [17]. Meaningful firearm safety and control policies remain controversial and difficult to enact even at the state level, despite states’ authority to do so [18]. Beyond firearm regulation, much public attention has focused
- 6. on mental health treatment interventions to reduce youth sui - cide. However, studies examining the effectiveness of these in- terventions have been limited by power issues and small sample sizes [19]. Substance abuse, interpersonal trauma, and mental illness are known risk factors strongly linked to suicide attempts among younger persons [13,20], but studies have shown promise that primary care-based interventions, adequate outpatient care, and access to ongoing mental healthcare may reduce youth suicide [21,22]. Prior research also suggests the assessmen- t/restriction of lethal means (i.e., firearms, medications) and counseling by clinicians can reduce lethal suicide attempts among adults and may improve opportunities to detect and treat mental health conditions [23e26], but knowledge is more limited for youth. Mental healthcare shortages are well-documented across the U.S., and many families find it difficult to access child or adolescent mental health clinicians. Prior research [27] has demonstrated an association between access to mental health- care and reduced risk of suicide among persons of all ages, including one recent study suggesting that living in a federally designated mental health professional shortage area was corre- lated with suicide death [28]. But less is known about the pro- tective effects of mental health services for suicide among adolescents and young adults. To our knowledge, there has not been a comprehensive state-level analysis of mental health treatment capacity and suicide rates among adolescents and young adults. The severity of youth suicide in the U.S., and the fact that states have significant power to fund and design their mental healthcare systems and enact firearm safety and control pol- icies, prompted this state-level analysis examining the rela- tionship between mental health treatment capacity and suicide. Using data from 2002 to 2017, we examined whether states
- 7. with greater mental health treatment capacity have lower sui - cide rates among adolescents (aged 10e19) and young adults (aged 20e24), including both firearm and nonfirearm suicide rates, compared with states having less treatment capacity. Methods Data and study design Our analysis merged data from multiple sources. The pri- mary data sources were the Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System (WISQARS) [4], an interactive database that compiles information on fatal and nonfatal injury and violent death in the U.S., and the Bureau of Labor Statistics (BLS) Occupational Employment Statistics program, which produces state-level, longitudinal employment data for nearly 800 occu- pations. Additional data sources included the American Com- munity Survey and Current Population Survey from IPUMS, Kaiser Family Foundation State Health Facts database, Federal Bureau of Investigation National Instant Criminal Background Check System, U.S. Census Bureau Historical Poverty Tables, and the Urban Institute State and Local Finance initiative. We performed a state-level, time-series cross-sectional analysis that took advantage of natural variation between states and over time in our variables of interest. The state-year was the unit of analysis, which is appropriate because states have authority over the funding, design, and regulation of their mental healthcare systems, as well as firearm safety and control regulation. The final analytic file contained 186 observations spanning four time periods: t ¼ 2002, 2007, 2012, and 2017. Dependent variables
- 8. Our first dependent variable measured total intentional suicide among adolescents (aged 10e19) and young adults (aged 20e24). E.V. Goldstein et al. / Journal of Adolescent Health 70 (2022) 83e90 85 Our second and third dependent variables measured intentional firearm and nonfirearm suicide, respectively, among adolescents and young adults. Because the CDC recognizes suicide as a leading cause of death among persons up to age 24 [1], we extracted crude rates of annual suicides per 100,000 persons aged 10e24 from the WISQARS Fatal Injury database for the three dependent variables [4]. CDC data restrictions prevent the analysis of state-level suicide rates involving less than 10 decedents. For this reason, for each dependent variable, we combined the annual suicide rates for each time period and its preceding year to develop an average rate for the 2-year period. Following this process, we excluded state- years from the analysis if the 2-year average suicide rate for any dependent variable was still constructed from less than 10 de- cedents. Excluded state-years were Connecticut (2012), Delaware (2002, 2007), Hawaii (2002, 2007, 2017), Massachusetts (2012), New Hampshire (2012), Rhode Island (all years), Vermont (2002, 2007), and Washington, DC (all years), representing 8.8% of all possible state-years. Independent variables
- 9. We had one independent variable: mental health treatment capacity, measured as the annual mental health workforce size for each state-year. To construct this measure, we extracted occupa- tional (OCC) codes gathered from the Occupational Employment Statistics database [29]. OCC codes 19-3031 (clinical, counseling, and school psychologists), 21-1011 (substance abuse and Table 1 Characteristics of the analytic sample: 2002e2017 2002 2007 Total suicide rate per 100,000 (2-year averages) 8.5 (3.2) 8.6 Firearm suicide rate per 100,000 (2-year averages) 4.8 (2.4) 4.3 Nonfirearm suicide rate per 100,000 (2-year averages) 3.7 (1.3) 4.4 Mental health practitioners per state, in 1,000s 10.6 (10.5) 12.4 Annual FBI firearm background checks per state, in 100,000s
- 10. 1.8 (1.5) 2.4 State population, in 100,000s 61.6 (64.6) 64.5 Race (% of population) White 80.6% (10.1) 79.3% Black 10.3% (9.7) 10.4% Male (% of population) 49.0% (.8) 49.4% Adult population with high school diploma (%) 83.9% (4.1) 86.0% Population reporting divorced marital status (%) 7.9% (1.2) 8.0% Per capita public expenditure on parks, recreation, and libraries $175.3 (63.7) $185.2 State unemployment rate 5.2% (1.0) 4.6% Population living below poverty (%) 11.8% (3.2) 11.9% Affordable Care Act Medicaid expansion Expansion not yet adopted 46 0% 46 State adopted expansion 0 100% 0 Observations 46 46
- 11. Authors’ analysis of data from the Web-based Injury Statistics Query and Reporting S Population Survey from IPUMS CPS, Federal Bureau of Investigation (FBI) National Insta initiative, U.S. Census Bureau, and Kaiser Family Foundation, 2002e2017. For each var included in the analytic. Standard deviations are shown in parentheses for continuou States could enact the Affordable Care Act Medicaid expansion beginning in 2014. behavioral disorder counselors), 21-1014 (mental health coun- selors), 21-1022 (medical and public health social workers), 29- 1066 (psychiatrists), 31-1013 (psychiatric aides), and 21-1023 (mental health and substance abuse social workers) were used to construct the variable for each state-year in the analytic sample. Covariates We included covariates in our statistical models to adjust for potential confounding factors. We used data from the Bureau of Labor Statistics, U.S. Census Bureau, and American Community Survey to adjust for state-level, temporal differences in unem- ployment rate, poverty rate, and educational attainment, race, and gender compositions. Our models adjusted for the total population of each state across time to account for population-to size-related variation in mental health workforce capacity. We included data from the Current Population Survey to adjust for the percentage of people in each state-year who reported “divorced” for their marital status. To adjust for state-level dif- ferences in the availability of social support resources, we used data from the Urban Institute to construct a proxy measure of the per capita public expenditure on parks, recreation, and libraries. Because the Affordable Care Act Medicaid expansion may have been associated with reductions in suicide by improving access to healthcare [30], we included data from Kaiser Family Foun-
- 12. dation to adjust for whether states enacted the Affordable Care Act Medicaid expansion. Finally, we included dummy variables 2012 2017 (3.8) 10.1 (3.6) 12.5 (5.1) (2.3) 5.0 (2.6) 6.3 (3.4) (1.8) 5.1 (1.9) 6.2 (2.3) (13.1) 12.9 (14.5) 14.8 (15.8) (2.6) 4.1 (4.5) 5.1 (7.3) (67.6) 65.3 (72.0) 67.1 (73.9) (10.4) 77.2% (13.0) 77.4% (10.7) (9.6) 10.8% (9.9) 10.8% (9.7) (.8) 49.4% (.8) 49.4% (.8) (3.7) 87.9% (3.2) 89.5% (2.7) (1.1) 8.5% (1.3) 8.6% (1.4) (73.2) $175.4 (61.6) $179.4 (76.4) (.9) 7.7% (1.6) 4.4% (.9) (2.9) 14.5% (3.3) 12.1% (2.9) 0% 46 0% 19 39.6% 100% 0 100% 29 60.4% 46 48 ystem (WISQARS) Fatal Injury system, American Community Survey and Current nt Criminal Background Check System, the Urban Institute
- 13. State and Local Finance iable, unadjusted average percentages or counts per year are shown for the states s variables, and percentages are shown in parentheses for categorical variables. Table 2 National suicide and crude death rates by year and age group: 2002e2017 Panel A: ages 10e19 Year Total suicide rate per 100,000, ages 10e19 Firearm suicide rate per 100,000, ages 10e19 Nonfirearm suicide rate per 100,000, ages 10e19 Crude death rate per 100,000, ages 10e19 (all causes) 2002 4.23 1.98 2.25 42.85 2007 3.87 1.59 2.28 39.00 2012 4.97 2.05 2.92 30.79 2017 7.18 3.09 4.09 33.65 Panel B: ages 20e24 Year Total suicide rate per 100,000, ages 20e24
- 14. Firearm suicide rate per 100,000, ages 20e24 Nonfirearm suicide rate per 100,000, ages 20e24 Crude death rate per 100,000, ages 20e24 (all causes) 2002 12.33 6.65 5.68 95.01 2007 12.62 6.03 6.59 98.13 2012 13.68 6.47 7.21 84.61 2017 17.04 8.38 8.66 95.57 National suicide rates were obtained from the CDC Web-based Injury Statistics Query and Reporting System (WISQARS) Fatal Injury Reports and crude death data were obtained from the CDC WONDER database. Crude rates per 100,000 shown. CDC ¼ Centers for Disease Control and Prevention. E.V. Goldstein et al. / Journal of Adolescent Health 70 (2022) 83e9086 for each time period and each state to adjust for secular time trends and unmeasured, time-invariant state-level policies and characteristics. Firearm availability is associated with suicide [31], but we were unable to directly control for it. Consistent measures of firearm availability are not available at the state level for all states. As recommended elsewhere [32], we included the mea- sure of annual federal firearm background checks from the Federal Bureau of Investigation National Instant Criminal Back- ground Check System as a proxy for gun ownership rates in the Table 3 Highest and lowest total suicide rates per 100,000, by state and
- 15. year: 2002e2017 2002 States with highest ratesa Total suicide rate per 100,000 Alaska 19.78 Wyoming 17.84 South Dakota 14.19 Idaho 12.56 Montana 12.33 New Mexico 11.64 Colorado 11.37 Arizona 10.96 Kansas 10.41 New Hampshire 10.39 2017 States with highest ratesa Total suicide rate per 100,000 Alaska 32.81 Montana 23.48 South Dakota 23.12 Wyoming 19.72 North Dakota 18.81 New Mexico 18.63 Colorado 16.99 Oklahoma 16.60 Utah 16.37 Idaho 15.99 Authors’ analysis of data from the CDC Web-based Injury Statistics Query and Reportin average of crude firearm suicide rates for individuals aged 10e24 for each study time
- 16. observations were available in this analysis. For 2002 and 2017, we compared the av highest and lowest suicide rates using bivariate t-tests and Mann-Whitney U-tests. p a The states with the highest suicide rates had significantly greater federal firearm statistical models for total and firearm suicide rates, but not in the nonfirearm suicide rate model. Analysis We tested multivariable linear fixed-effects regression models to examine the relationships between mental health treatment capacity and suicide rates. Robust standard errors were clustered at the state level to correct for problems poten- tially caused by heteroscedasticity or serial correlation. To States with lowest rates Total suicide rate per 100,000 New Jersey 3.58 Massachusetts 4.41 California 4.42 New York 4.71 Connecticut 4.84 South Carolina 6.1 Illinois 6.31 Florida 6.54 Maryland 6.69 Virginia 6.71 States with lowest rates Total suicide rate per 100,000 New Jersey 5.54 New York 5.90 Connecticut 6.50 Massachusetts 6.56
- 17. California 6.83 Maryland 6.87 Delaware 7.58 Florida 8.17 Illinois 8.23 North Carolina 9.56 g System (WISQARS) Fatal Injury Reports. The total suicide variable is the 2-year period (and its preceding year), as described in the manuscript. Not all state-year erage federal firearm background checks per capita between the states with the < .01 using both tests. background checks per capita than the states with the lowest suicide rates. Table 4 Estimating the effects of greater mental health treatment capacity on suicides per 100,000 persons aged 10e24 1 2 3 Outcome: total suicides/100,000 persons Outcome: firearm suicides/100,000 persons Outcome: nonfirearm suicides/100,000 persons Mental health practitioners per state, in 1,000s �.073 �.021 �.052*
- 18. .106 .521 .015 Annual FBI firearm background checks, in 100,000s .025 .022 .430 .221 State population, in 100,000s �.009 �.007 �.003 .746 .706 .984 Race (%) White �.032 �.12 .083 .734 .136 .112 Black �.643* �.518þ �.131 .035 .077 .307 Male population (%) 1.192 .324 .866þ .162 .541 .069 Adult population with high school diploma (%) �.453** �.14 �.299** .005 .222 <.001 Population reporting divorced marital status (%) �.294 .047 �.335* .127 .693 .018 Per capita public expenditure on parks, recreation, and libraries .005 .003 .002 .361 .432 .432 Unemployment rate (state) .086 .062 .01 .653 .546 .931 Population living below poverty (%) .074 .026 .043 .544 .786 .376
- 19. Affordable Care Act Medicaid expansion Expansion not yet adopted Reference Reference Reference State adopted the expansion �.459 �.432 �.066 .448 .342 .849 Year 2002 Reference Reference Reference 2007 .843 �.339 1.138** .177 .348 <.001 2012 3.450** .583 2.847** <.001 .268 <.001 2017 7.272** 2.505** 4.666** <.001 .004 <.001 Constant .322 15.327 �15.783 .933 .543 .503 Observations 186 186 186 Adjusted R2 .69 .52 .69 p values are shown in italics below each coefficient. State fixed-effects (FE) coefficients not shown. Authors’ analysis of data from the Web-based Injury Statistics Query and Reporting System (WISQARS) Fatal Injury system, American Community Survey from IPUMS USA, Current Population Survey from IPUMS CPS, Federal Bureau of Investigation (FBI) National Instant Criminal Background Check System, U.S. Census Bureau, Kaiser Family Foundation, and the Urban Institute State and Local Finance initiative, 2002e2017. FBI ¼ Federal Bureau of Investigation. þp < .10; *p < .05; **p < .01. E.V. Goldstein et al. / Journal of Adolescent Health 70 (2022)
- 20. 83e90 87 facilitate the interpretation of our findings, we generated regression-adjusted annual probabilities of suicide for each study year, while keeping other covariates at their observed values (i.e., estimating average marginal effects). We established an a priori two-sided statistical significance level of .05. Analyses were conducted using Stata version 15.1 (College Station, TX). Insti- tutional Review Board approval was not necessary for this state- level study. Results On average, the total suicide rate among individuals aged 10e 24 in the states included in this analysis increased 47.1% from 2002 to 2017 (Table 1). The average firearm and nonfirearm suicide rates grew by 31.3% and 67.6%, respectively, over the same time period. Mental health treatment capacity, as measured by our mental health workforce variable, grew by 28.6% on a per capita basis. Table 2 shows that the total suicide rate from 2002 to 2017 grew more among adolescents aged 10e19 (69.8% in- crease) than young adults aged 20e24 (38.2% increase). From 2002 to 2017, the firearm and nonfirearm suicide rates increased by 56.1% and 81.8%, respectively, among 10- to 19-year olds and by 26.2% and 52.5%, respectively, among 20- to 24-year olds. In 2002, 9.9% of all deaths among individuals aged 10e19 were suicides. By 2017, approximately 21.3% of all deaths among per- sons aged 10e19 and 17.8% of all deaths among persons aged 20e 24 were suicides.
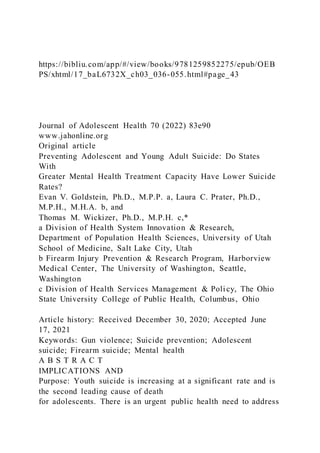
- 21. Table 3 demonstrates the between-state variation in total suicide rates over the study period, listing states with the highest and lowest total suicide rates at the beginning and end of our study. Among the states included in our analysis, Alaska, Wyoming, Montana, and South Dakota experienced the highest adolescent and young adult suicide rates, on average, from 2002 to 2017, and the rates increased in all four states from 2002 to 0.0000% 0.0020% 0.0040% 0.0060% 0.0080% 0.0100% 0.0120% 0.0140% 0.0160% 2002 2007 2012 2017 P ro b
- 22. a b il it y o f su ic id e Any suicide Firearm suicide Non-firearm suicide Figure 1. Adjusted probability of suicide, by method of suicide: 2002e2017. This figure shows the regression-adjusted probability of any suicide, firearm suicide, and nonfirearm suicide for the years 2002, 2007, 2012, and 2017. These probabilities were calculated for the entire estimation sample for each year, keeping all other covariates at their observed values (i.e., using average marginal effects). E.V. Goldstein et al. / Journal of Adolescent Health 70 (2022) 83e9088 2017. In contrast, New Jersey, New York, Massachusetts, Califor- nia, and Connecticut were consistently ranked among the states experiencing the lowest suicide rates from 2002 to 2017, although the suicide rates also increased in these states from 2002 to 2017. Bivariate analyses comparing the states with the lowest and highest suicide rates in 2017 also showed that the 10
- 23. states with the highest suicide rates likely had significantly greater firearm availability, as measured by the annual federal firearm background checks per capita. In 2017, the states with the highest suicide rates had an average of .096 federal firearm background checks per capita, compared to an average of .047 federal firearm background checks per capita in the states with the lowest suicide rates (p < .001). Table 4 shows the results of our multivariable analysis. We found an inverse relationship between the state-level mental health workforce capacity and the total suicide rate (b ¼ �.073, p ¼ .106). Although the finding was not statistically significant at the .05 significance level, the result implies that, on average, a 10% relative increase in the mental health workforce capacity in a state would be independently associated with a .923% relative reduction in the total suicide rate for persons aged 10e24 (p ¼ .106). We found a statistically significant, inverse relationship between the mental health workforce capacity and the nonfirearm suicide rate (b¼ �.052, p ¼ .015). This result implies that, on average, a 10% relative increase in the mental health workforce capacity in a state would be independently associated with a 1.35% relative reduction in the nonfirearm suicide rate for persons aged 10e24 (p ¼ .015). There was no statistically significant relationship between state-level mental health workforce capacity and the firearm suicide rate. Figure 1 shows the adjusted probability of suicide in a given year for persons aged 10e24 over the study period, as observed in our estimation sample. The adjusted probability of a person aged 10e24 dying by any method of suicide in a year increased from .0071% in 2002% to .0143% in 2017da 101.4% relative increase. Although the adjusted probability of firearm suicide increased only modestly over time, the adjusted probability of a persons aged 10e24 dying by nonfirearm
- 24. suicide in a year increased considerably from .0027% in 2002 to .0074% in 2017. There was a negative relationship between the percentage of a state’s population reporting divorced marital status and the nonfirearm suicide rate (Table 4; p ¼ .018). The percentage of a state’s adult population with a high school diploma was also inversely related with the total (p ¼ .005) and nonfirearm suicide rates (p < .001). Discussion Our findings suggest that greater mental health treatment capacity at the state level has a statistically significant protective effect of modest magnitude against nonfirearm suicide among adolescents and young adults aged 10e24, though no protective effect against firearm suicide. Our findings have relevance for policy considerations and for the development of interventions aimed at reducing youth suicide incidence. Substance abuse, interpersonal trauma, and mental illness are strongly linked to suicide attempts among younger persons [13,20,33,34]. The high case-fatality rate of firearm suicide [35] may dampen the ability of mental health practitioners to diag- nosis a mental illness or successfully intervene when necessary, yet only 7% of those who make a nonfatal suicide attempt go on to die from a future attempt [36]. For younger persons who will attemptdor have attempteddsuicide using less lethal means, risk factors for suicide may be more sensitive to greater mental illness detection efforts, and improving access to mental health treatment when needed may help prevent nonfirearm suicide attempts. Previous studies have shown promise that adequate outpa-
- 25. tient care, primary care-based interventions such as improved screening for suicide risk factors and access to cognitive behav- ioral therapy, and access to mental healthcare after presenting in an emergency department following a suicide attempt may reduce youth suicide [21,22,34,37,38]. Lethal means assessment/ restriction has also shown promise among youth with programs such as SafetyCheck [39]. As index suicide attempts (IA) have been shown to be more lethal for youth and young adults across E.V. Goldstein et al. / Journal of Adolescent Health 70 (2022) 83e90 89 all methods [3,40], prevention efforts should start prior to an IA and consider an approach that addresses both identifying serious suicidal ideation and restricting access to lethal means. Our findings may therefore support state-level efforts to improve mental health treatment capacity and promote mental health awareness. For example, states can enhance school -based mental health services capacity, which has been shown to help reduce depressive episodes and suicide risk among adolescents [41]. Schools often access funds for school-based mental health and substance abuse services through state sources, including Medicaid benefits (e.g., Early and Periodic Screening, Diagnostic and Treatment) and Medicaid waiver programs; through the state-level allocation of funds from the Every Student Succeeds Act (2015); and through state applications to the federal School - Based Mental Health Services Grant Program. States can also raise awareness about youth mental health issues by promoting mental health literacy programs like Mental Health First Aid (MHFA), which provides training on
- 26. common mental health conditions and how to refer youth for care. Since 2015, 20 states have prioritized MHFA by enacting policies to fund training, require certification for public sector employees, and establish state-wide mental health training requirements. California and Pennsylvania led the U.S. in funding MHFA trainings in 2014, and Texas allocated $5 million to train youth educators in MHFA [42]. Prior evaluations have shown that the MHFA program may help reduce unmet need for behavioral healthcare in rural areas [43]. The Youth MHFA program has also helped participants (e.g., neighbors and teachers) become more aware of mental health resources, accepting of young persons with mental health conditions, and willing to help in times of need [44]. States can also fund mental health awareness campaigns using social media, such as California’s Each Mind Matters Campaign, which have improved positive beliefs about the possibility of recovery from mental illness [45]. Our findings do not suggest that greater mental health treatment capacity will systematically reduce firearm suicide among adolescents and young adults. The risk of firearm suicide may be less about diagnosing a mental illness and more about the potential impulsivity of those who attempt suicide with firearms [46,47] and the lethality of firearm suicide [48], which together often prevent intervention from health professionals. Prior research suggests that the adoption of stricter firearm safety and control policies will likely yield greater protective effects against firearm suicide [27]. Measures often discussed by policymakers include mandatory waiting periods before firearm issue and child access prevention laws, which are shown to reduce youth firearm suicide [49,50]. However, policy interven- tion to improve firearm control is often overwhelmed by pre- vailing political forces, even though large majorities of Americansdincluding both firearm owners and nonfirearm
- 27. ownersdsupport a range of regulatory measures to strengthen firearm safety laws [51]. As described in Table 3, states with the highest suicide rates had significantly greater federal firearm background checks per capita, a proxy for gun ownership. Yet evidence-based policies shown to reduce firearm suicide appear to be absent in states with the highest suicide rates [17]. Our findings also suggest that higher rates of high school completion were significantly associated with lower suicide rates, consistent with other studies [52]. These findings may support the idea that investments in education are important for preventing suicide among adolescents and young adults. At the individual level, suicide risk tends to increase with poor school performance and dropout [53,54], though the link between educational attainment and suicide is less certain. However, when considering education as a measure of aggregate human capital in the context of other related socioeconomic factors, education may have a protective effect [55]. Improving funding for K-12 public education in states with high suicide rates, encouraging other investments in human capital development, and providing opportunities for family counseling as part of schooling [56] should be explored as population-level suicide prevention strategies. Limitations This study has several limitations. First, we used a non- randomized, retrospective study design, which imposes limits on causal inference. Second, because we conducted a state-level analysis, readers should refrain from making inferences about individual behavior. Third, without more granular data (e.g., in- dividual or county level), we could not perform a multivariable analysis within each state longitudinally. Fourth, as described earlier, CDC data restrictions prevented us from constructing our
- 28. dependent variables for all state-years. For this reason, the generalizability of our results is potentially limited to the states included in our analytic sample. Fifth, for the same reasons of insufficient data and data restrictions, we could not conduct subgroup analyses by sex or age (e.g., only persons <18 years). It would be important to explore how sex may have moderated our findings in future studies using different data. Sixth, due to Bu- reau of Labor Statistics data limitations, we could not identify and include other types of providersdsuch as mental health nurse practitioners or adolescent behavioral health physiciansdin our measure of mental health treatment capacity. Nonmental health practitioners may provide mental health screening or other services to adolescents and young adults. This limitation also prevented us from identifying and constructing a measure of only school-based mental healthcare providers. Finally, we could not directly control for firearm availability, an important pre- dictor of youth suicide. Consistent with other studies we included a proxy measure of the annual number of federal firearm background checks performed in each state [32]. How - ever, federal background checks do not capture private firearm purchases, hence this variable is an incomplete proxy measure for firearm availability. Conclusions Increasing the mental health workforce and the availability of mental health services at the state level appears to be important for nonfirearm suicide prevention. In contrast, mental health treatment capacity appears to have little effect on the more lethal method of firearm suicide. Mental health dis- orders may go undiagnosed among youth who die by all methods of suicide. However, given that suicide can be an impulsive act [46] and suicide attempts using a firearm are nearly always fatal, preventing firearm suicide directly may be
- 29. best addressed through the enactment of evidence-based firearm safety and storage regulations by state-level policy- makers. Population-level investments in human capital devel- opment may also promote future well-being and protect young persons from suicide. E.V. Goldstein et al. / Journal of Adolescent Health 70 (2022) 83e9090 Funding Sources Dr. Prater receives research funding support from the State of Washington. References [1] Centers for Disease Control and Prevention. Suicide & self- inflicted injury. 2017. Available at: https://www.cdc.gov/nchs/fastats/suicide.htm. Accessed December 1, 2019. [2] Heron M. Deaths: Leading causes for 2016. Natl Vital Stat Rep 2018;67:1e 77. [3] Ruch DA, Sheftall AH, Schlagbaum P, et al. Trends in suicide among youth aged 10 to 19 years in the United States, 1975 to 2016. JAMA Netw Open 2019;2:e193886. [4] Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system (WISQARS) [Internet]. Available
- 30. at: https:// www.cdc.gov/injury/wisqars/index.html. Accessed December 15, 2020. [5] Choi NG, DiNitto DM, Marti CN. Youth firearm suicide: Precipitating/risk factors and gun access. Child Youth Serv Rev 2017;83:9e16. [6] Centers for Disease Control and Preventation. 10 leading causes of death by age group, United States e 2017. 2017. Available at: https://www.cdc.gov/ nchs/fastats/leading-causes-of-death.htm. Accessed December 1, 2019. [7] Doran CM, Kinchin I. Economic and epidemiological impact of youth sui- cide in countries with the highest human development index. PLoS One 2020;15:e0232940. [8] Knopov A, Sherman RJ, Raifman JR, et al. Household gun ownership and youth suicide rates at the state level, 2005e2015. Am J Prev Med 2019;56:335e42. [9] Minoiu C, Andrés AR. The effect of public spending on suicide: Evidence from U.S. state data. J Socio Econ 2008;37:237e61. [10] Cash SJ, Bridge JA. Epidemiology of youth suicide and suicidal behavior. Curr Opin Pediatr 2009;21:613e9. [11] Lindsey MA, Sheftall AH, Xiao Y, Joe S. Trends of suicidal behaviors among
- 31. high school students in the United States: 1991-2017. Pediatrics 2019;144: e20191187. [12] Russell ST, Fish JN. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annu Rev Clin Psychol 2016;12:465e87. [13] Nanayakkara S, Misch D, Chang L, Henry D. Depression and exposure to suicide predict suicide attempt. Depress Anxiety 2013;30:991e6. [14] Stone DM, Simon TR, Fowler KA, et al. Trends in state suicide rates 1999- 2016. Morb Mortal Wkly Rep 2018;67:617e24. [15] Fleegler EW, Lee LK, Monuteaux MC, et al. Firearm legislation and firearm- related fatalities in the United States. JAMA Intern Med 2013;173:732e40. [16] Santaella-Tenorio J, Cerdá M, Villaveces A, Galea S. What do we know about the association between firearm legislation and firearm- related in- juries? Epidemiol Rev 2016;38:140e57. [17] Smart R, Morral A, Smucker S, et al. The science of gun policy. 2nd ed. Santa Monica: RAND Corporation; 2020. [18] Goldstein EV, Prater LC, Bose-Brill S, Wickizer TM. The firearm suicide crisis: Physicians can make a difference. Ann Fam Med 2020;18:265e8.
- 32. [19] Robinson J, Bailey E, Witt K, et al. What works in youth suicide prevention? A systematic review and meta-analysis. EClinicalMedicine 2018;4-5:52e91. [20] Joshi K, Billick SB. Biopsychosocial causes of suicide and suicide prevention outcome studies in juvenile detention facilities: A review. Psychiatr Q 2017;88:141e53. [21] Asarnow JR, Baraff LJ, Berk M, et al. An emergency department intervention for linking pediatric suicidal patients to follow -up mental health treat- ment. Psychiatr Serv 2011;62:1303e9. [22] Campo JV. Youth suicide prevention: Does access to care matter? Curr Opin Pediatr 2009;21:628e34. [23] Boggs JM, Beck A, Ritzwoller DP, et al. A quasi- experimental analysis of lethal means assessment and risk for subsequent suicide attempts and deaths. J Gen Intern Med 2020;35:1709e14. [24] Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: A sys- tematic review. J Am Med Assoc 2005;294:2064e74. [25] Yip PSF, Caine E, Yousuf S, et al. Means restriction for suicide prevention. Lancet 2012;379:2393e9. [26] Daigle MS. Suicide prevention through means restriction:
- 33. Assessing the risk of substitution. A critical review and synthesis. Accid Anal Prev 2005; 37:625e32. [27] Goldstein EV, Prater LC, Wickizer TM. Behavioral health care and firearm suicide: Do states with greater treatment capacity have lower suicide rates? Health Aff (Millwood) 2019;38:1711e8. [28] Johnson KF, Brookover DL. Counselors’ role in decreasing suicide in mental health professional shortage areas in the United States. J Ment Health Couns 2020;42:170e86. [29] Bureau of Labor Statistics. Occupational Employment Statistics [Internet]. Available at: https://www.bls.gov/oes/. Accessed December 15, 2020. [30] Borgschulte M, Vogler J. Did the ACA Medicaid expansion save lives? J Health Econ 2020;72:102333. [31] Anglemyer A, Horvath T, Rutherford G. The accessibility of firearms and risk for suicide and homicide victimization among household members: A systematic review and meta-analysis. Ann Intern Med 2014;160: 101e10. [32] Lang M. Firearm background checks and suicide. Econ J 2013;123:1085e 99.
- 34. [33] Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents. JAMA Psychiatry 2013;70: 300. [34] Cavanagh JTO, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: A systematic review. Psychol Med 2003;33:395e405. [35] Spicer RS, Miller TR. Suicide acts in 8 states: Incidence and case fatality rates by demographics and method. Am J Public Health 2000;90:1885e 91. [36] Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Br J Psychiatry 2002;181:193e9. [37] Bridge JA, Horowitz LM, Fontanella CA, et al. Prioritizing research to reduce youth suicide and suicidal behavior. Am J Prev Med 2014;47(3 Suppl 2): S229e34. [38] Fontanella CA, Warner LA, Steelesmith DL, et al. Association of timely outpatient mental health services for youths after psychiatric hospi- talization with risk of death by suicide. JAMA Netw Open 2020;3: e2012887. [39] Wolk CB, Jager-Hyman S, Marcus SC, et al. Developing
- 35. implementation strategies for firearm safety promotion in paediatric primary care for suicide prevention in two large US health systems: A study protocol for a mixed-methods implementation study. BMJ Open 2017;7: e014407. [40] McKean AJS, Pabbati CP, Geske JR, Bostwick JM. Rethinking lethality in youth suicide attempts: First suicide attempt outcomes in youth ages 10 to 24. J Am Acad Child Adolesc Psychiatry 2018;57:786e91. [41] Paschall MJ, Bersamin M. School-based health centers, depression, and suicide risk among adolescents. Am J Prev Med 2018;54:44e50. [42] National Council for Behavioral Health. Mental health first aid policy handbook. 2019. Available at: https://www.thenationalcouncil.org/wp- content/uploads/2019/03/031219_NCBH_MHFAPolicyHandboo k_v6.pdf? daf¼375ateTbd56. Accessed December 15, 2020. [43] Talbot JA, Ziller EC, Szlosek DA. Mental health first aid in rural com- munities: Appropriateness and outcomes. J Rural Health 2017;33:82e 91. [44] Noltemeyer A, Huang H, Meehan C, et al. Youth mental health first aid: Initial outcomes of a statewide rollout in Ohio. J Appl Sch Psychol 2020;36:
- 36. 1e19. [45] Collins RL, Wong EC, Breslau J, et al. Social marketing of mental health treatment: California’s mental illness stigma reduction campaign. Am J Public Health 2019;109:S228e35. [46] Simon TR, Swann AC, Powell KE, et al. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav 2002;32:49e59. [47] Peterson LG, Peterson M, O’Shanick GJ, Swann A. Self- inflicted gunshot wounds: Lethality of method versus intent. Am J Psychiatry 1985;142: 228e31. [48] Conner A, Azrael D, Miller M. Suicide case-fatality rates in the United States, 2007 to 2014 a nationwide population-based study. Ann Intern Med 2019;171:885e95. [49] Webster DW, Vernick JS, Zeoli AM, Manganello JA. Association between youth-focused firearm laws and youth suicides. J Am Med Assoc 2004;292: 594e601. [50] Gius M. The impact of minimum age and child access prevention laws on firearm-related youth suicides and unintentional deaths. Soc Sci J 2015;52: 168e75.
- 37. [51] Barry CL, Stone EM, Crifasi CK, et al. Trends in public opinion on us gun laws: Majorities of gun owners and nonegun owners support a range of measures. Health Aff (Millwood) 2019;38:1727e34. [52] Fontanella CA, Saman DM, Campo JV, et al. Mapping suicide mortality in Ohio: A spatial epidemiological analysis of suicide clusters and area level correlates. Prev Med 2018;106:177e84. [53] Kosidou K, Dalman C, Fredlund P, et al. School performance and the risk of suicide attempts in young adults: A longitudinal population- based study. Psychol Med 2014;44:1235e43. [54] Daniel SS, Walsh AK, Goldston DB, et al. Suicidality, school dropout, and reading problems among adolescents. J Learn Disabil 2006;39:507e14. [55] Kroll-Desrosiers AR, Crawford SL, Moore Simas TA, et al. Improving preg- nancy outcomes through maternity care coordination: A systematic re- view. Womens Health Issues 2016;26:87e99. [56] Stormshak EA, Connell AM, Véronneau MH, et al. An ecological approach to promoting early adolescent mental health and social adaptation: Family-centered intervention in public middle schools. Child Dev 2011;82:
- 43. http://refhub.elsevier.com/S1054-139X(21)00333-5/sref52 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref52 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref53 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref53 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref53 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref53 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref54 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref54 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref54 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref55 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref55 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref55 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref55 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref56 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref56 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref56 http://refhub.elsevier.com/S1054-139X(21)00333-5/sref56 http://refhub.elsevier.com/S1054-139X(21)00333- 5/sref56Preventing Adolescent and Young Adult Suicide: Do States With Greater Mental Health Treatment Capacity Have Lower Suicide R ...MethodsData and study designDependent variablesIndependent variablesCovariatesAnalysisResultsDiscussionLimitationsConcl usionsFunding SourcesReferences Aggression and Violent Behavior xxx (xxxx) xxx Please cite this article as: Scott Poland, Sara Ferguson, Aggression and Violent Behavior, https://doi.org/10.1016/j.avb.2021.101579 Available online 15 February 2021 1359-1789/© 2021 Elsevier Ltd. All rights reserved.
- 44. Youth suicide in the school context Scott Poland, Sara Ferguson * Nova Southeastern University, 3301 College Ave, Fort Lauderdale, FL 33314, United States of America A R T I C L E I N F O Keywords: School mental health professionals Postvention Intervention School Prevention Youth suicide A B S T R A C T Across the domains of youth risk behavior, suicidality is a significant concern for parents and professionals alike, requiring ongoing efforts to better understand and prevent rising trends. Recent examinations of suicidal be- haviors in the United States over the last decade revealed an increase in emergency and inpatient hospital set- tings. Of importance, seasonal variations were demonstrated, finding the lowest frequency of suicidality encounters in summer months, and observed peaks in the fall and spring, during the school year. Given these findings and the fact that youth spend nearly half of their time at school, consideration of youth suicide in the school environment is critical. This paper will review the trends of youth suicide within the school context, exploring factors such as at-risk youth, bullying, relevant legal issues, and the current state of crisis response in school settings. Recommendations for prevention, intervention,
- 45. and postvention will be provided. The authors propose that school professionals play a vital role in addressing youth suicide and will aim to provide guidance on effective crisis response within the school context. 1. Introduction Suicide is a leading cause of death in the United States (CDC, 2018) and a prominent concern in the mental health and medical fields given the high rates of suicidal ideation and attempts. While death by suicide is an incredibly difficult and often unfathomable tragedy, its occurrence in the youth population can bring even more confusion and intense grief for loved ones. In 2016, suicide became the second leading cause of death for ages 10–34 (CDC, 2017b). Furthermore, a 2018 review of injury mortality among youth during 1999–2016 identified suicide as the second leading injury intent among 10–19 years (in which a 56% increase was observed between 2007 and 2016 [Curtin et al., 2016]). The Youth Risk Behavior Surveillance Survey ([YRBSS], CDC, 2017a), the Centers for Disease Control and Prevention’s (CDC) biennial survey of adolescent health risk and health protective behaviors, revealed upward trends in their survey of suicidality and related be- haviors of high school students (see Fig. 1.1). Specifically, students re-
- 46. ported an increase over the last decade in seriously considering attempting suicide and making a suicide plan. Of concern, among the few states that queried middle school students, trends were observed at an even higher rate. Given the high rates of suicidal behavior among young people, ample research has been dedicated to this topic, resulting in pertinent knowl- edge necessary to better understand the matter. A variety of risk factors have been consistently identified across the literature, many of which inform prevention and intervention practices for clinicians. There is, however, an area in which additional attention should be awarded: the school context. Young people spend a significant portion of their time in school settings in which they are actively engaged with their peers and subject to the potential stressors of academic achievement and future success. In light of this, consideration of youth suicide in the school context is of utmost importance. Evidence reports that school influences the behavior and health of young people (Evans & Hurrell, 2016). This is additionally supported by recent research that has demonstrated significant seasonal variations in youth suicide patterns (Plemmons’ et al., 2018),
- 47. suggesting that involvement in school should be further examined as a critical factor in youth suicidality. This paper aims to contribute to this suggestion, in which we will review relevant literature related to youth suicide in the school context, including associated risk factors, existing prevention, intervention, and postvention programming, and related legal implications. Recommen- dations for best practices will be offered, specific to both school and mental health professionals. The authors propose that school pro- fessionals play an essential role in addressing youth suicide and will aim to offer guidance on effective crisis response within the school context. * Corresponding author. E-mail addresses: [email protected] (S. Poland), [email protected] (S. Ferguson). Contents lists available at ScienceDirect Aggression and Violent Behavior journal homepage: www.elsevier.com/locate/aggviobeh https://doi.org/10.1016/j.avb.2021.101579 Received 1 December 2019; Received in revised form 19 July 2020; Accepted 5 February 2021
- 48. mailto:[email protected] mailto:[email protected] www.sciencedirect.com/science/journal/13591789 https://www.elsevier.com/locate/aggviobeh https://doi.org/10.1016/j.avb.2021.101579 https://doi.org/10.1016/j.avb.2021.101579 https://doi.org/10.1016/j.avb.2021.101579 Aggression and Violent Behavior xxx (xxxx) xxx 2 2. Youth suicide & seasonal variations As discussed, it has been well established that there are rising trends in youth suicidal behavior. Recent research in related domains supports these findings, such as observed increases in hospitalizations (Burstein et al., 2019), attempts by females (CDC, 2017b), use of suffocation as preferred method (Curtin et al., 2018), and serious considerations of suicide, along with the creation of a plan (CDC, 2017a). Plemmons’ et al. (2018) recent large-scale study examining youth suicidal encounters in pediatric emergency and inpatient hospital settings further supported the observed increases, demonstrating consistent upward trends of sui- cidal ideation and attempts across age groups and genders. Of interest, a pattern of seasonal variation was observed, in which a higher
- 49. percentage of cases was found during the fall and spring and conversely, a lower number of cases during the summer months. Such findings are of significance, as they shed light on a critical factor of youth suicide that has not been historically explored. Research related to this matter is limited and recent (see Hansen & Lang, 2011; Lueck et al., 2015), suggesting a gap in the conceptualization of youth suicide. Plemmons’ et al. (2018) findings of seasonal patterns lead one to consider the variables associated with the months in which increased and decreased rates were observed. Most glaringly, is the consideration of youth participation in school during the fall and winter months and the subsequent break during the summer months. Lueck et al. (2015) set out to investigate this aspect of youth suicide, in which they analyzed the relationship between weeks in school vs. weeks out of school (i.e., vacation) with concern for danger to self or others. Of note, the researcher’s review of 3223 subjects (mean age, 13.8 years) who presented to a local pediatric emergency unit included youth with both suicidal and homicidal ideation, creating challenges in isolating the results solely to the examination of suicidal behavior.
- 50. However, their findings of higher rates of such ideation during weeks in which the subjects were in school vs. the reduced rates observe d during vacation weeks certainly contributes to the growing understanding that the school context has a significant impact on risk behaviors such as suicidality. Similarly, Hansen and Lang (2011) hypothesized that youth in school served as a crucial factor in the seasonal patterns of youth suicide. Their investigation established a distinct alignment of youth suicide with the school calendar, including a significant decrease during the summer breaks; one that commenced upon entering adulthood. Further, unlike many youth suicide studies, the researchers examined the data for each gender separately, finding that the suicide rate, on average, was 95% higher for boys in school months when compared to girls (33%). Addi- tionally, the authors proposed theories regarding school specific factors that likely influenced these trends, including negative peer interactions, along with academic stressors and the related mental health impact. These findings create a scientific foundation for youth suicide in the
- 51. school context that warrant a deeper investigation. Additionally, the authors would be remiss not to highlight the fact that youth spend nearly half of the total days of the year in school settings, thereby making it the most logical place to intervene. Access to the youth, along with potential resources within the school and community create an ideal environment for prevention and intervention. These factors create a cogent argument for continued exploration of youth suicide in the context of the school environment. 3. Risk factors in the school context In light of the reviewed findings of seasonal patterns of youth suicide rates and their association to school participation, along with the sheer amount of time spent in the school setting, consideration of the school related factors that may contribute to youth suicidal behaviors is essential. Risk factors associated with youth suicide have been broadly identified, including specific individual and psychosocial variables. Such factors include youth that have little social supports, many of whom often present with pathologies such as mood and substance use disorders, bullies and victims, individuals who identify as LGBTQ, and
- 52. youth exposed to adverse early childhood experiences such as trauma, family system disturbances, and most notably, suicide (Gould et al., 2003; Lieberman et al., 2008). Moreover, across the risk factors reviewed, of greatest significance is a prior suicide attempt. Research reveals that a prior attempt is the strongest predictor of a future death by suicide (Harris & Barraclough, 1997). Fig. 1.1. YRBSS suicide related behavioral trends. S. Poland and S. Ferguson Aggression and Violent Behavior xxx (xxxx) xxx 3 3.1. Social connectedness Specific to the context of school, a variety of risk factors are pertinent to review in detail. As mentioned, level of social support has been determined as a risk factor for youth suicide, in which a child or ado- lescent’s connectedness to his or her peers can play a significant role in his or her vulnerability to suicidal behavior (Lieberman et al., 2008). It is broadly accepted that the development of positive and close relation- ships with others can serve as a protective and preventive buffer
- 53. against suicidal ideation and behaviors. Connectedness typically results in high rates of social contact and lower rates of feelings of loneliness and isolation (CDC, 2011). While social connectedness has been established as a prominent factor in the conceptualization of suicidal behaviors (Joiner, 2005), it is important to consider this variable specifically in the context of youth suicide, given the easy access to potential social relationships (both negative and positive). Furthermore, it has been well documented that young people who are at higher risk for suicidal behaviors often face adversity such as familial disturbances and related neglect, homeless- ness, or involvement in social services (i.e., foster care), all of which negatively impact an individual’s level of connectedness. Lack of social connectedness in youth is a broad risk factor to consider and the related vulnerabilities that arise as a result are certainly contributing factors to suicidal behavior. Increased isolation, for example, can negatively impact self-esteem and potentially lead to depression, another identified risk factor of youth suicide (Lieberman et al., 2008). The milieu of school provides an ideal setting to enhance social connectedness for children and adolescents. Moreover, it gives
- 54. the op- portunity for school staff to act as warm and accepting social role models that can aid in providing a formal support system of connectedness. Recommendations for enhancing social support and connectedness as means to buffer suicide risk have been discussed across the literature, including the development of prevention programs that are founded upon this concept (e.g., Gatekeeping Training (Burnette et al., 2015; CDC, 2011)). While such programs (which will be reviewed in further detail) have been demonstrated as being an effective intervention for reducing suicide attempts in youth (see Aseltine et al., 2007; Aseltine & DeMartino, 2004), there are a variety of factors in school settings that not only create challenges in enhancing social connectedness across diverse student bodies, but also contribute to higher rates of suicidal behavior in young people. 3.2. Bullying Relatedly, engagement in bullying (whether as the bully or the victim), has been identified as a risk factor for youth suicide (Holt et al., 2015; Lieberman et al., 2008). The Suicide Prevention Resource Center’s (SPRC) (2011) Issue Brief on Suicide and Bullying revealed a strong
- 55. association between bullying and suicide, reporting that children who are bullied are at highest risk for suicide due to the commonality of risk factors. Dan Olweus, creator of the Olweus Bullying Prevention Program (1993), defines bullying as occurring “when a person is exposed repeatedly, and over time, to negative actions on the part of one or more persons, and he or she has difficulty defending himself or herself” (p. 9, Olweus, 1993). Lierberman and Cowan (2006) reported that interper- sonal problems are frequently cited by adolescents as the antecedent of suicidal behavior, in which loss of dignity and humanity is conceptu- alized as a triggering event. Moreover, Gould and Kramer (2001) pro- vided insight regarding bully behavior, suggesting that the more frequently an adolescent engages in bullying, the more likely that she or he is experiencing feelings of hopelessness and depression, has serious suicidal ideation, or has attempted suicide in the past. The 2017 School Crime Supplement (National Center for Education Statistics and Bureau of Justice, 2018) found that in the United States, approximately 20% of students ages 12–18 experienced bullying. It is important to note that bullying can occur both in and out of the school environment, especially given the rapidly evolving state of
- 56. technology and social media. Cyberbullying is a growing concern (YBRSS data es- timates that 14.9% of high school students were electronically bullied in the 12 months prior to the survey [CDC, 2017a]). It is defined as any type of bullying (i.e., mean/hurtful comments, spreading rumors, physical threats, pretending to be someone else, and mean/hurtful pic- tures) through a cell phone text, e-mail, or any social media outlet or online source (Hinduja & Patchin, 2012). Cyberbullying presents significant concerns related to its aspects of anonymity and ease of access. Moreover, it is pervasive and can occur in both the home and school setting, creating an environment of contin- uous bullying. The high frequency of cyberbullying is significant in the conceptualization of youth suicide in the school context, as students often have access to social media platforms where bullying frequently occurs during school hours. This likely contributes to the finding that reports of bullying continue to be highest within the school setting (U.S. Department of Health and Human Services, 2019). This is further sup- ported by the YRBSS data (CDC, 2017a), which revealed that nationally, 19% of students in grades 9–12 report being bullied on school
- 57. property in the 12 months preceding the survey. While bullying has received increased public attention over time and actions have been taken to target the issue, it clearly persists in the school settings. More so, the findings certainly demonstrate the tragic and very permanent implica- tions that bullying can lead to in the context of youth suicide. 3.3. LGBTQ population Given the significant findings related to bullying and suicidal behavior in children and adolescents, it is important to consider special populations that may be at higher risk of being bullied, as this may serve as an indirect route to suicidal behaviors. Children and adolescents who are questioning their sexual orientation or gender identity have been found to have high rates of negative outcomes in a number of areas including harassment, victimization, and bullying, along with violence, drug abuse, sexually transmitted diseases, and mental health problems, such as depression (Birkett et al., 2015; CDC, 2017a). Strikingly, this population has been found to be more likely to consider and attempt suicide (Almeida et al., 2009; Hatzenbuehler, 2011; Kosciw, Greytak, Bartkiewicz, Boesen, & Palmer, 2012; Lieberman et al., 2014). In fact,
- 58. YRBSS (CDC, 2017a) data revealed significantly higher percentages of attempted suicides of lesbian, gay, or bisexual students (23.0%) and students not sure of their sexual identity (14.3%) when compared to their heterosexual students (5.4%). Family acceptance appears to be a major factor in the experience of suicidal ideation, as those who experience a high level of acceptance are found to have lower rates (18.5%) when compared to those with low acceptance from their families (38.3% (Ryan, Russell, Huebner, Diaz, & Sanchez, 2010)). Furthermore, acceptance in other areas of a LGBTQ identifying youth’s life, such as the school and broader community, has been suggested as a significant protective factor to the many risks they face (Birkett et al., 2015), thereby promoting self-acceptance and resil- ience (Dahl & Galliher, 2012). Consideration of the LGBTQ population in the school context is critical, as it can serve as an environment of safety, acceptance, and connectedness. There are a number of recommendations for school and mental health professionals to best support LGBTQ youth; however, despite the availability of specific recommendations (e.g., creation of safe-spaces and student-led advocacy groups), LGBTQ youth
- 59. continue to widely report feeling unsafe at school (10%, CDC, 2017a), presenting serious ongoing concerns for this population. These findings, paired with the previously mentioned associated negative outcomes, including high rates of suicidal behavior, certainly justify the need for special attention and consideration in the school context. S. Poland and S. Ferguson Aggression and Violent Behavior xxx (xxxx) xxx 4 3.4. Ethnicity and culture Consideration of high-risk populations must include the examination of suicide rates and related risk factors of young people across diverse ethnic and cultural backgrounds. While the prevalence rates of SI and SA vary among differing identifications of race and ethnicity, there are specific populations who have been identified as high risk for suicidal behavior (Lieberman et al., 2008). In 2017, The CDC (2017b) reported that the age-adjusted rate of suicide among American Indians/Alaska Natives was 22.15 per 100,000 and among non-Hispanic whites
- 60. it was 17.83. In contrast, lower and more similar rates were found among Asian/Pacific Islanders (6.75%), Blacks (6.85%), and Hispanics (6.89%). YRBSS’ data reveals that Black or African American students reported the highest rate of suicide attempts (9.8%), followed by white students at 6.1% (CDC, 2017a). Of note, YRBSS did not include Amer- ican Indians/Alaska Natives as an option of ethnic identification; how- ever, the CDC (2017b) reported that suicide rates peak during adolescence and young adulthood among this population and then decline. This pattern greatly differs from the general United States population, where rates of suicide peak in mid-life. The disproportionate level of risk for suicide in youth who identify as American Indian and Alaska Native has been well researched, in which a variety of contributing factors have been identified, e.g., high rates of substance use, exposure to adverse early childhood experiences, limited access to resources due to rural settings, and increased potential for contagion effects of suicide (Leavitt et al., 2018). In light of these complex vulnerabilities, researchers often recommend school involve- ment in prevention and intervention to target the varied risk factors present, especially as they relate to suicidal behavior. School
- 61. program- ming can typically reach larger populations, a dire need in rural areas in which many of these young people reside (Leavitt et al., 2018; Lieber- man et al., 2008). Specific recommendations within the school context are offered across the relevant literature, which will be integrated into clinical recommendations in later reading. 4. Legal implications of suicide in the school context Suicide in the school context is a complex issue that can create sig- nificant legal implications regarding the liability of the school district and staff, especially administrators, support staff, and school psycholo- gists. In the United States, there have been numerous legal battles in which schools are sued in the aftermath of a death by suicide of a young person. While this presents major concerns for school personnel, very rarely do the parents of suicidal students succeed in court proceedings. With the exception of the school’s failure to notify parents when there is reason to suspect a student’s risk for suicide, courts have been reluctant to find schools culpable (Stone, 2017). Friedlander (2013) reported that parents as the plaintiffs face slim chances when they file a lawsuit against the school or its
- 62. officials after the suicide of their child. Many factors contribute to this, including the lack of resources, i.e., financial means, the lengthy trial periods, and limited evidentiary documentation. Cases that cite bullying as a critical factor in the youth’s suicide, for example, often lack the necessary documentation of the parents’ concerns that are often reportedly shared with school officials prior to their child’s death by suicide. Moreover, Poland (Erbacher, Singer, & Poland, in press) reported that only a small number of these cases make it to a jury trial. More often, the school districts’ insurance companies decide to settle the cases outside of court, as it can be a less costly and public matter, when compared to the potential of a lengthy defense of the district in litiga- tion. Moreover, public legal battles can generate a negative stigma around the school and its district. However, MacIver (2011) suggested that the number of court cases against schools may continue to rise in the future, as courts are becoming more receptive to finding the defendants liable for causing another person’s suicide. Further, suicide experts are reported as having increased success in either proving or disproving a
- 63. specific cause of suicide. In review of cases that have gone to trial, rulings are varied, muddying the legal guidelines for school suicide prevention and related liability. Dr. Scott Poland, one of the present authors and a leading expert in youth suicide, discussed the complexity of these cases in his chapter on Legal Issues for Schools (Erbacher et al., in press). In sum, courts must primarily consider whether a student’s death by suicide was a direct result of an inadequate response from the school personnel; however, given the varied psychosocial risk factors associated with youth suicide (e.g., mental health, and adverse childhood experiences), it is highly difficult to prove that a school’s breach of duty is the sole causal factor of the suicide, thereby making the personnel liable. 4.1. School liability: relevant legal cases What then is the school’s liability in cases of student suicides? His- torically, courts ruled that schools did not have a legal obligation to prevent suicide (Stone & Zirkel, 2012). A 1991 appellate case, Eisel v. Board of Education of Montgomery County, set new precedent on this matter. The father of 13-year-old Nicole Eisel sued the school district
- 64. and two of its school counselors after they failed to report their learning of an apparent murder-suicide pact with another peer. The father argued that the special relationship the personnel maintained with his daughter placed a duty upon them to share her reported suicidal ideation with her parents. The Maryland Supreme Court held that the state’s Suicide Prevention School Programs Act, the school’s own suicide prevention policy, and the relationship between school, counselor, and youth gave rise to a duty on the counselors’ part to use “reasonable means to attempt to prevent a suicide when they are on notice of a child or adolescent student’s suicidal intent” (Eisel v. Board of Education of Montgomery County, 1991), including, at a minimum, a report to the student’s parents. The Court listed “foreseeability of harm,” i.e., a reasonable person would have been able to recognize that a student was in an acute emotional state of distress and in danger of suicide, as the prominent factor in determining whether school employees had a duty to warn student’s parents (Eisel v. Board of Education of Montgomery County, 1991; Friedlander, 2013). While this was significant regarding the role of school professionals,
- 65. it did not create an absolute precedent of liability for schools. In fact, the very same school district cited in the 1991 case was sued just a few years later after another student’s suicide in Scott v. Montgomery County Board of Education (1997), in which the court did not adhere to the precedent of liability for school mental health professionals (SMHPs). A federal appellate court upheld the dismissal of the lawsuit initiated by the mother of a middle school student who had hanged himself. The school psychologist met with the student approximately two months prior to the student’s suicide and did not assess him as posing an im- mediate danger of self-harm; furthermore, did not report the informa- tion to the student’s parents. The court dismissed the mother’s claims of negligence as educational malpractice, concluding that the alleged causal linkage to the school psychologist was not sufficient (Scott vs. Montgomery County Board of Education, 1997; Stone & Zirkel, 2012). Court cases post Eisel (1991) in many states have continued to consider school districts or personnel liability for student suicides. Friedlander (2013) relayed that among these cases, claims of negligence that are grounded in “statutory, regulatory, or district policy for suicidal
- 66. threats and suicide prevention” (Friedlander, 2013) are most promising to plaintiffs. Negligence is a breach of duty owed to an individual involving injury or damage (suicide) that finds a causal connection be- tween a lack of or absence of duty to care for the student and his/her subsequent suicide (Stone, 2017). In Wyke v. Polk County School Board (1997), for example, the Eleventh Circuit Court of Appeals concluded that the school board was liable for the death of 13-year-old Shawn Wyke. Wyke hanged himself at his home two days after two failed attempts were completed at school. His mother, Carol Wyke utilized the “failure to train theory” arguing that S. Poland and S. Ferguson Aggression and Violent Behavior xxx (xxxx) xxx 5 the lack of suicide prevention/intervention training for the school personnel demonstrated a direct indifference to their duty to care and protect (Erbacher et al., in press). While the school board argued that suicide is an intervening force, the jury found that the school was
- 67. “somewhat aware” of the attempts on campus and made no efforts to intervene, i.e., hold the child in protective custody, recommend, pro- vide, or obtain protective counseling for the student, or report the in- cidents to his parents. Further, the Court concluded that given the known attempts, the school personnel had strong reason to anticipate the suicide which was thus, foreseeable (Erbacher et al., in press; Friedlander, 2013; Wyke v. Polk County School Board, 1997). Negligence and foreseeability are not the only factors that have been identified in determining school liability in student suicides. Sovereign immunity, for example, has been used in school related suicide cases. Government entities are granted immunity if their conduct does not clearly violate constitutional rights of which a reasonable person would have known. There is a constitutional right of a duty to protect students and state laws require compulsory attendance for students; however, legal cases have failed to find that a child’s required attendance at school creates a relationship that would mandate a school’s duty to protect students. Immunity is based on state law; if the state deems schools an arm of the state government, then schools within that state are granted
- 68. sovereign immunity (Erbacher et al., in press). Additionally, a school can be found in violation of legal re- sponsibility based on the constitutional rights of the victims, i.e., state created danger. The school may be liable if it does not enact or follow through with specific policies and procedures, thereby causing danger to the student who died by suicide (Erbacher et al., in press; Sanford v. Stiles, 2006). Lastly, many school attorneys use the “intervening force” argument to defend the school and its personnel, stating that suicide is a superseding and intervening force that breaks the direct connection between the defendants’ actions, i.e., failure to notify parents, and the suicide. In sum, the intervening force is the real reason for the suicide that resulted and the longer the timeframe between the possible negli- gence of the school and the suicide of a student, the more logical the intervening force argument (Erbacher et al., in press). 4.2. Legislation The major legal implications of youth suicide in the school context certainly justify the need for state laws and mandates targeted at suicide prevention and intervention in the school setting. In the past, district- wide suicide prevention efforts oftentimes only occurred after
- 69. the occurrence of a tragic student death. Currently, a majority of states require some type of suicide prevention training for their school personnel. However, the programming, efforts, and quality vary state by state (Kreuze et al., 2017; Singer et al., 2018). The American Foundation of Prevention for Suicide (AFPS, 2019) reviewed current state laws in the United States, finding varied policies and procedures related to prevention programming. To date, 11 states require mandated annual training; moreover, 20 states (40%) also require mandated training, but without the yearly contingency. Many states without mandated training are making efforts to encourage training throughout school districts; further, many require the provision of suicide prevention and intervention policies and procedures (AFPS, 2019). The Garrett Lee Smith Memorial Act (2004) was the first bill signed into law pertaining to suicide prevention among young people in the United States. It affirmed suicide as national public health problem and intended to provide funding to states, tribes, campuses, and behavioral mental health services for grants that support prevention and inter-
- 70. vention efforts. In 2007, a hallmark piece of legislation, the Jason Flatt Act, was passed in the state of Tennessee, requiring all educators in the state to complete 2 h of youth suicide awareness and prevention training each year in order to be able to be licensed to teach. The Tennessee legislation now serves as the model to introduce the Jason Flatt Act (2007) in other states. It’s founders, Jason Foundation Inc. (a non-profit agency dedicated to bringing suicide prevention awareness and educa- tion to schools), report that to date, 20 states have adopted the act (although each state’s requirements vary [AFPS, 2019]) and have been supported by the state’s Department of Education and the state’s Teacher’s Association, highlighting the value observed in such preven- tative training (Erbacher et al., in press; JasonFoundation, 2019). AFPS (2019) is dedicating major advocacy efforts toward the adop- tion of the Jason Flatt Act (2007) in states that are still lacking in legal mandates for suicide prevention. For these states, AFPS has created a model legislation that can be used as a guide for individuals who would like to lobby for the passage of this type of training. Lobbyists and ad- vocates report frustrations in their continued efforts,
- 71. particularly regarding the language used in the adoption of policies and procedures. One critique, for example, is the state’s use of the word “recommended” instead of “required” in suicide training for schools (Lieberman & Poland, 2017). Nevertheless, ongoing pursuits for mandated prevention programming and training for school personnel are imperative, as they have been demonstrated as significant lifesaving and life changing legislation. 5. Addressing youth suicide in the school context The content reviewed thus far has set forth a solid foundation for the argument that increased attention must be dedicated to youth suicide in the school context. Comprehensive research on broad suicidal ity has acted as a crucial guide to informing professionals and the general public, creating more awareness and understanding surrounding the topic. It has generated helpful statistics that shed light upon specific factors that are associated with suicidal behaviors in children and ado- lescents. The identified risk factors discussed are key findings that inform suicide response practices in the school setting; best practices to target youth suicide include health promotion, prevention,
- 72. intervention, and postvention (Gould et al., 2003; Katz et al., 2013). 5.1. Prevention The World Health Organization (WHO, 2019) emphasizes the fact that while suicide is a significant public health concern, it is one that is preventable, with timely, evidence-based and at times, affordable in- terventions. The conceptualization of youth suicide as a public health problem prompted the United State to adopt a public health model of its prevention. “The public-health approach focuses on identifying patterns of suicide and suicidal behaviors in a group or population. It aims at changing the environment to protect people against diseases and changing the behaviors that put people at risk of getting them” (p. 118, Yip, 2011). While suicide is not considered a “disease” in the traditional sense, it is a significant public health concern. Moreover, given the legal implications discussed and the very real preventability of such tragic deaths, school personnel, specifically SMHPs, must understand the importance implementing suicide prevention programs via the lens of public health in order to reduce suicide risk and suicide rates among the adolescent population (Lieberman et al., 2014).
- 73. Prevention strategies for this population are traditionally completed in three domains, including community, healthcare systems, and school. The primary goal of prevention programs is to reduce the prevalence of suicidal behavior in the youth population (Katz et al., 2013). Ancillary goals include identification of at-risk individuals and the completion of appropriate referrals and treatment targeting risk factor reductions (Gould & Kramer, 2001; Gould et al., 2003). Given the sheer amount of time that youth spend in the school setting, school-based programs have been suggested as being perhaps the most effective way to reach this population (Calear et al., 2016; Miller et al., 2009). 5.1.1. School suicide prevention programs A variety of school-based suicide prevention programs exist; S. Poland and S. Ferguson Aggression and Violent Behavior xxx (xxxx) xxx 6 however, systematic reviews reveal that the field has yet to find a definitive, evidence-based, best practice guideline (Calear et al., 2016; Gould et al., 2003; Katz et al., 2013). While prevention
- 74. programming varies across design, methods, and implementation, common recom- mendations are observed across the literature. AFPS (2019) has devel- oped four evidence-based frameworks for youth in the U.S. for ensuring success of suicide prevention strategies, including gatekeeping (i.e., training those considered to be natural helpers to recognize signs and symptoms of suicide [Katz et al., 2013]), psychoeducation, restriction to access of lethal means, and provision of mental health treatment to students with depression and/or anxiety disorders, or those at risk for such disorders (Lieberman et al., 2014). Additionally, the U.S. Depart- ment of Health and Human Services Substance Abuse and Mental Health Services Administration (SAMHSA, 2012), has developed “Preventing Suicide: A Toolkit for High Schools” that outlines a plan on how to educate school personnel, students, and parents on youth suicide and related behaviors. Lieberman et al. (2014) relayed that SAMHSA’s guidelines are highly regarded methods that target the identification of at-risk youth and the use of appropriate protocols for these students. Additionally, the toolkit offers suggestions for evidence-based suicide prevention programs that are well matched for the school setting
- 75. (SAMHSA, 2012). Katz et al. (2013) comprehensive systematic literature review examined a number of school-based suicide prevention programs, including, but not limited to suicide awareness curricula, general skills training, and peer leadership. Ultimately, the investigators concluded that while there are numerous available programs, few are evidence based; importantly, the research lacks randomized controlled trial (RCT) studies that evaluate their effectiveness on the outcome of suicide. Suggestions for best practices include the combined use of multiple programs in order to address the varied and complex needs of youth suicide in the school context. Cooper et al. (2011) drew similar conclusions in their systematic review of high school-based suicide prevention programs in the United States, in which they recommended a hybrid approach that includes elements from the various programs reviewed. Of note, the authors re- ported that across the most commonly used programs, four types were isolated, including enhancement of protective factors, screening tools, gatekeeper trainings, and curriculum based. Programs that enhance protective factors were described as those that aim to identify
- 76. problem solving skills, means to adaptively cope, and the promotion of devel- opmentally appropriate mental health. As mentioned previously, gate- keeping utilizes a training approach in which school personnel and sometimes peers work to increase their skills related to the identification of and response to suicidal behavior in the school environment. Addi- tionally, screening methods, such as depression screening tools, are used to gain objective measures of student self-report of suicidality and related risk factors. Lastly, curriculum-based programs emphasize the importance of addressing mental health factors, including the use of training materials that educate school personnel on suicidality and at risk-youth (Condron et al., 2015; Cooper et al., 2011). Kalafat (2006) highlighted that while aspects of these programs are critical components of effective suicide prevention planning, there is little evidence to prove they are effective as stand-alone programs; however, these four cate- gories warrant deeper review, including a brief discussion of existing programs that fall within respective types of prevention programming. 5.1.2. Enhancement of protective factors Common protective factors for at risk youth have been
- 77. identified, including family cohesion and stability, strong coping and problem- solving skills, positive self-worth, connections to school and extracur- ricular participation, academic success, and enhanced impulse control (WHO, 2014). Self-esteem and social support are two critical protective factors that buffer the risk of suicide. When the availability of peer and family support is present, suicide risk decreases, as self-esteem increases (Eisenberg & Resnick, 2006; Kleiman & Riskind, 2013; Sharaf et al., 2009). Further, stronger levels of resiliency have been found in in- dividuals with higher self-esteem (Sharaf et al., 2009). These factors are significant in the conceptualization of youth suicide prevention plan- ning and can be enhanced in programs that emphasize protective fac- tors. Kalafat (2006) reported that research findings (Jessor et al., 1995) have demonstrated that prevention strategies targeting the enhance- ment of protective factors may be more effective than those that address risk factors. Despite this, such programs are not recommended as lone practices, as they do not fully account for the complex needs present in youth suicidality.
- 78. Promoting CARE, for example, is a school and home-based program that primarily targets the enhancement of protective factors (i.e., per- sonal and social resources) in suicide-vulnerable high school youth. It incorporates principles of behavior change maintenance as means to increase skills acquisition, motivation, social support, and self- efficacy. The program implements strategies aimed to decrease negative behav- iors via the improvement of emotional management, interconnected- ness, and coping skills. Its design is based on the empirical findings that have demonstrated that interventions that emphasize motivation to change, social support access, and self-efficacy (i.e., the confidence that an individual is equipped with the ability to face life challenge and ac- cess learned skills), increase the likelihood of skill acquisition, behav- ioral change, and continued maintenance of change (Cooper et al., 2011; Hooven et al., 2010; Hooven et al., 2012). Hooven et al. (2010) analyzed the longitudinal data of the long- term maintenance of achieved short-term changes of 615 high school youth and their parents, all of whom had participated in the Promoting CARE program in the United States. A review of the identified at-risk