Visual Inspection in Parenteral Drug Products
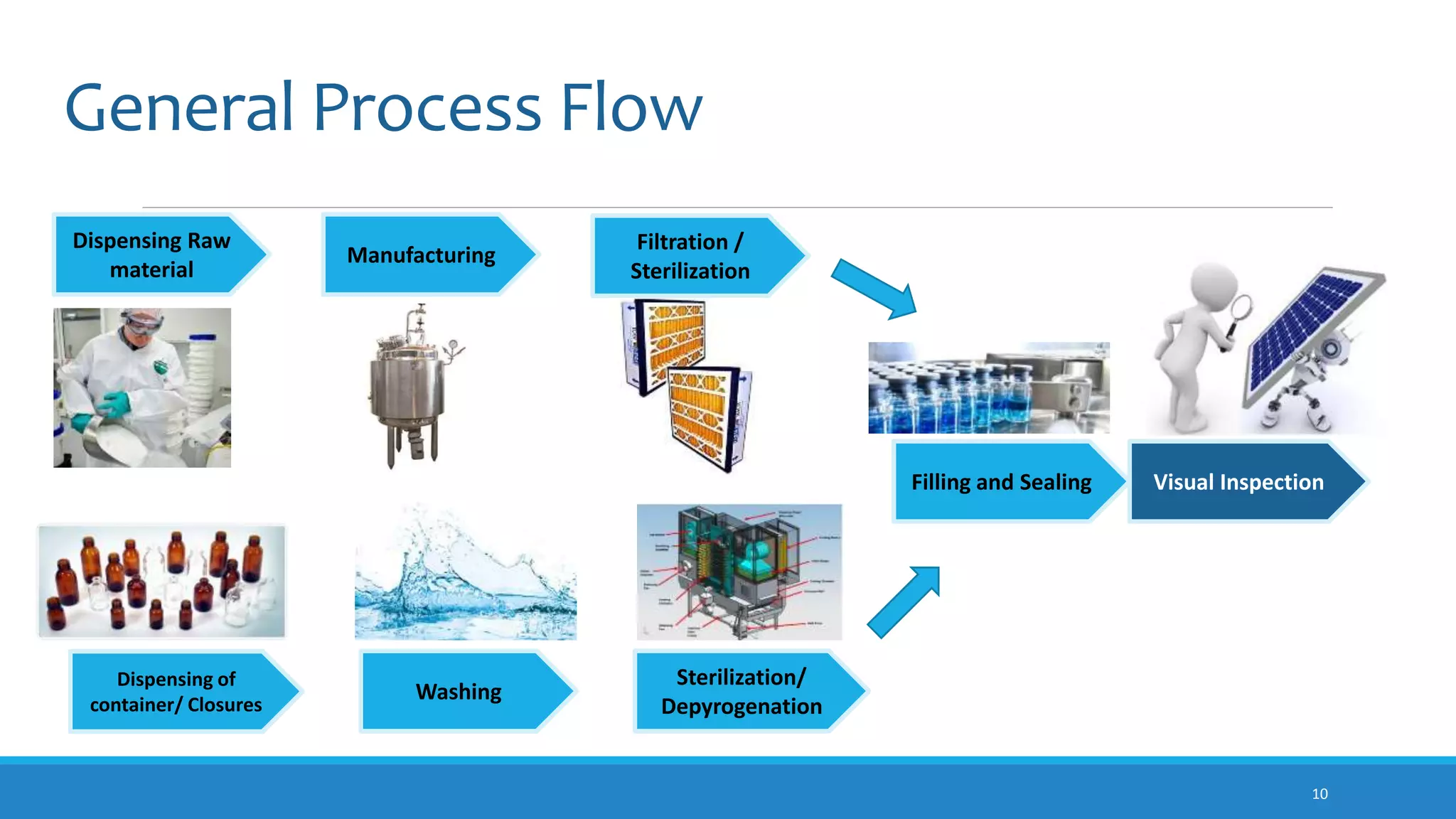
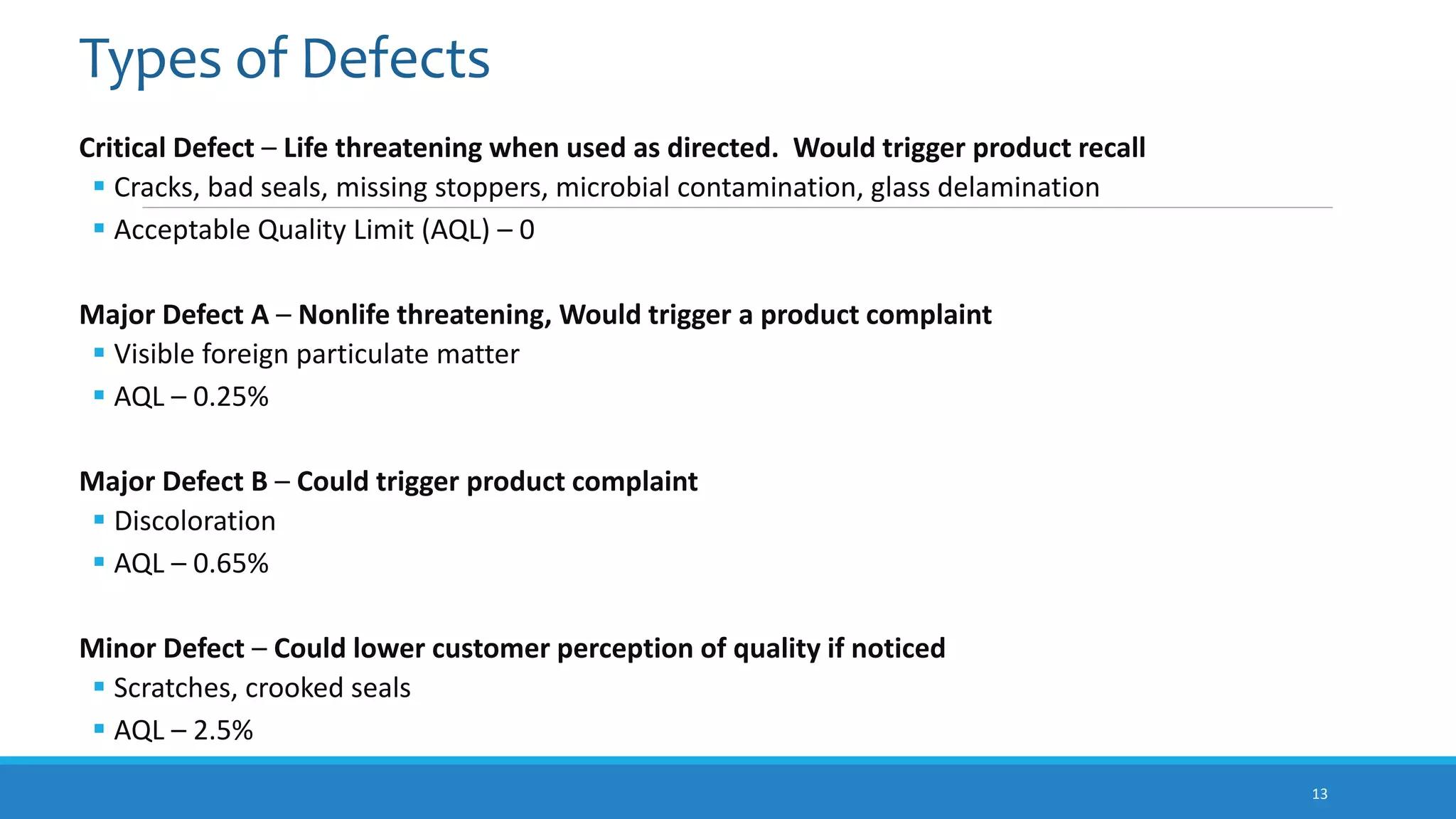
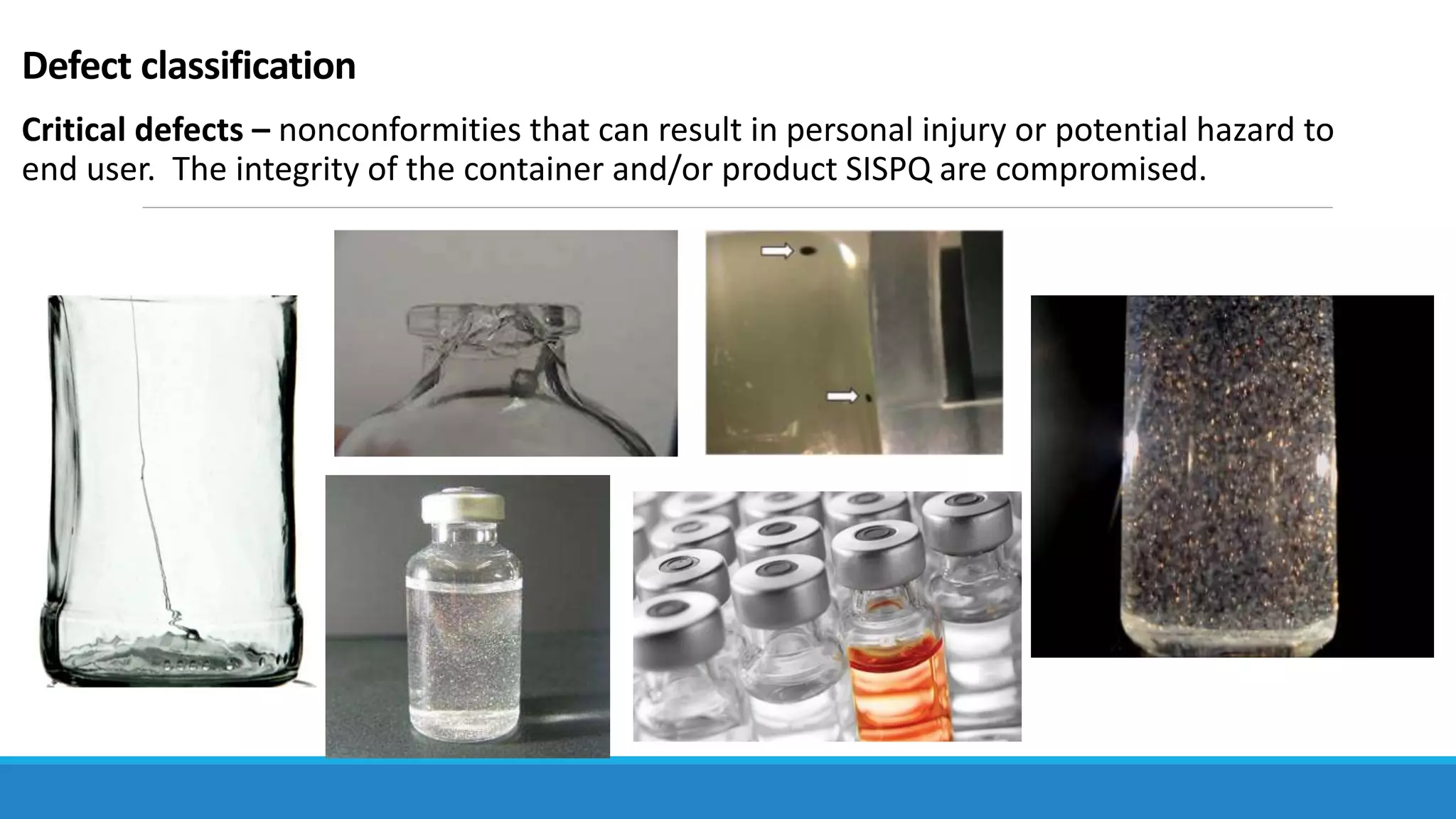
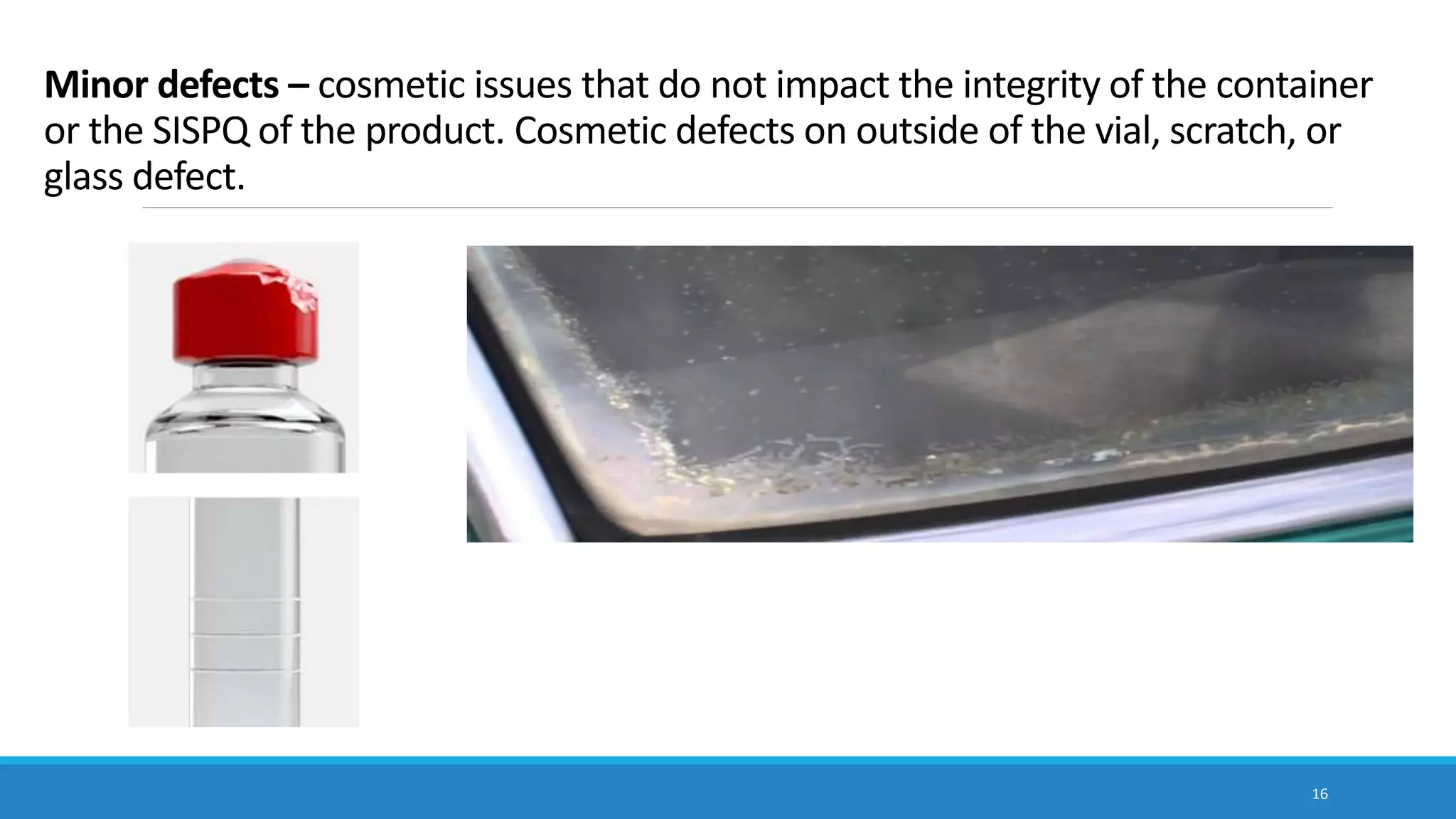
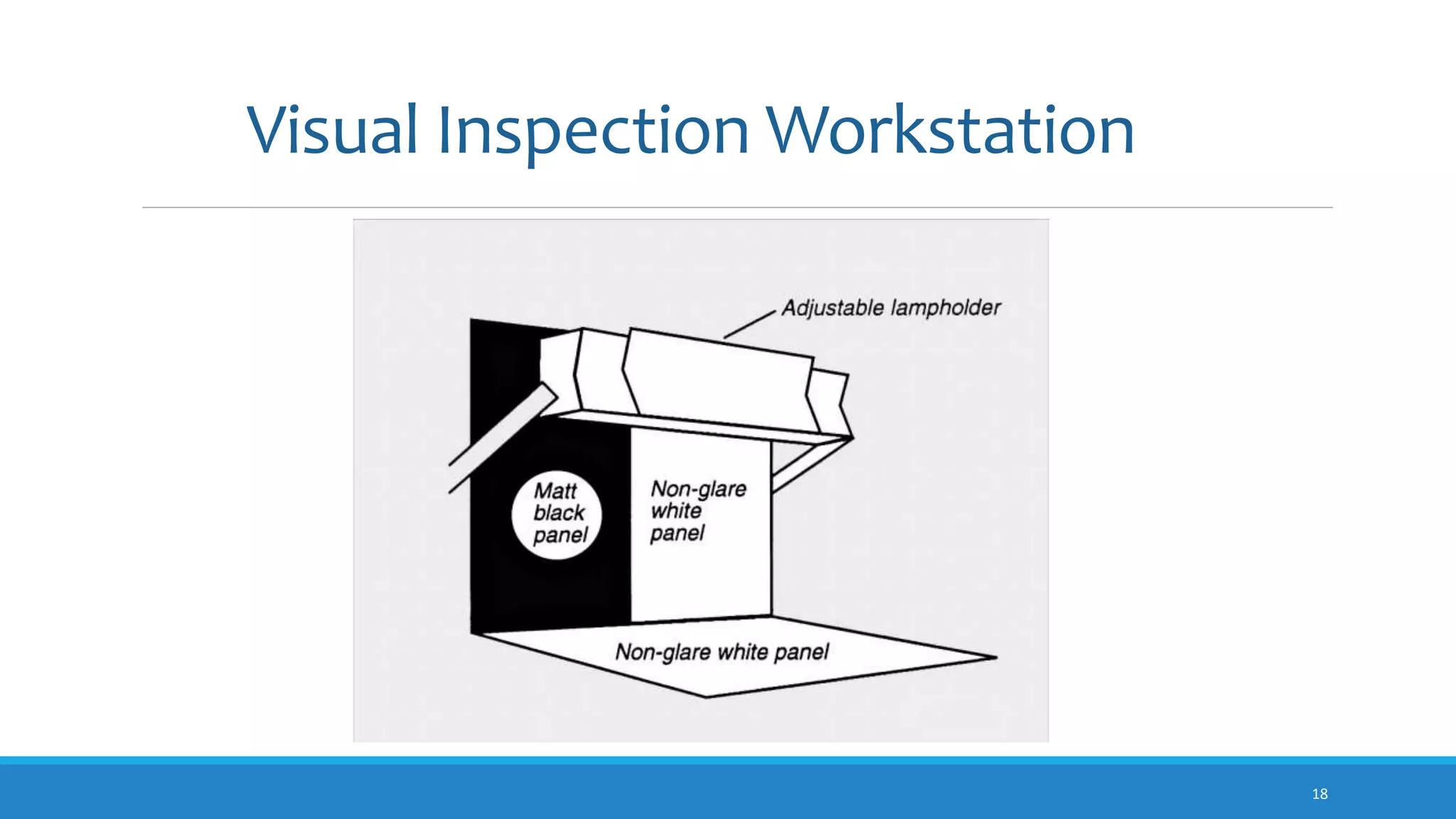
The document discusses visual inspection of parenteral drug products. It notes that visual inspection is needed to detect defects like particulate matter that could impact patient safety. Inspection is required by compendial and regulatory standards to ensure products are essentially free of visible particles. The summary describes the types of defects classified as critical, major, or minor and the acceptable quality limits for each. It also provides an overview of manual, semi-automated, and automated inspection methods and defines what constitutes a "visible particle" during the inspection process.