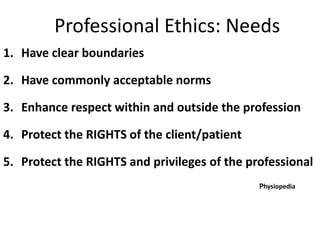
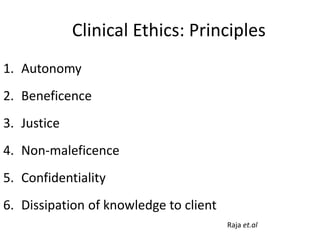
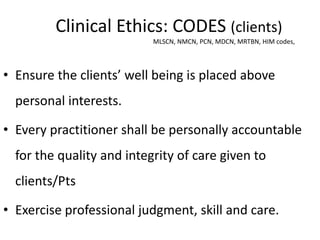
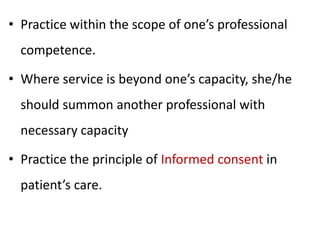
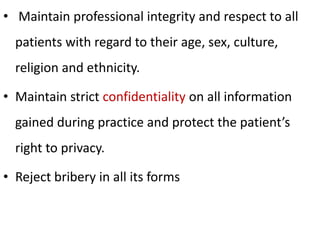
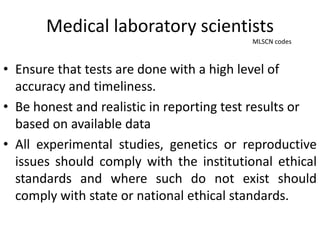
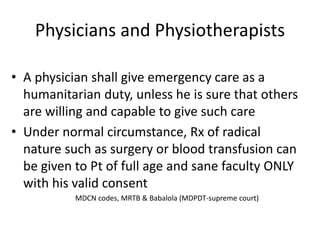
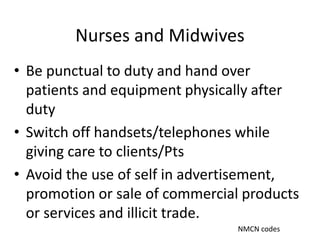
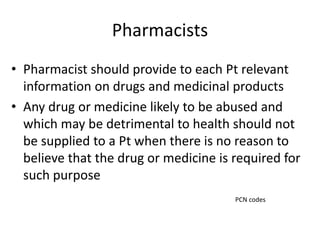
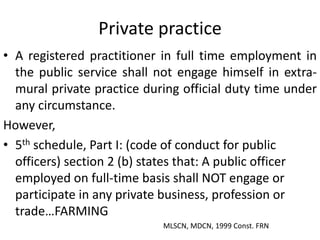
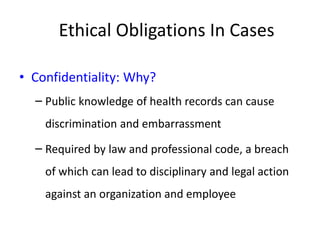
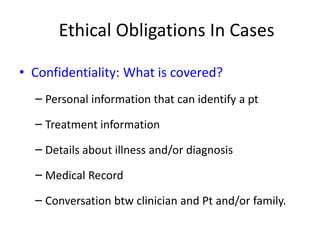
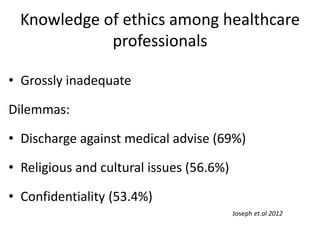
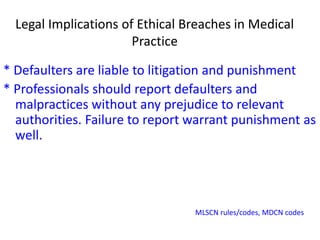
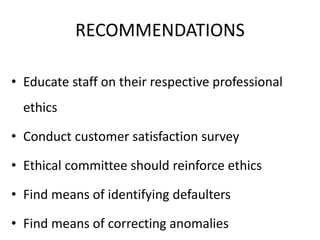
The document outlines the principles and codes of ethics that govern clinical practice for healthcare professionals in Nigeria, emphasizing the importance of patient autonomy, confidentiality, and professional conduct. It highlights the need for clear ethical boundaries and accountability among practitioners, along with the consequences of ethical breaches. Recommendations include educating staff on ethics, conducting customer satisfaction surveys, and reinforcing ethical standards within healthcare organizations.