Types and Diagnosis of Bronchiectasis
- 2. • Bronchiectasis is a long-term condition where the airways of the lungs become abnormally widened, leading to a build-up of excess mucus that can make the lungs more vulnerable to infection.
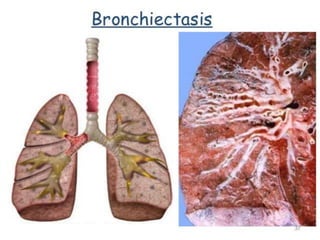
- 4. Types Of Bronchiectasis The three different types of bronchiectasis. Cylindrical or tubular bronchiectasis involves dilated airways alone. Varicose bronchiectasis is characterized by focal constrictive areas between the dilated airways. Saccular or cystic bronchiectasis is characterized by progressive dilatation of the airways, which form grape-like clusters.
- 6. Signs and symptoms • Clinical manifestations of bronchiectasis are as follows: • Cough and daily mucopurulent sputum production, often lasting months to years (classic) • Blood-streaked sputum or hemoptysis from airway damage associated with acute infection • Dyspnea, pleuritic chest pain, wheezing, fever, weakness, fatigue, and weight loss • Rarely, episodic hemoptysis with little to no sputum production (ie, dry bronchiectasis)
- 7. • Exacerbations of bronchiectasis from acute bacterial infections may produce the following signs: • Increased sputum production over baseline • Increased viscidity of sputum • A foul odor of the sputum (occasional) • Low-grade fever (rare) • Increased constitutional symptoms (eg, fatigue, malaise) • Increased dyspnea, shortness of breath, wheezing, or pleuritic pain
- 8. • Findings on physical examination are nonspecific and may include the following: • Crackles, rhonchi, scattered wheezing, and inspiratory squeaks on auscultation • Digital clubbing (2-3% of patients; more frequent in moderate-to-severe cases) • Cyanosis and plethora with polycythemia from chronic hypoxia (rare) • Wasting and weight loss • Nasal polyps and signs of chronic sinusitis • Physical stigmata of cor pulmonale, in advanced disease
- 9. Diagnostic Considerations • Investigate the possible etiology of a patient's bronchiectasis. Specifically, allergic bronchopulmonary aspergillosis, atypical mycobacterial infections, immunodeficiency states, and autoimmune diseases are causes of bronchiectasis that may be treated effectively once diagnosed. • Cystic fibrosis (CF), Young syndrome, primary ciliary dyskinesia, and alpha1-antitrypsin (AAT) deficiency require aggressive treatment, as well as genetic counseling for patients and their families. Likewise, congenital abnormalities should be identified as such for the patient and their family. • Foreign body obstruction needs to be excluded as an etiology in all patients.
- 10. Approach Considerations • In a typical patient, bronchiectasis is suspected on the basis of the clinical presentation, especially if purulent sputum is present and other conditions (eg, pneumonia, lung abscess) have been ruled out. A sputum analysis may be used to further strengthen clinical suspicion. • Radiographic studies, specifically CT scanning, then may be used to confirm the diagnosis. Once the diagnosis is confirmed, additional laboratory testing may be useful to determine the underlying cause. Although many causes are untreatable, identifying treatable conditions is paramount. In a significant percentage of patients, no readily identifiable cause is found.
- 11. • The choice of laboratory tests may vary and should be tailored to the individual patient and clinical situation. However, high-resolution CT (HRCT) scanning is the criterion standard for the diagnosis of bronchiectasis. • The anatomical distribution of bronchiectasis may be important in helping diagnose any associated condition or cause of bronchiectasis, as follows:
- 12. • Bronchiectasis as a result of infection generally involves the lower lobes, the right-middle lobe, and the lingula • Right-middle lobe involvement alone suggests right- middle lobe syndrome, an anatomic dysfunction, or a neoplastic cause with secondary mechanical obstruction • Bronchiectasis caused by cystic fibrosis (CF), Mycobacterium tuberculosis infection , or chronic fungal infections tends to affect the upper lobes, although this is not universal in CF • Allergic bronchopulmonary aspergillosis (ABPA) also affects the upper lobes but usually involves the central bronchi, whereas most other forms of bronchiectasis involve distal bronchial segments
- 14. Investigation • Computed Tomography • CXR • Sputum Analysis • CBC Count • Quantitative Immunoglobulin levels • Quantitative Alpha1-Antitrypsin Levels • Sweat Test • Aspergillus Precipitins and Serum Total IgE levels • PFT
- 15. Sputum Analysis • A sputum analysis may reinforce the diagnosis of bronchiectasis and add significant information regarding potential etiologies. A Gram stain and culture result may reveal evidence of microorganisms, including mucoid Pseudomonas species and Escherichia coli, which suggest CF but are not diagnostic.
- 16. • Chronic bronchial infection with nonmucoid Pseudomonas aeruginosa is becoming much more common in patients with non-CF bronchiectasis. The presence of eosinophils and golden plugs containing hyphae suggests Aspergillus species, although this finding alone is not diagnostic of ABPA. • Perform a smear and culture of sputum for mycobacteria and fungi. Atypical mycobacterial infection is a common cause of bronchiectasis in the older population, especially in those with underlying structural lung disease.
- 17. CBC Count • The CBC count is often abnormal in patients with bronchiectasis. Typical findings are nonspecific and include anemia and an elevated white blood cell count with an increased percentage of neutrophils. An increased percentage of eosinophils is one criterion for ABPA. Alternatively, polycythemia secondary to chronic hypoxia may be observed in advanced cases.
- 18. Quantitative Immunoglobulin levels • Quantitative immunoglobulin levels, including IgG subclasses, IgM, and IgA, are useful to exclude hypogammaglobulinemia. Note, however, that on rare occasions, bronchiectasis may be seen in patients with antibody production deficiency but normal to low-normal IgG levels. In situations such as these, evaluating antibody response to Haemophilus influenzae and pneumococcal vaccines may be useful.
- 19. Quantitative Alpha1-Antitrypsin Levels • Quantitative serum alpha1-antitrypsin (AAT) levels are used to rule out AAT deficiency. In addition to a suggestive family history, clinical features of emphysema that suggest the possibility of AAT deficiency and the need for serum testing include onset at an early age (45 y or less) and the absence of a recognized risk factor (eg, smoking, occupational dust exposure).
- 20. Sweat Test • sweat test was the criterion standard test to evaluate for CF. However, genetic analysis has now become standard and may be performed to look for evidence of mutations consistent with CF and to look for potential variants, such as Young syndrome Aspergillus Precipitins and Serum Total IgE levels • Aspergillus precipitins and serum total IgE levels are important in making the diagnosis of ABPA. Diagnostic criteria for ABPA include a total serum IgE level greater than 1000 IU/mL or a greater than 2-fold rise from baseline.
- 21. Computed Tomography • CT scanning , particularly high-resolution CT (HRCT) scanning of the chest, has replaced bronchography as the defining modality of bronchiectasis. CT sensitivity and specificity reportedly are 84-97% and 82-99%, respectively, but may be higher at referral centers. • Additional advantages of HRCT scanning include noninvasiveness, avoidance of possible allergic reactions to contrast media, and information regarding other pulmonary processes. The 3 forms of bronchiectasis in the Reid classification can be visualized by HRCT.
- 22. The following are aspects of CT findings in bronchiectasis: • Cylindrical bronchiectasis has parallel tram track lines, or it may have a signet-ring appearance composed of a dilated bronchus cut in a horizontal section with an adjacent pulmonary artery representing the stone • The diameter of the bronchus lumen is normally 1-1.5 times that of the adjacent vessel; a diameter greater than 1.5 times that of the adjacent vessel is suggestive of bronchiectasis • Varicose bronchiectasis has irregular or beaded bronchi, with alternating areas of dilatation and constriction • Cystic bronchiectasis has large cystic spaces and a honeycomb appearance; this contrasts with the blebs of emphysema, which have thinner walls and are not accompanied by proximal airway abnormalities
- 29. Radiography • Posterior-anterior and lateral chest radiographs should be obtained in all patients. Expected general findings include increased pulmonary markings, honeycombing, atelectasis, and pleural changes. Specific findings may include linear lucencies and parallel markings radiating from the hila (tram tracking) in cylindrical bronchiectasis, dilated bronchi in varicose bronchiectasis, and clustered cysts in cystic bronchiectasis. In the appropriate clinical setting, chest radiograph findings are occasionally sufficient for confirming the diagnosis of bronchiectasis.
- 33. Pulmonary Function Tests • Pulmonary function test results may be normal or abnormal and may reflect underlying comorbidities as well as providing information regarding predisposing conditions. These tests are useful in obtaining a functional assessment of the patient, as well as allowing for objective determination of the deterioration of a patient's pulmonary function when baseline studies are available.
- 34. • The most common abnormality is an obstructive airway defect, which may even be found in patients without a prior smoking history. In addition, patients with bronchiectasis have higher rates of yearly decline in forced expiratory volume in 1 second (FEV1) than patients without bronchiectasis. In patients with non-CF bronchiectasis, risk factors for a more rapid decline in FEV1 include colonization with Pseudomonas aeruginosa and higher concentrations of proinflammatory markers. • Obstruction in bronchiectasis is not usually reversible with bronchodilator therapy. However, a subgroup of patients may develop hyperreactive airways in conjunction with their bronchiectasis that will respond to bronchodilators. • Restriction may be observed in patients with severe advanced disease secondary to scarring and atelectasis, but this is not common. Traction bronchiectasis most often occurs in the setting of a restrictive lung defect from underlying fibrosis.
- 35. Approach Considerations • The goals of therapy are to improve symptoms, to reduce complications, to control exacerbations, and to reduce morbidity and mortality. Early recognition is essential in bronchiectasis and associated conditions. Additionally, management of underlying conditions, which may include the use of intravenous immunoglobulin or intravenous alpha1- antitrypsin (AAT) therapy, is essential to the overall treatment. • Antibiotics and chest physiotherapy are the mainstay modalities. Other modalities (beyond those for specific associated conditions) may include bronchodilators, corticosteroid therapy, dietary supplementation, and oxygen or surgical therapies. Admitting patients with severe exacerbations of bronchiectasis to the hospital and treating them with intravenous antibiotics, bronchodilators, aggressive physiotherapy, and supplemental nutrition is not uncommon.
- 36. Supportive Treatment • The following general measures are recommended: • Smoking cessation • Avoidance of second-hand smoke • Adequate nutritional intake with supplementation, if necessary • Immunizations for influenza and pneumococcal pneumonia • Confirmation of immunizations for measles, rubeola, and pertussis • Oxygen therapy is reserved for patients who are hypoxemic with severe disease and end-stage complications, such as cor pulmonale
- 37. • Antibiotic Therapy • Antibiotics have been the mainstay of treatment for more than 40 years. Oral, parenteral, and aerosolized antibiotics are used, depending on the clinical situation. • In acute exacerbations, broad-spectrum antibacterial agents are generally preferred. However, if time and the clinical situation allows, sampling of respiratory secretions during an acute exacerbation may allow treatment with antibiotics based on specific species identification. • Acceptable choices for the outpatient who is mild to moderately ill include any of the following: • Amoxicillin • Tetracycline • Trimethoprim-sulfamethoxazol • A newer macrolide (eg, azithromycin or clarithromycin) • A second-generation cephalosporin • A fluoroquinolone
- 38. • In general, the duration of antibiotic therapy for mild to moderate illness is 7-10 days. • For patients with moderate-to-severe symptoms, parenteral antibiotics, such as an aminoglycoside (gentamicin, tobramycin) and an antipseudomonal synthetic penicillin, a third-generation cephalosporin, or a fluoroquinolone, may be indicated. Patients with bronchiectasis from CF are often infected with mucoid Pseudomonas species, and, as such, tobramycin is often the drug of choice for acute exacerbation.
- 39. Regular antibiotic regimens • Some patients with chronic bronchial infections may need regular antibiotic treatment to control the infectious process. Some clinicians prefer to prescribe antibiotics on a regular basis or for a set number of weeks each month. • The oral antibiotics of choice are the same as those mentioned previously. Potential regimens include daily antibiotics for 7-14 days of each month, alternating antibiotics for 7-10 days with antibiotic-free periods of 7-10 days, or a long-term daily dose of antibiotics. For patients with severe CF and bronchiectasis, intermittent courses of intravenous antibiotics are sometimes used
- 40. Bronchial Hygiene • Good bronchial hygiene is paramount in the treatment of bronchiectasis, because of the tenacious sputum and defects in clearance of mucus in these patients. Postural drainage with percussion and vibration is used to loosen and mobilize secretions. • Devices available to assist with mucus clearance include flutter devices, intrapulmonic percussive ventilation devices, and incentive spirometry. Although consistent benefits from these techniques are lacking and vary with patient motivation and knowledge, a review did report improvement in patients’ cough- related quality of life scores. • A relatively new device called the "Vest" system is a pneumatic compression device/vest that is worn by the patient periodically throughout the day. It is essentially technique independent and has variable success, especially in patients with CF.
- 42. Vest system
- 43. Anti-inflammatory Therapy • The use of anti-inflammatory therapy is to modify the inflammatory response caused by the microorganisms associated with bronchiectasis and subsequently reduce the amount of tissue damage. Inhaled corticosteroids, oral corticosteroids,leukotriene inhibitors,and nonsteroidal anti-inflammatory agents have all been examined. • Azithromycin has known anti-inflammatory properties and long-term use has been studied in patients with both CF and non-CF bronchiectasis. In non-CF patients, azithromycin has been shown to decrease exacerbations and improve spirometry and microbiologic profiles. In CF patients a meta-analysis suggests that it improves lung function, especially in those patients colonized with Pseudomonas
- 44. Adjunctive Surgical Resection • Surgery is an important adjunct to therapy in some patients with advanced or complicated disease. Surgical resection for bronchiectasis can be performed with acceptable morbidity and mortality in patients of any age. Lung Transplantation • Single- or double-lung transplantation has been used as treatment of severe bronchiectasis, predominantly when related to CF. In general, consider patients with CF and bronchiectasis for lung transplantation when FEV1 falls below 30% of the predicted value.