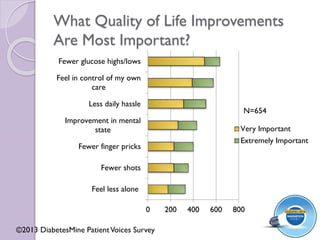
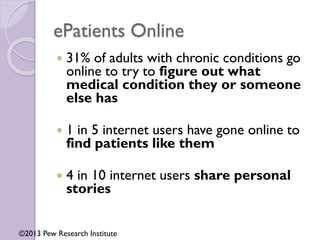
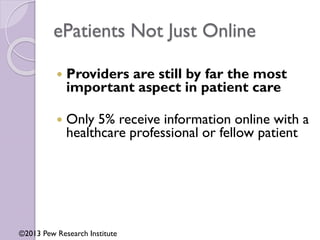
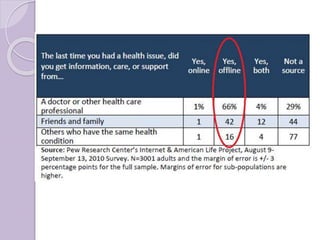
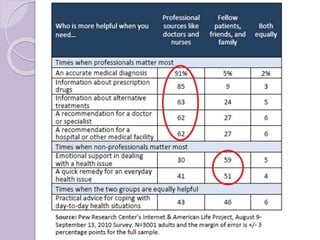
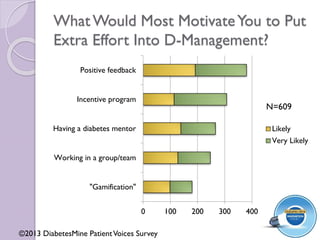
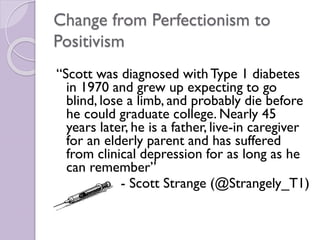
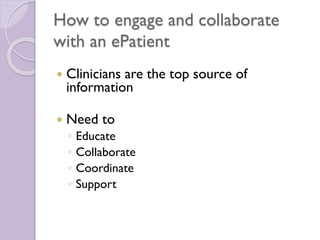
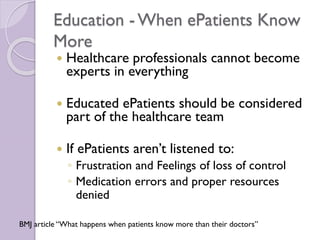
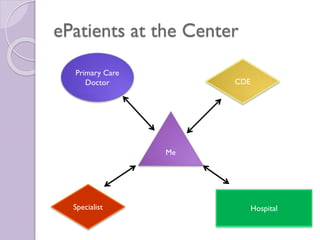
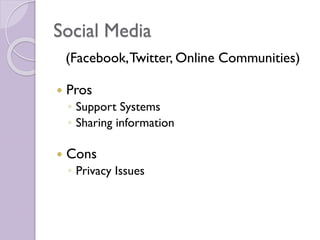
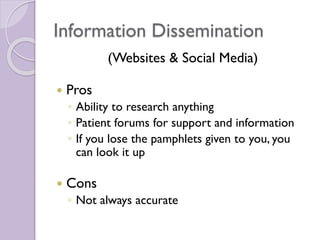
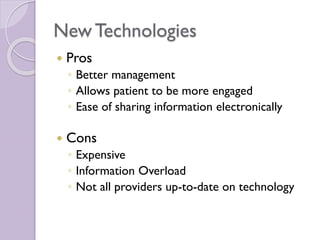
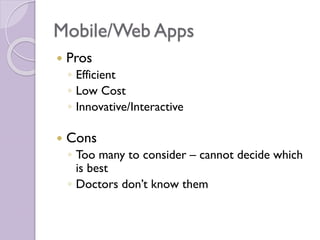
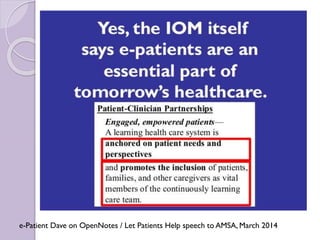
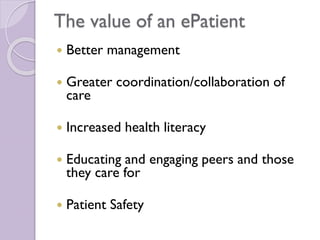
This document discusses the experiences and perspectives of an ePatient named Erin Gilmer. An ePatient is someone who is equipped, enabled, empowered and engaged in their own health care through online resources and digital technologies. The document outlines Erin's journey of coping with multiple chronic conditions and becoming more involved in her own care management. It also explores how ePatients access health information online, use tools like social media and apps, and want to collaborate as partners with their healthcare providers. Both the opportunities and challenges of new technologies for patients and providers are examined.