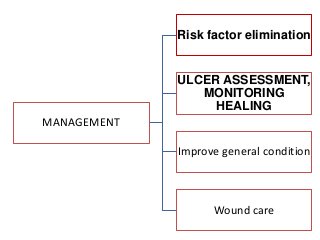
This document defines pressure ulcers, discusses their pathogenesis and risk factors, and outlines their classification and management. Key points:
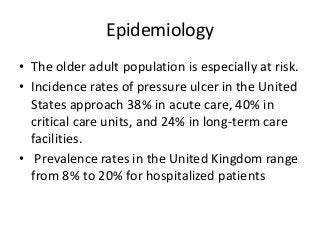
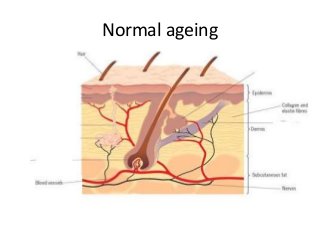
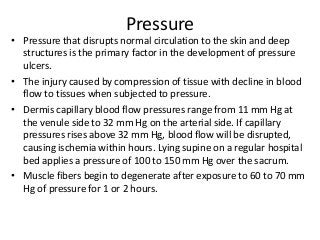
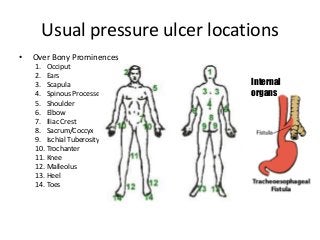
- Pressure ulcers are localized skin injuries caused by pressure that disrupts blood flow, often over bony prominences. The elderly are especially at risk.
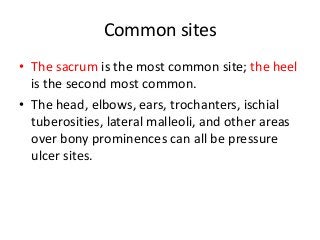
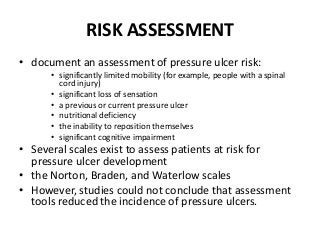
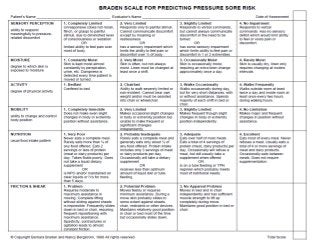
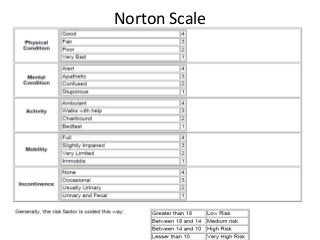
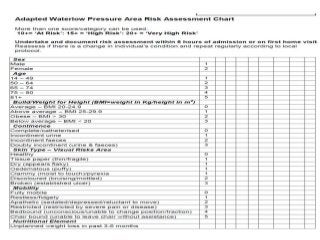
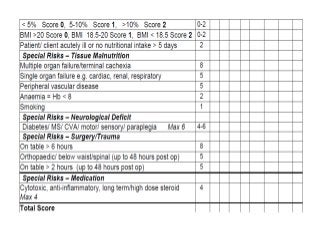
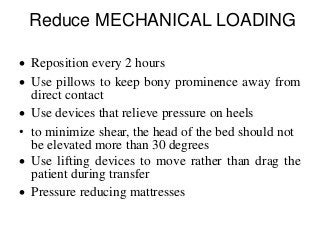
- Risk factors include immobility, sensory impairment, malnutrition, moisture, shear and friction forces on the skin. Common sites are the sacrum and heels.
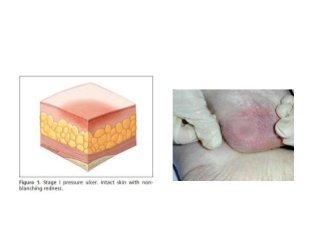
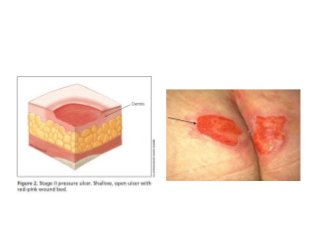
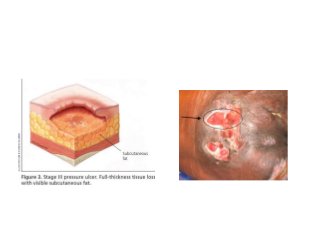
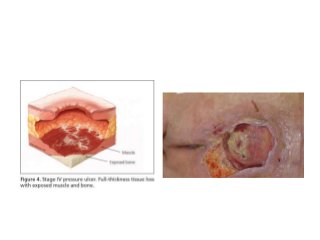
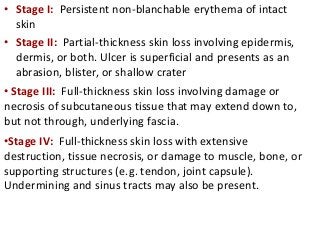
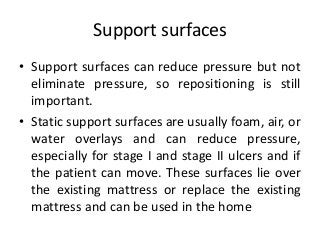
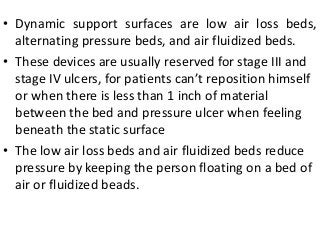
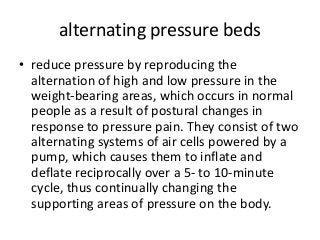
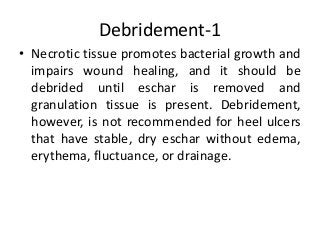
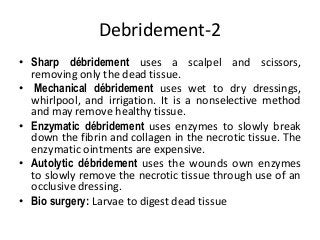
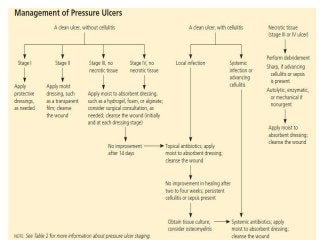
- Pressure ulcers are classified in stages from I to IV based on tissue damage depth. Prevention focuses on pressure reduction through repositioning, support surfaces, and skin care. Treatment involves dressing, debridement and wound healing promotion.





![Wound cleansing
• Wound cleansing should be done with tap water
or saline.
• Wounds should be cleansed initially and with
each dressing change. U se of a 35-mL syringe
and 19-gauge angiocatheter provides a degree of
force that is effective yet safe;
• Wound cleansing with antiseptic agents (e.g.,
povidone-iodine [Betadine], hydrogen peroxide,
acetic acid) should be avoided because they
destroy granulation tissue](https://image.slidesharecdn.com/pressureulcer-150111101318-conversion-gate02/85/Pressure-ulcer-62-320.jpg?cb=1676626658)



![Growth factors
• (e.g., platelet-derived growth factor becaplermin
[Regranex]).
• PDGF promotes chemotaxis of neutrophils, monocytes
and smooth muscle cells in wounds. Topical
application of recombinant PDGF speeds wound
healing and promotes granulation tissue formation,
synthesis of extracellular matrix and the inflammatory
phase of the wound healing process.
• PDGF promotes cutaneous wound healing by
increasing proliferation and migration of dermal
fibroblasts and extracellular matrix deposition](https://image.slidesharecdn.com/pressureulcer-150111101318-conversion-gate02/85/Pressure-ulcer-79-320.jpg?cb=1676626658)