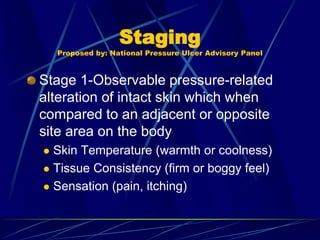
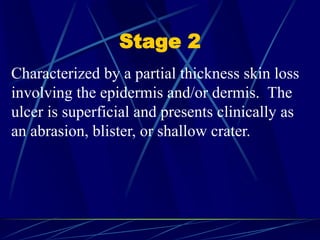
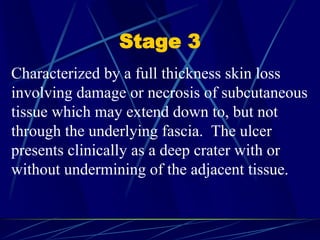
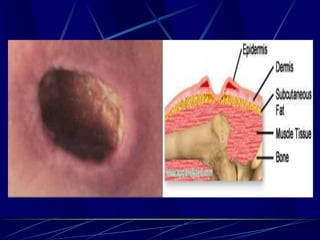
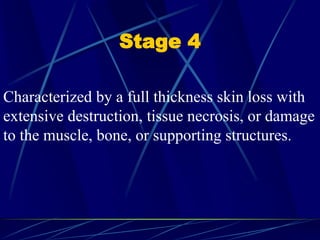
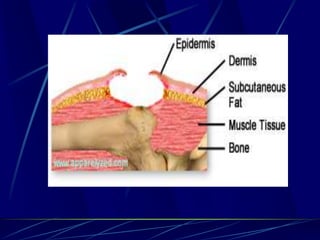
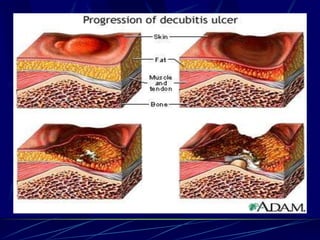
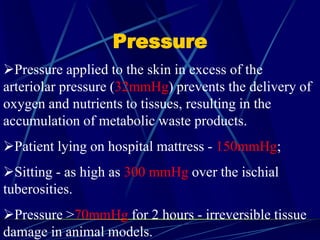
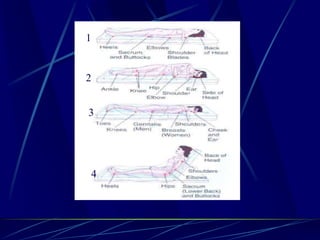
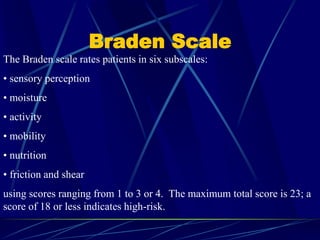
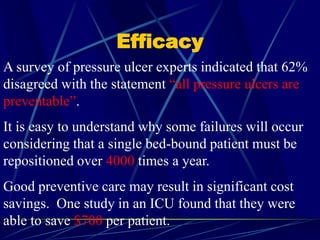
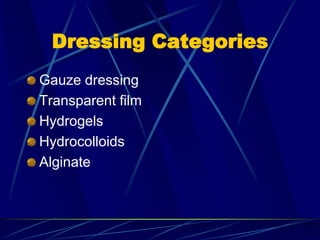
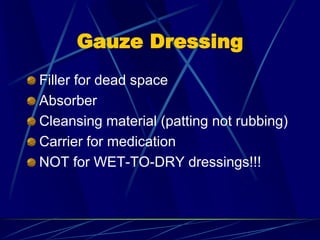
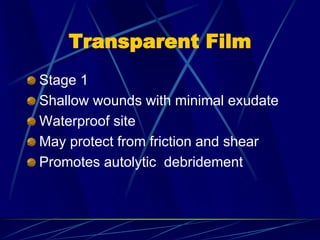
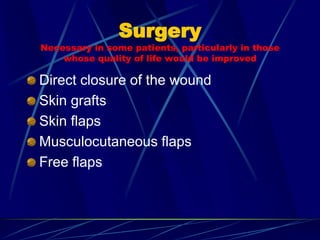
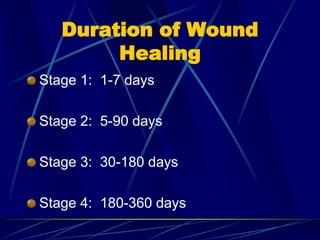
This document provides information on pressure ulcers/sores, including their definition, stages, risk factors, prevention, and treatment. It discusses how pressure ulcers develop from prolonged pressure on soft tissue over bony prominences, and outlines 4 stages based on tissue depth involvement. Key risk factors include immobility, incontinence, and nutritional status. Prevention focuses on pressure relief through repositioning and support surfaces. Treatment involves wound cleaning, debridement of necrotic tissue, and dressings to promote healing.