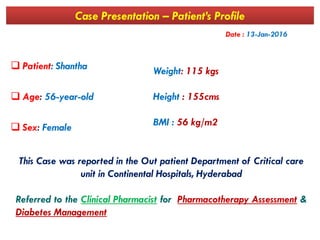
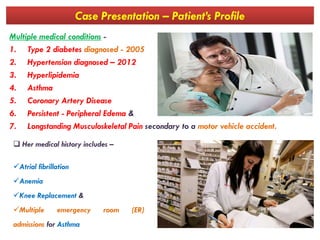
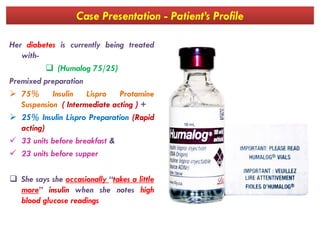
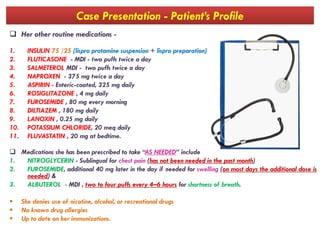
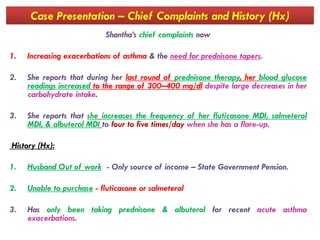
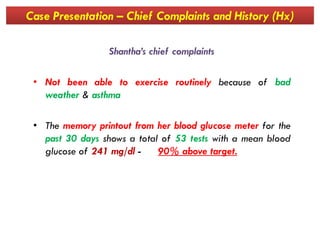
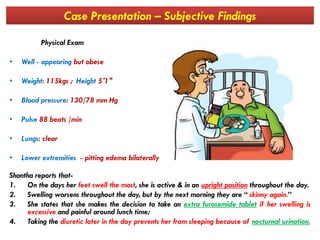
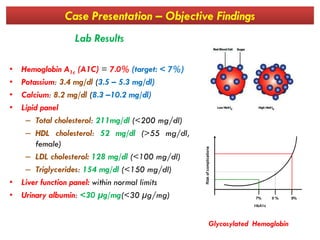
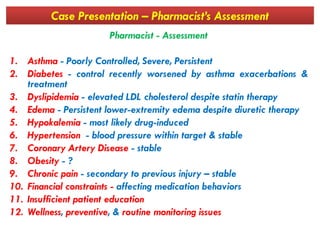
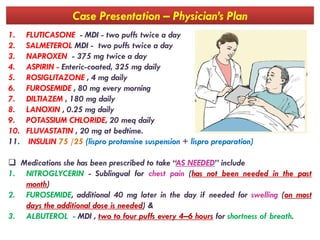
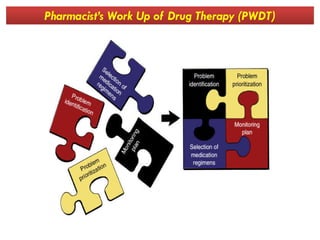
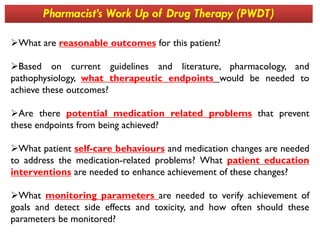
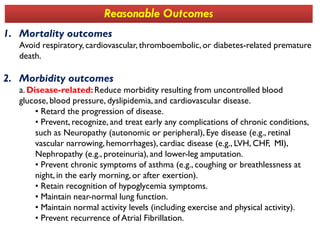
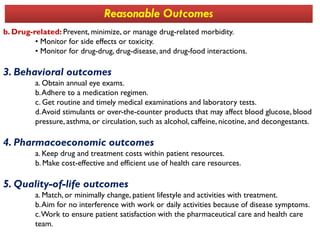
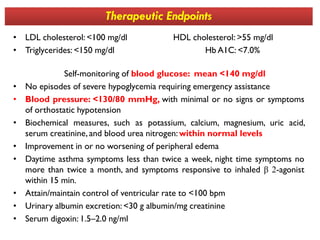
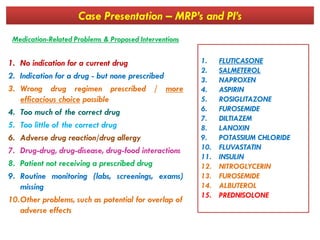
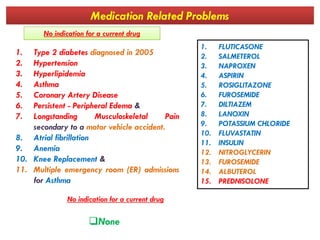
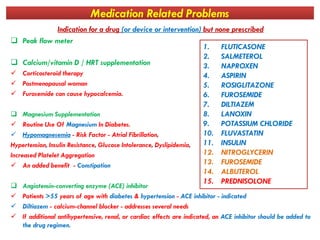
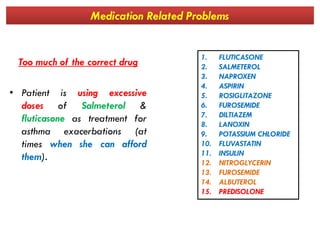
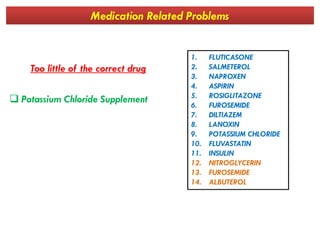
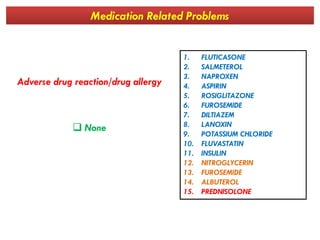
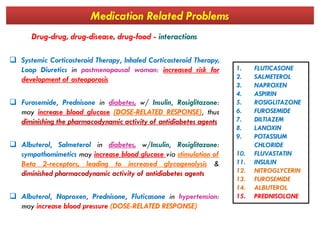
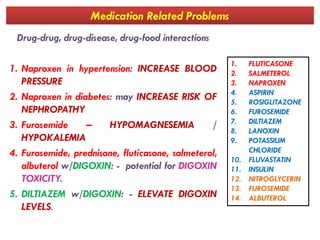
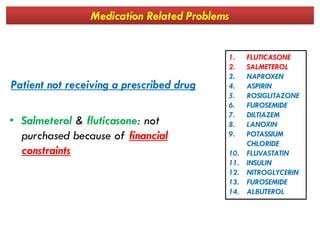
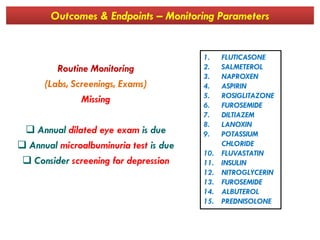
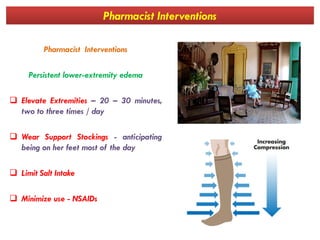
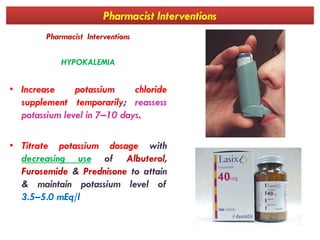
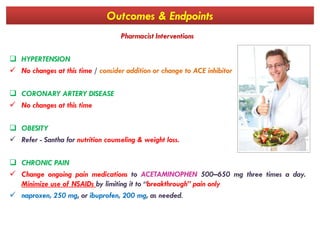
The document details a case presentation of a 56-year-old female patient, Shantha, with multiple chronic conditions including type 2 diabetes and asthma, who is facing challenges with medication adherence due to financial constraints and worsening health issues. It includes a comprehensive overview of her medical history, current medications, chief complaints, and results from the pharmacist's assessment, as well as proposed pharmaceutical interventions and therapeutic endpoints. The analysis emphasizes the importance of addressing medication-related problems and enhancing patient education to improve health outcomes.