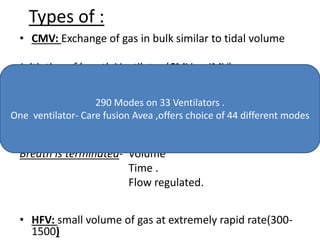
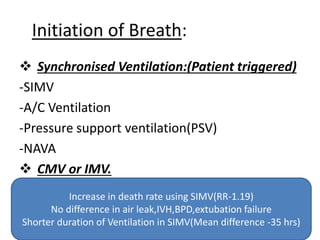
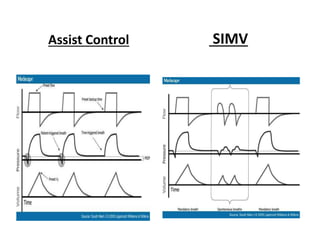
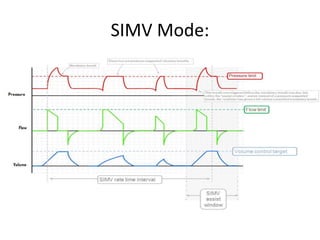
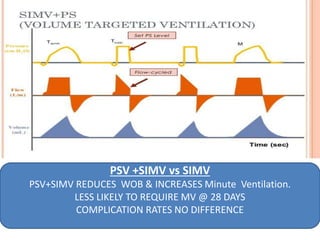
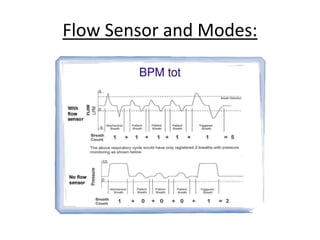
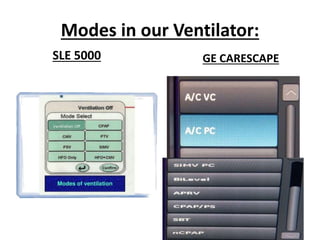
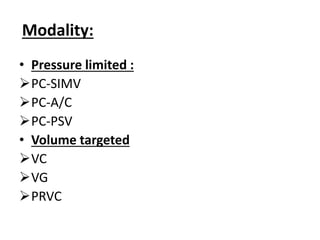
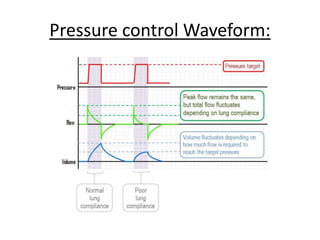
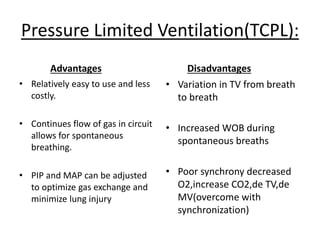
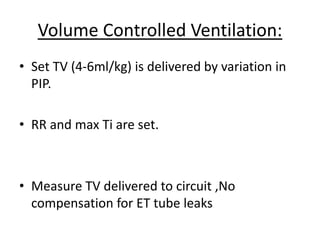
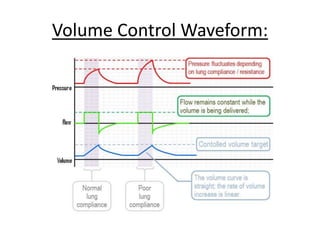
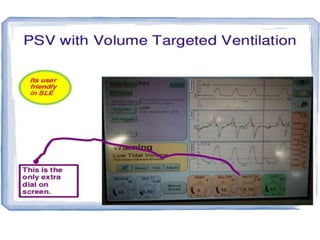
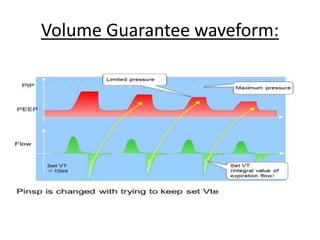
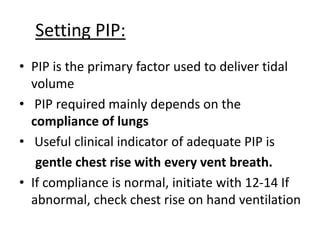
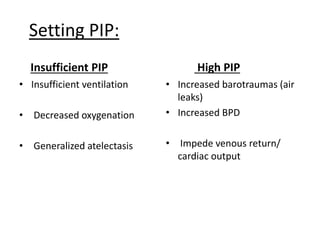
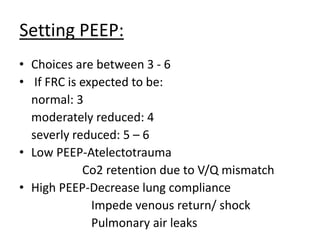
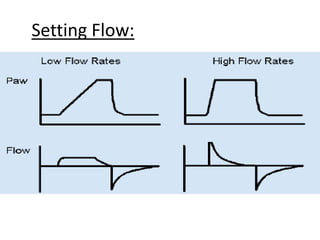
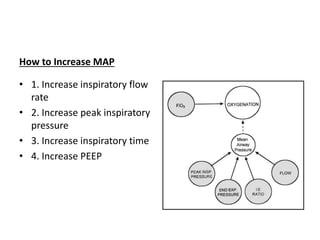
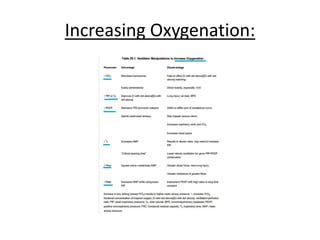
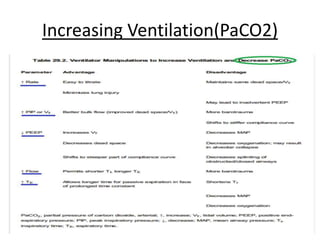
This document discusses neonatal mechanical ventilation. It begins by introducing mechanical ventilation and its importance in improving neonatal survival since the 1960s. It then discusses the benefits of mechanical ventilation in improving gas exchange and decreasing work of breathing. Various indications for ventilation are provided. Common conditions requiring ventilation are also listed. The document goes on to describe different types of ventilators and modes, how to initiate a breath, and studies comparing different modes. It concludes by discussing parameters for conventional ventilation like PIP, PEEP, flow rates, and methods for controlling oxygenation and ventilation.