Syncope
•Download as PPTX, PDF•
13 likes•1,721 views
Syncope
Report
Share
Report
Share
More Related Content
What's hot
What's hot (20)
Similar to Syncope
Similar to Syncope (20)
03 Samir Rafla-Sudden Cardiac Death and Resuscitation.ppt

03 Samir Rafla-Sudden Cardiac Death and Resuscitation.ppt
More from Ramachandra Barik
More from Ramachandra Barik (20)
A Case of Device Closure of an Eccentric Atrial Septal Defect Using a Large D...

A Case of Device Closure of an Eccentric Atrial Septal Defect Using a Large D...
Trio of Rheumatic Mitral Stenosis, Right Posterior Septal Accessory Pathway a...

Trio of Rheumatic Mitral Stenosis, Right Posterior Septal Accessory Pathway a...
Recently uploaded
Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...

Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...Call Girls in Nagpur High Profile
Recently uploaded (20)
Top Rated Bangalore Call Girls Mg Road ⟟ 8250192130 ⟟ Call Me For Genuine Sex...

Top Rated Bangalore Call Girls Mg Road ⟟ 8250192130 ⟟ Call Me For Genuine Sex...
(👑VVIP ISHAAN ) Russian Call Girls Service Navi Mumbai🖕9920874524🖕Independent...

(👑VVIP ISHAAN ) Russian Call Girls Service Navi Mumbai🖕9920874524🖕Independent...
Call Girls Ludhiana Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Ludhiana Just Call 9907093804 Top Class Call Girl Service Available
💎VVIP Kolkata Call Girls Parganas🩱7001035870🩱Independent Girl ( Ac Rooms Avai...

💎VVIP Kolkata Call Girls Parganas🩱7001035870🩱Independent Girl ( Ac Rooms Avai...
Night 7k to 12k Navi Mumbai Call Girl Photo 👉 BOOK NOW 9833363713 👈 ♀️ night ...

Night 7k to 12k Navi Mumbai Call Girl Photo 👉 BOOK NOW 9833363713 👈 ♀️ night ...
Call Girls Varanasi Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Varanasi Just Call 9907093804 Top Class Call Girl Service Available
Call Girls Dehradun Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Dehradun Just Call 9907093804 Top Class Call Girl Service Available
Lucknow Call girls - 8800925952 - 24x7 service with hotel room

Lucknow Call girls - 8800925952 - 24x7 service with hotel room
Night 7k to 12k Chennai City Center Call Girls 👉👉 7427069034⭐⭐ 100% Genuine E...

Night 7k to 12k Chennai City Center Call Girls 👉👉 7427069034⭐⭐ 100% Genuine E...
Call Girls Haridwar Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Haridwar Just Call 9907093804 Top Class Call Girl Service Available
Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...

Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...
Call Girls Bhubaneswar Just Call 9907093804 Top Class Call Girl Service Avail...

Call Girls Bhubaneswar Just Call 9907093804 Top Class Call Girl Service Avail...
Russian Escorts Girls Nehru Place ZINATHI 🔝9711199012 ☪ 24/7 Call Girls Delhi

Russian Escorts Girls Nehru Place ZINATHI 🔝9711199012 ☪ 24/7 Call Girls Delhi
Call Girls Bangalore Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Bangalore Just Call 9907093804 Top Class Call Girl Service Available
Call Girls Horamavu WhatsApp Number 7001035870 Meeting With Bangalore Escorts

Call Girls Horamavu WhatsApp Number 7001035870 Meeting With Bangalore Escorts
Top Rated Hyderabad Call Girls Erragadda ⟟ 6297143586 ⟟ Call Me For Genuine ...

Top Rated Hyderabad Call Girls Erragadda ⟟ 6297143586 ⟟ Call Me For Genuine ...
VIP Service Call Girls Sindhi Colony 📳 7877925207 For 18+ VIP Call Girl At Th...

VIP Service Call Girls Sindhi Colony 📳 7877925207 For 18+ VIP Call Girl At Th...
Best Rate (Hyderabad) Call Girls Jahanuma ⟟ 8250192130 ⟟ High Class Call Girl...

Best Rate (Hyderabad) Call Girls Jahanuma ⟟ 8250192130 ⟟ High Class Call Girl...
Premium Call Girls Cottonpet Whatsapp 7001035870 Independent Escort Service

Premium Call Girls Cottonpet Whatsapp 7001035870 Independent Escort Service
Call Girls Visakhapatnam Just Call 9907093804 Top Class Call Girl Service Ava...

Call Girls Visakhapatnam Just Call 9907093804 Top Class Call Girl Service Ava...
Syncope
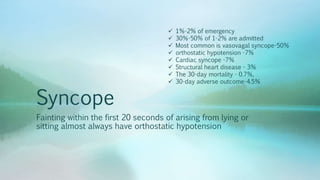
- 1. Syncope Fainting within the first 20 seconds of arising from lying or sitting almost always have orthostatic hypotension 1%-2% of emergency 30%-50% of 1-2% are admitted Most common is vasovagal syncope-50% orthostatic hypotension -7% Cardiac syncope -7% Structural heart disease - 3% The 30-day mortality - 0.7%, 30-day adverse outcome-4.5%
- 2. Define • Syncope – transient – loss of consciousness – rapid onset – short duration, – spontaneous recovery, – associated with at least 1 of – (1) Specific forms of syncope (like vasovagal syncope); and/or – (2) the absence of features suggesting another cause of loss of consciousness (like epileptic convulsions or hypoglycemia).
- 3. Aim Structural substrate ? Risk factors? Syncope spell detail? Induce syncope under controlled conditions(Tilt table)
- 4. Tests Beyond an electrocardiogram are not usually needed The most commonly used tests implantable loop recorders-30-40% diagnosis in 2-3 yrs Tilt table testing Neither are needed most of the time A good history provides more useful and more accurate information in most
- 5. History • 4 distinct phases (1) the context before symptoms; (2) prodromal symptoms (3) how the patient felt afterward (4)Try to get a bystander • Vasovagal syncope and orthostatic vs from arrhythmic • Strenuous exertion –Arrhythmias
- 6. Physical Examination • No physical findings are completely diagnostic of syncope or its causes – aortic stenosis – hypertrophic cardiomyopathy – dilated left ventricle – carotid sinus supersenistivity, – orthostatic hypotension.
- 7. High risk markers for syncope
- 9. Risk score
- 10. Diagnostic Tests • Positive - 1%-4%
- 11. 12-lead ECG • Low detection • Inexpensive • Detects – Conduction disease – repolarization abnormalities – QT prolongation/abbreviation, – ischemic heart disease – ventricular hypertrophy – Brugada, ARVD – Cardiomyopathy –
- 12. ECG monitoring • Arrhythmic • Low detection rate • Telemetry – Structural heart disease – High risk of arrhythmic events – 72-hour :16% – 1 month -12% • Loop recorders : 30%-40% of patients are detected over 2-3 years.
- 13. Echocardiography • Structural heart disease.
- 14. Tilt Table test • The most common provocative test • The goal is to trigger clinically reminiscent presyncope or syncope • Result of hypotension or bradycardia or both
- 15. To avoid syncope during MRI
