Ar medical conditions and dental care-dental toxicology
•Download as PPT, PDF•
7 likes•1,487 views
Report
Share
Report
Share
Recommended
Recommended
More Related Content
What's hot
What's hot (20)
ROLE OF PHARMACIST IN PREVENTION & MANAGEMENT OF DRUG INTERACTIONS

ROLE OF PHARMACIST IN PREVENTION & MANAGEMENT OF DRUG INTERACTIONS
Viewers also liked
Viewers also liked (20)
Management of patient with hepatic disorder in dental office (hepatitis, alco...

Management of patient with hepatic disorder in dental office (hepatitis, alco...
SELF MEDICATION PRACTICES FOR ORAL HEALTH PROBLEMS AMONG DENTAL PATIENTS IN B...

SELF MEDICATION PRACTICES FOR ORAL HEALTH PROBLEMS AMONG DENTAL PATIENTS IN B...
General Chemistry and Inorganic Pharmaceutical Chemistry Module 1 Pharmacist ...

General Chemistry and Inorganic Pharmaceutical Chemistry Module 1 Pharmacist ...
Similar to Ar medical conditions and dental care-dental toxicology
Similar to Ar medical conditions and dental care-dental toxicology (20)
Hazards of OTC medication - a community pharmacy practice

Hazards of OTC medication - a community pharmacy practice
More from Iyad Abou Rabii
More from Iyad Abou Rabii (20)
Recently uploaded
Model Call Girl Services in Delhi reach out to us at 🔝 9953056974 🔝✔️✔️
Our agency presents a selection of young, charming call girls available for bookings at Oyo Hotels. Experience high-class escort services at pocket-friendly rates, with our female escorts exuding both beauty and a delightful personality, ready to meet your desires. Whether it's Housewives, College girls, Russian girls, Muslim girls, or any other preference, we offer a diverse range of options to cater to your tastes.
We provide both in-call and out-call services for your convenience. Our in-call location in Delhi ensures cleanliness, hygiene, and 100% safety, while our out-call services offer doorstep delivery for added ease.
We value your time and money, hence we kindly request pic collectors, time-passers, and bargain hunters to refrain from contacting us.
Our services feature various packages at competitive rates:
One shot: ₹2000/in-call, ₹5000/out-call
Two shots with one girl: ₹3500/in-call, ₹6000/out-call
Body to body massage with sex: ₹3000/in-call
Full night for one person: ₹7000/in-call, ₹10000/out-call
Full night for more than 1 person: Contact us at 🔝 9953056974 🔝. for details
Operating 24/7, we serve various locations in Delhi, including Green Park, Lajpat Nagar, Saket, and Hauz Khas near metro stations.
For premium call girl services in Delhi 🔝 9953056974 🔝. Thank you for considering us!Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X79953056974 Low Rate Call Girls In Saket, Delhi NCR
Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent High Profile Call Girl 24×7
Booking Contact Details
WhatsApp Chat: +91-9930245274
Mumbai Escort Service includes providing maximum physical satisfaction to their clients as well as engaging conversation that keeps your time enjoyable and entertaining. Plus they look fabulously elegant; making an impressionable.
Independent Escorts Mumbai understands the value of confidentiality and discretion - they will go the extra mile to meet your needs. Simply contact them via text messaging or through their online profiles; they'd be more than delighted to accommodate any request or arrange a romantic date or fun-filled night together.
We provide -
Flexibility
Choices and options
Lists of many beauty fantasies
Turn your dream into reality
Perfect companionship
Cheap and convenient
In-call and Out-call services
And many more.
29-04-24 (Smt)Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...

Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...Call Girls in Nagpur High Profile
Recently uploaded (20)
Russian Call Girls Service Jaipur {8445551418} ❤️PALLAVI VIP Jaipur Call Gir...

Russian Call Girls Service Jaipur {8445551418} ❤️PALLAVI VIP Jaipur Call Gir...
(Low Rate RASHMI ) Rate Of Call Girls Jaipur ❣ 8445551418 ❣ Elite Models & Ce...

(Low Rate RASHMI ) Rate Of Call Girls Jaipur ❣ 8445551418 ❣ Elite Models & Ce...
Mumbai ] (Call Girls) in Mumbai 10k @ I'm VIP Independent Escorts Girls 98333...![Mumbai ] (Call Girls) in Mumbai 10k @ I'm VIP Independent Escorts Girls 98333...](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
![Mumbai ] (Call Girls) in Mumbai 10k @ I'm VIP Independent Escorts Girls 98333...](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
Mumbai ] (Call Girls) in Mumbai 10k @ I'm VIP Independent Escorts Girls 98333...
Best Rate (Hyderabad) Call Girls Jahanuma ⟟ 8250192130 ⟟ High Class Call Girl...

Best Rate (Hyderabad) Call Girls Jahanuma ⟟ 8250192130 ⟟ High Class Call Girl...
Top Rated Bangalore Call Girls Mg Road ⟟ 9332606886 ⟟ Call Me For Genuine S...

Top Rated Bangalore Call Girls Mg Road ⟟ 9332606886 ⟟ Call Me For Genuine S...
Call Girls Coimbatore Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Coimbatore Just Call 9907093804 Top Class Call Girl Service Available
♛VVIP Hyderabad Call Girls Chintalkunta🖕7001035870🖕Riya Kappor Top Call Girl ...

♛VVIP Hyderabad Call Girls Chintalkunta🖕7001035870🖕Riya Kappor Top Call Girl ...
Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
![Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7](data:image/gif;base64,R0lGODlhAQABAIAAAAAAAP///yH5BAEAAAAALAAAAAABAAEAAAIBRAA7)
Call Girls in Gagan Vihar (delhi) call me [🔝 9953056974 🔝] escort service 24X7
Call Girls Faridabad Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Faridabad Just Call 9907093804 Top Class Call Girl Service Available
Call Girls Kochi Just Call 8250077686 Top Class Call Girl Service Available

Call Girls Kochi Just Call 8250077686 Top Class Call Girl Service Available
Top Rated Bangalore Call Girls Richmond Circle ⟟ 9332606886 ⟟ Call Me For Ge...

Top Rated Bangalore Call Girls Richmond Circle ⟟ 9332606886 ⟟ Call Me For Ge...
Call Girls Bareilly Just Call 8250077686 Top Class Call Girl Service Available

Call Girls Bareilly Just Call 8250077686 Top Class Call Girl Service Available
Call Girls Cuttack Just Call 9907093804 Top Class Call Girl Service Available

Call Girls Cuttack Just Call 9907093804 Top Class Call Girl Service Available
Call Girls Visakhapatnam Just Call 8250077686 Top Class Call Girl Service Ava...

Call Girls Visakhapatnam Just Call 8250077686 Top Class Call Girl Service Ava...
Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...

Book Paid Powai Call Girls Mumbai 𖠋 9930245274 𖠋Low Budget Full Independent H...
Call Girls Agra Just Call 8250077686 Top Class Call Girl Service Available

Call Girls Agra Just Call 8250077686 Top Class Call Girl Service Available
Call Girls Siliguri Just Call 8250077686 Top Class Call Girl Service Available

Call Girls Siliguri Just Call 8250077686 Top Class Call Girl Service Available
College Call Girls in Haridwar 9667172968 Short 4000 Night 10000 Best call gi...

College Call Girls in Haridwar 9667172968 Short 4000 Night 10000 Best call gi...
Call Girls Ooty Just Call 8250077686 Top Class Call Girl Service Available

Call Girls Ooty Just Call 8250077686 Top Class Call Girl Service Available
(👑VVIP ISHAAN ) Russian Call Girls Service Navi Mumbai🖕9920874524🖕Independent...

(👑VVIP ISHAAN ) Russian Call Girls Service Navi Mumbai🖕9920874524🖕Independent...
Ar medical conditions and dental care-dental toxicology
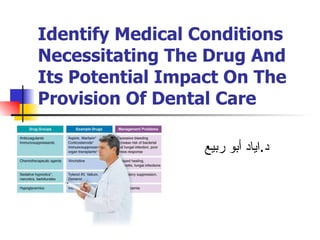
- 1. Identify Medical Conditions Necessitating The Drug And Its Potential Impact On The Provision Of Dental Care د . اياد أبو ربيع
- 5. Potential drug related oral health/management complications. Delayed healing, mucositis, fungal infections Vincristine Chemotherapeutic agents Increase risk of bacterial and fungal infection, poor stress response Corticosteroids* Immunosuppressants for organ transplants* Immunosuppressants Excessive bleeding Aspirin, Warfarin* Anticoagulants Management Problems Example Drugs Drug Groups
- 6. Potential drug related oral health/management complications. Delayed bone healing, bone necrosis Pamidronate (Aredia) Alendronate (Fosmax) Bisphosphonate bone stabilizers Hypoglycemia Insulin*, sulfonylureas Hypoglycemics Respiratory suppression, fall risk Tylenol, Valium, Demerol Sedative hypnotics*, narcotics, barbiturates Management Problems Example Drugs Drug Groups
- 8. Natural products that may alter dental management These herbs inhibit liver enzymes so they may potentiate the liver enzyme (cytochrome P450) inhibiting the effect of erythromycin and ketokonazole. Echinacea St. John’s Wort May increase bleeding Feverfew Garlic , Ginger Ginko Biloba Bilberry Dong Quai St. John’s Wort Possible Dentally Relevant Problem Compound
- 9. Natural products that may alter dental management May potentiate the effects of sedative Hypnotics and anti-anxiety drugs Valerian Hepatotoxicity, especially in those taking other medications metabolized in the liver. Sedative effects. Kava-Kava May increase blood pressure and heart rate due to anxiety or if epinephrine/vasoconstrictor used. Ephedra (Ma-Huang) Bitter orange Possible Dentally Relevant Problem Compound
- 19. Guidelines for compromised renal or hepatic function If greater than 4 times normal, do not use drugs that are toxic to or metabolized by the liver 30-40 u/l AST, ALT, liver transaminases Acetaminophen Codeine Diazepam Erythromycin Ibuprofen Ketoconazole Lidocaine Lorazepam Prednisone Hepatic One dose q 24 hrs One dose q 8-12 hours One dose q 8 hours <10 ml/min 10-50 ml/min >50 ml/min GFR (Creatinine Clearance) Amoxicillin Cephalosporin Penicillin Tetracycline Renal Margin of safety for dental prescribing Range Lab test Examples of dental drugs eliminated Potential impairment
- 24. Dealing with Patients of advanced age Renal Elimination Fluconazole Antifungal Amoxicillin Cephalosporin Tetracycline Antibiotic Drug Drug class
- 25. Dealing with Patients of advanced age Hepatic Elimination Diazepam Lorazepam Sedative/anxiolytic Lidocaine Local anesthetic Erythromycin Antibiotic Ibuprofen Pain reliever Drug Drug class
- 26. Dental Toxicology HEAVY METALS AND ANTIDOTES
- 27. HEAVY METALS AND ANTIDOTES
- 32. Lead Mechanisms of toxicity
