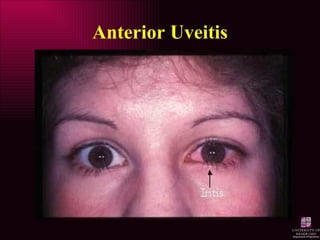
Anterior Uveitis
•Download as PPT, PDF•
138 likes•48,780 views
Report
Share
Report
Share
Recommended
More Related Content
What's hot (20)
ETIOLOGY, PATHOLOGY AND PATHOGENESIS OF CORNEAL ULCER

ETIOLOGY, PATHOLOGY AND PATHOGENESIS OF CORNEAL ULCER
Viewers also liked
Viewers also liked (13)
Similar to Anterior Uveitis
Similar to Anterior Uveitis (20)
Presentation 7- Mr Kim Son Lett- BMI RCGP Meeting 26-1-17.pptx

Presentation 7- Mr Kim Son Lett- BMI RCGP Meeting 26-1-17.pptx
More from Hossein Mirzaie
More from Hossein Mirzaie (20)
Mba monograph13 0412_marketinganoptometricpractice

Mba monograph13 0412_marketinganoptometricpractice
Spectacle prescription fulfillment in medical optometry cope approved

Spectacle prescription fulfillment in medical optometry cope approved
Recently uploaded
Recently uploaded (20)
call girls in munirka DELHI 🔝 >༒9540349809 🔝 genuine Escort Service 🔝✔️✔️

call girls in munirka DELHI 🔝 >༒9540349809 🔝 genuine Escort Service 🔝✔️✔️
Call Girls Jayanagar Just Call 7001305949 Top Class Call Girl Service Available

Call Girls Jayanagar Just Call 7001305949 Top Class Call Girl Service Available
Call Girls Hebbal Just Call 7001305949 Top Class Call Girl Service Available

Call Girls Hebbal Just Call 7001305949 Top Class Call Girl Service Available
Call Girl Koramangala | 7001305949 At Low Cost Cash Payment Booking

Call Girl Koramangala | 7001305949 At Low Cost Cash Payment Booking
Russian Call Girls Chickpet - 7001305949 Booking and charges genuine rate for...

Russian Call Girls Chickpet - 7001305949 Booking and charges genuine rate for...
VIP Call Girls Mumbai Arpita 9910780858 Independent Escort Service Mumbai

VIP Call Girls Mumbai Arpita 9910780858 Independent Escort Service Mumbai
Russian Call Girls in Pune Riya 9907093804 Short 1500 Night 6000 Best call gi...

Russian Call Girls in Pune Riya 9907093804 Short 1500 Night 6000 Best call gi...
Book Call Girls in Kasavanahalli - 7001305949 with real photos and phone numbers

Book Call Girls in Kasavanahalli - 7001305949 with real photos and phone numbers
call girls in green park DELHI 🔝 >༒9540349809 🔝 genuine Escort Service 🔝✔️✔️

call girls in green park DELHI 🔝 >༒9540349809 🔝 genuine Escort Service 🔝✔️✔️
Housewife Call Girls Hsr Layout - Call 7001305949 Rs-3500 with A/C Room Cash ...

Housewife Call Girls Hsr Layout - Call 7001305949 Rs-3500 with A/C Room Cash ...
College Call Girls Pune Mira 9907093804 Short 1500 Night 6000 Best call girls...

College Call Girls Pune Mira 9907093804 Short 1500 Night 6000 Best call girls...
Russian Call Girl Brookfield - 7001305949 Escorts Service 50% Off with Cash O...

Russian Call Girl Brookfield - 7001305949 Escorts Service 50% Off with Cash O...
Call Girls Frazer Town Just Call 7001305949 Top Class Call Girl Service Avail...

Call Girls Frazer Town Just Call 7001305949 Top Class Call Girl Service Avail...
Housewife Call Girls Bangalore - Call 7001305949 Rs-3500 with A/C Room Cash o...

Housewife Call Girls Bangalore - Call 7001305949 Rs-3500 with A/C Room Cash o...
Call Girls Hsr Layout Just Call 7001305949 Top Class Call Girl Service Available

Call Girls Hsr Layout Just Call 7001305949 Top Class Call Girl Service Available
Call Girls Service Nandiambakkam | 7001305949 At Low Cost Cash Payment Booking

Call Girls Service Nandiambakkam | 7001305949 At Low Cost Cash Payment Booking
Call Girls ITPL Just Call 7001305949 Top Class Call Girl Service Available

Call Girls ITPL Just Call 7001305949 Top Class Call Girl Service Available
Call Girls Whitefield Just Call 7001305949 Top Class Call Girl Service Available

Call Girls Whitefield Just Call 7001305949 Top Class Call Girl Service Available
VIP Call Girls Lucknow Nandini 7001305949 Independent Escort Service Lucknow

VIP Call Girls Lucknow Nandini 7001305949 Independent Escort Service Lucknow
Anterior Uveitis
- 11. Anterior Uveitis – Diagnostic Techniques & Signs Circumlimbal injection
- 12. Anterior Uveitis – Diagnostic Techniques & Signs Circumlimbal injection
- 13. Anterior Uveitis – Diagnostic Techniques & Signs Aqueous Flare
- 14. Anterior Uveitis – Diagnostic Techniques & Signs Cells in aqueous
- 15. Anterior Uveitis – Diagnostic Techniques & Signs 50+ cells in view Intense flare (coagulated aqueous, no circulation, fibrin visible) 4+ 20 to 50 cells in view Marked flare (iris and lens hazy) 3+ 10 to 20 cells in view Moderate flare (iris and lens still clear) 2+ 5 to 10 cells in view Faint flare (barely detectable) 1+ No cells Complete absence 0 Cells Flare Grade Grading of cells and flare
- 16. Anterior Uveitis – Diagnostic Techniques & Signs Keratic Precipitates
- 17. Anterior Uveitis – Diagnostic Techniques & Signs Hypopyon vs Hyphaema
- 18. Anterior Uveitis – Diagnostic Techniques & Signs Hypopyon vs Hyphaema
- 19. Anterior Uveitis – Diagnostic Techniques & Signs Band Keratopathy
- 20. Anterior Uveitis – Diagnostic Techniques & Signs Fibrin in aqueous
- 21. Anterior Uveitis – Diagnostic Techniques & Signs Fibrin in aqueous
- 22. Anterior Uveitis – Diagnostic Techniques & Signs Posterior Synechiae
- 27. Anterior Uveitis – Diagnostic Techniques & Signs Rubeosis Iridis
- 28. Anterior Uveitis – Diagnostic Techniques & Signs Mutton Fat Keratic Precipitates
- 29. Anterior Uveitis – Diagnostic Techniques & Signs Iris Nodules
- 30. Anterior Uveitis – Diagnostic Techniques & Signs Severe Acute Anterior Uveitis
- 31. Anterior Uveitis – Diagnostic Techniques & Signs Gonioscope view of Peripheral Anterior Synechiae (PAS)
- 36. Anterior Uveitis – Classification of Severity Moderate to severe symptoms VA <6/30 Deep circumcorneal flush KPs 3-4+ cells and flare Moderate to severe symptoms AV 6/9 to 6/30 Deep circumcorneal flush KPs 1-3+ cells and flare Mild to moderate Symptoms VA 6/6 to 6/9 Superficial circumcorneal flush No KPs 0-1+ cells and flare Severe Moderate Mild Clinical Degree of Anterior Uveitis
- 37. Anterior Uveitis – Classification of Severity Sluggish or fixed pupil Fibrous posterior synechiae Boggy iris (crypts) IOP increased Moderate to severe anterior vitreous cells Miotic, sluggish pupil Mild posterior synechiae Mild iris swelling IOP reduced 3-6 mmHg Anterior vitreous cells Normal pupil . No posterior synechiae No iris swelling IOP reduced <4mmHg Severe Moderate Mild Clinical Degree of Anterior Uveitis
