CNS Drugs and Their Mechanisms
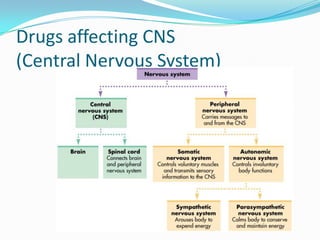
- 1. Drugs affecting CNS (Central Nervous System)
- 2. 1)General Anesthetics (block pain n conciousness before surgery) 2) Local Anesthetics (block pain n conciousness before surgery) 3) Sedative and Hypnotics ( induce calmness and sleep) 4) Opiod Analgesics (opium plant based analgesics) 5) Antitussive (prevent cough) 6) Antiparkinsonics (prevent rigidity of muscles ) 7) CNS stimulants (increase attentiveness) 8) Pshychotropic agents 8.1) Antipsychotics (manage schizophrenia and bipolar disorder ) 8.2) Anticonvulsants/ Antiepilepsy (prevent seizures) 8.3) Antidepressants (promotes good mood) 9) Anxiolytics/ Antianxiety (reduces anxiety/fear) What are the various drugs that target CNS and what they do?
- 3. Drugs causing CNS depression 1) General Anesthetics
- 4. Anesthesia – is a reversible condition of comfort, stillness and physiological stability in a patient before, during and after performance of a surgical procedure General anesthesia – required for to make the patient unaware / unresponsive to the painful stimuli in big surgical procedure e.g. heart, brain surgery. It effects entire body. Such drugs are called General Anesthetics eg cyclopropane, Ether, Nitrous oxide Local anesthesia - required for to make the patient unaware / unresponsive to the painful stimuli in small surgical procedure eg dental surgery. It effect is limited to the area of application. Such drugs are called Local Anaesthetics e.g. Procaine, Lidocaine and Bupivacaine etc. Anesthetics
- 5. 1)General Anesthetics General Characteristics 1) Analgesia (pain relief) 2) Impairment of all skeletal muscle (ie causes motionlessness and allow smooth surgury) 3) Loss of consciousness (needed to abolish fear and anxiety in patients during surgury) 4) Loss of motor reflexes 5) Reversible 6) Not therapeutic or diagnostic but facilitates surgery procedures
- 6. Side effects of Anesthetics May cause short term or long term Amnesia Nausea and vomiting after surgery Hypothermia (feeling very cold) Decreases respiration and heart beat (thus it requires monitoring during surgery)
- 7. Stages of GA and its Mechanism
- 8. Stages of GA Stage I: Analgesia Starts from beginning of anaesthetic inhalation and lasts upto the loss of consciousness Pain is progressively abolished during this stage Patient remains conscious, can hear and see, and feels a dream like state Reflexes, respiration and heart rate remain normal use is limited to short surgical procedures eg dental surgery
- 9. stages of GA – contd. Stage II: Delirium and Excitement: From loss of consciousness to beginning of regular respiration Excitement - patient may shout, struggle and hold his breath Muscle tone increases, jaws are tightly closed. Breathing is jerky; vomiting, involuntary micturition or defecation may occur. Heart rate and BP may rise and pupils dilate due to sympathetic stimulation. No stimulus or operative procedure carried out during this stage. This stage is not found with modern anaesthesia due to preanaesthetic medication, rapid induction to stage 3 etc.
- 10. stages of GA – contd. Stage III: Surgical anaesthesia Extends from onset of regular respiration to ending of spontaneous breathing. This has been divided into 4 planes: Plane 1: Roving eye balls. This plane ends when eyes become fixed. Plane 2: Loss of corneal and laryngeal reflexes. Plane 3: Pupil starts dilating and light reflex is lost. Plane 4: Intercostal paralysis, shallow abdominal respiration, dilated pupil.
- 11. stages of GA – contd. Stage IV: Medullary / respiratory paralysis breathing stops and failure of circulation which leads to death Pupils: widely dilated Muscles are totally flabby Pulse is imperceptible BP is very low.
- 12. Summary Stage 1: loss of pain Stage 2: loss of consciousness and excitement (we want to avoid this stage!) Stage 3: clam, stable patient. Surgery is done Stage 4: coma/death (we want to avoid this stage too!)
- 13. Mechanism of action 1) Non-specific/ Unified theory of anesthetics/ Meyer- overton theory eg all hydrocarbons (ether, cyclopropane) 2) Receptor specific action GABA gated Cl- channels Eg barbiturates, benzodiazepines and propofol Glycine gated channels eg Barbiturates, propofol NMDA (N – Methyl D- Aspartate) receptors eg Nitrous oxide and ketamine
- 14. Mechanism of action of GS Neurotransmission /synaptictransmission, is the process by which signaling molecules called neurotransmitters (NT) are released by a neuron (the Presynaptic neuron), and bind to and activate the receptors of another neuron (the postsynaptic neuron). Q) How do neurons communicate with each other? Ans. Through binding of neurotransmitters eg GABA, Glutamate with their receptors Physiology Review
- 15. Many CNS drugs work by influencing neurotransmitters release neurotransmitters receptor binding sites neurotransmitters reuptake Physiology Review
- 16. 1) Meyer-Overton Theory Meyer-Overton proposed a non-specific action of anesthetic drugs. They concluded: a) All lipid- soluble substances depress the CNS and act as anesthetic b) Increasing partition coefficient increases activity, regardless the structure c) The depressant activity occurs mostly in lipid rich cells
- 17. Meyer-Overton Theory cont Neurons transmit signal across each other when transmembrane receptor in post-synaptic neuron cell membrane bind neurotransmitters from pre-synaptic neuron Anesthetics show their effect due to great lipophilicity Thus they easily penetrate and dissolve in the phospholipid bilayer cell membranes of neurons This causes increase in volume of the membrane and alters shape of those transmembrane receptor so that they can’t bind with their ligands anymore. This prevents conductance of nerve signals thus effectively causes anesthesia
- 18. Receptor based action There are receptors present in the neuron cell membrane which are ligand gated ion channels such as glutamate gated Ca+ channels of NMDA receptors. GABA gated Cl- channels of GABAA receptor or When these ligand bind to their receptors, they allow ion entry into the cell. This can either allow propagation of stimulus in the nerves, as in Ca+ entry during NMDA opening due to glutamate binding. Glutamate is thus termed stimulatory neurotransmitter. inhibit propagation of stimulus in the nerves, as in Cl- entry during GABAA opening due to GABA. GABA is thus termed inhibitory neurotransmitter. Drugs show action through direct binding to these receptor in two ways. • They can inhibit the binding of glutamate to NMDA receptor and block its stimulating effect, which brings about CNS depressing effect • They can enhance binding of GABA to GABAA receptor and promote its inhibitory effect, which brings about CNS depressing effect
- 19. Preanesthetic medication: Definition: It is the term applied to the use of drugs prior to the administration of an anesthetic agent to make anesthesia safer and more agreeable to the patient.
- 20. Aim: Relief of anxiety and skeletal muscle relaxation Amnesia for pre and post operative events Supplement analgesic action so less anesthetic needed Decrease salivary and bronchial secretions to prevent any reflex coughing Antiemetic effects Decrease acidity and volume of gastric juice
- 21. Preanaesthetic medication – contd. Drugs used: Benzodiazepams - diazepam or lorazepam, midazolam, promethazine (abolish fear and relax skeletal muscle) Profolol (cause amnesia in addition to anesthesia) Opioids – Morphine and its derivatives (analgesic supplement) Anticholinergics – Atropine (inhibit saliva, bronchial secretion) H2 blockers – ranitidine, famotidine (inhibit gastric acid) Proton pump inhibitors- Omeprazole (inhibit gastric acid) Antiemetics – Metoclopramide, domperidone (inhibit vomitting)
- 22. Current Intravenous reversal agents In some cases drugs are needed to antagonize anesthetic medication so that patients can be brought back to consciousness after surgury Naloxone (reverse opioids), Physostigmine (reversal of various sedatives), Flumazenil (reversal of benzodiazepine) Naloxone is very useful and specific for reversing adverse and life- threatening respiratory depression caused by narcotic drugs antagonizing opiod receptors. Physostigmime is used for reversing sedative effects in patients who are depressed after having received benzodiazepines, droperidol, scopolamine, opioids, and phenothiazines which prevent metabolic degradation of acetylcholine and start the parasympathetic NS Flumazenil reverses the sedative, respiratory depressant, anxiolytic, muscle relaxant, anticonvulsant, amnestic, and anesthetic effects of only benzodiazepine by antagonizing the GABA receptors
- 23. Classification of GAInhalation: 1. Gas: Nitrous Oxide* 2.Volatile liquids: Halothane* Enflurane Isoflurane Desflurane Sevoflurane Intravenous: 1. Ultrashort acting Barbiturates Thiopental sodium*, Thiamylal 2. Benzodiazepines Midazolam 3. Dissociative anesthesia: Ketamine 4. Narcotic : fentanyl 5. Micellneous Propofol and Etomidate
- 24. Nitrous oxide/laughing gas (N2O) Colorless, odorless inorganic gas with sweet taste Noninflammable and nonirritating Very potent analgesic but weak anesthetic Used wit O2 in dental extraction and in obstetrics Stored in metal cylinders
- 25. Mechanism Of Action (MOA) They antagonize NMDA receptors. This prevents NMDA from binding to this receptor which prevents entry of Ca2+ ion and propagation of action potential. Thus they block signal transmission between neurons NH4NO3 N2O + 2H2O 170 o C Synthesis:
- 26. Advantages: - Non-inflammable and nonirritant - Rapid induction and recovery - Very potent analgesic (low concentration) - No nausea and vomiting - Nontoxic to liver, kidney and brain - doesn’t depress respiration Disadvantages: Not potent anasthetic alone (needs supplementation) If given in high conc., it causes Hypoxia Inhibits methionine synthetase (precursor to DNA synthesis) Inhibits vitamin B-12 metabolism NH4NO3 N2O + 2H2O 170 o C Synthesis:
- 27. Inhalation/Volatile liquids These are organic compounds that are held by weak intermolecular forces and hence can transform from liquids to gas state spontaneously. They are administered in gas phase by especial equipment called vaporizer which balance oxygen amount along with the inhalation Types: Class Examples Hydrocarbon Cyclopropane, Ethylene (2HC=CH2) Halogenated hydrocarbon Halothane, Ethyl Chloride (C2H5Cl) Ether Diethyl Ether (C2H5-O-C2H5) Vinyl Ether (CH2=CH-O- CH=CH2) Alcohol Trichloroethanol (CCl3CH2OH)
- 28. Anesthetic Vaporizer: A machine that delivers volatile anesthetic in the right dose while maintaining oxygen intake too
- 29. Ideal properties of volatile anesthetics They should not be flammable cause irritation to epithelial cells cause any physiological response They should have wide margin of safety Quick action Quick recovery Easy to administer Good stability in metal containers Cheap and easy to manufacture
- 31. Halothane Fluorinated volatile liquid with sweet odour, non- irritant non-inflammable and supplied in amber coloured bottle Potent anaesthetic, requires only 2-4% for induction and 0.5-1% for maintenance Boiling point : 50ºC Pharmacokinetics: 60 to 80% eliminated unchanged. 20% retained in body for 24 hours and metabolized Cl ClCl HF (hydrogen fluride), 130o C SbCl3 (antimony trichloride), F ClF F Br2, 450o C F ClF F Br Trichloroethylene 2-Chloro-1,1,1 -trifluoro-ethane Haloethane Synthesis of Haloethane
- 32. Halothane – contd. Advantages: - Non-inflammable and non-irritant - Pharyngeal and laryngeal reflexes – bronchodilatation - Potent and speedy induction & recovery - Controlled hypotension - Inhibits intestinal and uterine contractions Disadvantages: - Special apparatus - Poor analgesic and muscle relaxation - Respiratory depression - Decreased urine formation – due to decreased GFR - Causes Hepatitis: 1 in 10,000 - Malignant hyperthermia - Prolong labour
- 33. Enflurane: Non-inflammable, with mild sweet odour and boils at 57ºC Similar to halothane in action, except better muscular relaxation Depresses myocardial force of contraction Induces seizure in deep anaesthesia and therefore not used now Metabolism is only one-tenth that of halothane ie does not release high quantity of hepatotoxic metabolites But metabolism releases fluoride ion which causes renal toxicity
- 34. Isoflurane: Isomer of enflurane and have simmilar properties but slightly more potent and Induction dose is 1.5 – 3% and maintenance dose is 1 – 2% Needs specialized vapourizer to deliver the patient
- 35. Isoflurane – contd. Advantages: - Rapid induction and recovery - Good muscle relaxation - Good coronary vasodilatation - No renal or hepatotoxicity - Low nausea and vomiting - No seizure and preferred in neurosurgery - Uterine muscle relaxation Disadvantages: - Special apparatus - Pungent and respiratory irritant - Special apparatus required - Respiratory depression - Maintenance only, no induction - ß adrenergic receptor stimulation - Costly
- 36. Desflurane A popular and safe,potent anesthetic It has pungent smell, thus first IV anesthetic is used for induction and this is used for maintenance Boiling point is 27 degree (very low) Only 0.02% is metabolized, rest expelled unchanged through lungs Induction dose is 3% and maintenance is 2.5% with or without nitrous oxide
- 37. Advantages - Non- inflammable - Non-corrosive to metal - Rapid induction and rapid recovery - No hetatotoxicity and Nephrotoxicity Disadvantages - Pungent smell - Special vaporizer needed since BP is so low there is chance of more drug delivery as room temperature fluctuates
- 38. Sevoflurane Potent anesthetic BP about 58.6 degree About 3% is metabolized, metabolism produces Fluoride ion F ion can cause nephrotoxicity but this effect is negligible Dose : 1.4-2.6% alone or 0.7-1.4% with nitrous oxide
- 39. Advantage - Non flammability - Non-irritating - Rapid induction and rapid recovery - Nephrotoxicity is negligible Disadvantage - Higher metabolism than desflurane - Rxn with sodalime forms toxic compound
- 40. “Rxn with sodalime forms toxic compound”. Explanation: The vaporizer machine that delivers the volatile anesthetic has soda lime (mixture of Ca(OH)2,NaOH,KOH and water) which is basic in nature Its purpose is to react with the exhaled CO2 to form water soluble salts CO2 This removes exhaled CO2 , which if not done, then it will be inhaled again and CO2 toxicity can occur
- 41. Some terminology defined. Maintaining Anesthetic : Volatile anesthetics that are potent and sustain stage 3 anesthesia long enough to complete surgery Inducing Anesthetic : IV Anesthetics that act rapidly enough to bypass the 2nd stage of anesthesia which is needed to prevent choking danger on saliva or vomit Minimum Alveolar Concentration : It is defined as the concentration at 1 atm of anesthetic in the alveoli that is required to produce immobility in 50% of adult patients subjected to a surgical incision
- 42. Intravenous Delivered by IV injection. Time taken is extremely fast. It causes anesthesia with 1 min. Ketamine Profolol Etomidate Barbiturates (thiopental sodium, thiamylal) & Benzodiazepam (Midazolam) (lectured in Sedative and hypnotics) Fentanyl (to be lectured in opiod analgesics)
- 43. Ketamine inject able and very potent, rapid acting agent Duration of action about 10-25 min Advantage: Do not relax skeletal muscle and thus used in dental surgery Disadvantage: After recovery patient is in state of confusion Disturbing dreams and hallucinations up to 24 hrs post recovery This long duration action is explained by its metabolic product norketamine which inhibits NMDA receptors and is itself a weak anesthetic 96% is metabolized in this way
- 44. MOA: They antagonize NMDA receptors. This prevents binding of glutamate/aspartate to this receptor. Glutamate is the main stimulatory neurotransmitter in CNS. The lack of any stimulation, causes the CNS to falls into depression. Dissociative effect of ketamine Ketamine makes patient appear to be awake but his eyes keep moving here and there and they aren’t aware of their environment. The drug disconnects limbic system from the thalamocortical system. This neural connection is required to feel consciousness. Thus patient is alive and well but is not aware about it!
- 45. Propofol Has amnesic property and formulated as a white emulsion. Thus named “milk of amnesia” MOA: It enhances effect of inhibitory neurotransmitter, GABA at the GABAA receptors and thus promotes CNS depression Advantage : Propofol has a fast onset of action and crosses the blood- brain barrier very quickly. Thus it is a very good inducing anesthesia. Its short duration of action is due to rapid distribution from the CNS to other tissues. No vomiting after surgury Disadvantage: It has narrow window of safety. High dose can create cardio-respiratory depression and death. There is no reversal medication for propofol toxicity. Thus overdose can be lethal. The ampoule containing it must be discarded after single use to avoid risk of sterility breakage Dose: 2-2.5 mg/kg produces hypnosis in 1 min lasting upto 5 min
- 46. Etomidate Potent, rapidly acting but short time only (less than 3 min) hypnotic agent with no analgesic activity The anaesthetic induction dose for adult humans is 0.3 mg/kg intravenously, with a typical dose ranging from 20–40 mg MOA: It enhances effect of inhibitory neurotransmitter, GABA at the GABAA receptors and thus promotes CNS depression Advantage: Useful for induction of anesthesia in patients susceptible to hypotension because of coronary artery disease Disadvantage: Known to inhibit adrenal steroid hormone synthesis eg aldosterone, testosterone, estrogen etc
- 47. Thank you Drug discovery Process Time taken : 10 years to 15 years Cost : 5 billion $ as of 2013 Proper study of a disease physiology/pharmacology is the key to success There is no cure for type 1 diabetes cause we don’t know what enzyme or receptor to stimulate or inhibit that will cause insulin secretion
- 48. Revision Anesthetics are drugs that allow painless, fearless and risk free surgery by depressing signal transfer between nuerons They are not a cure to any disease or manage any disease symptoms Two types General Anesthetic- act on full body Local Anesthetic – only area of application
- 49. Summary Stage 1: loss of pain Stage 2: loss of consciousness and excitement (we want to avoid this stage!) Stage 3: clam, stable patient. Surgery is done Stage 4: coma/death (we want to avoid this stage too!)
- 50. Stages of anesthesia Match the following Stage 1 Stage2 Stage 3 Stage 4 1. Calm, stable patient 2. Excited patient 3. Need maintenance 4. Respiratory failure 5. No pain 6. Surgical stage 7. No consciousness 8. Risk of choking on vomit and saliva 9. Death
- 51. Mechanism :Meyer-overturn Theory •It is a Non-specific mechanism i.e. drug don’t bind to any receptors but enters lipid cell membrane and dissolves in it •This causes membrane expansion which alters receptor shape. NT can’t bind with this altered receptors
- 53. How shape of lock/receptor is influenced by just the lipophilicity of drug?
- 54. The lipid layer surrounding the transmembrane protein have role in maintaining it’s shape. Both tightening or loosening of the lipid membrane alters shape of protein. Expansion of the lipid layers as a result of dissolving of anesthetic drugs squeezes the protein and alters it’s shape. In this altered shape it can’t bind with it’s substrate
- 55. Mechanism :Meyer-overturn Theory •Why do inhaled anesthetics enter lipid cell membranes and not just stay in the blood? Becoz they have high lipid solubility and high partition coefficient •What happens when anesthetics enter lipid membranes? They remain there and dissolve into the lipid membranes , thus increasing its volume •What is the result of this increase in volume of membrane? It alters receptor shape and binding site •What happens if shape of receptor is altered? Neurotransmiters can’t bind to this altered receptor’s binding site •What happens if NT can’t bind to their receptor? Nuerotransmission between adjacent neurons is stopped. CNS gets depressed. Person falls into anesthetic stage.
- 56. Current reversing agents Naloxone (reverse opioids), Physostigmine (reversal of many sedatives), Flumazenil (reversal of only benzodiazepine) Preanesthetic medication Which are not an objective of Preanesthetic medication? - Remove fear/anxiety after surgery - Cause memory loss of events before surgery - Stop urination and defecation during surgery - Stop salivary secretions/ vomiting/gastric acid - Supplement analgeisc - Relax smooth muscles Function of Current reversing agents - Recovery of patients who are extra sensitive to GA - Counter overdosing of Sedatives/narcotics
- 57. Inhalation anesthetics : N2O, Halothane, Enflurane, Isoflurane, Desflurane, Sevof lurane The only truly gas Anesthetic is ______ The only volatile Anesthetic containing Br is _______ The halogen not included in volatile Anesthetic is ____ Which volatile Anesthetic causes seizures during anesthesia? _______ Halogen that causes nephrotoxicity is _______ The weakest anesthetic is ____ Enflurane and isoflurane are ________ of each other -Diesteriomer - Conformational isomer -Geometric isomer - Enantiomer
- 59. •Why N2O gas can’t be given alone? a) It is not a potent anesthetic. It requires high dosing to produce stage 3 anesthesia. b) If given in such high does, it will reduce O2 intake causing hypoxia (Hypoxia means lack of O2 in the air we inhale) •How is N2O stored and delivered to patient? N2O is stored in pressurized metal gas containers. It is diluted with oxygen and delivered in gas phase by simple diffusion process •What are induction anesthesia? They are IV anesthetics that rapidly and smoothly bring stage 3 anesthetic stage by avoiding the complications of stage 2 (such as vomiting, shouting, saliva secretion, irregular breathing, micturation, defeacation, tight muscles )
- 60. • Why volatile anesthetics require a vaporizer machine? They are stored in liquid containers but need to heated to convert to vapour and then diluted with oxygen gas properly to allow inhalation to patient in right dose throughout the entire surgery period • Why desflurane requires special vaporizer for delivery? It has very low boiling point of 27oC. Slight increase in room temp can increase amount of gas inhaled. Thus careful delivery needs to be done to avoid overdosing as a result of variation in room temperature . •Why do vaporizer machine contain soda lime? To absorb and neutralize the CO2 exhaled by the patient in a simple acid base rxn so as to avoid inhalation of CO2
- 61. Which is false about volatile anesthetics? Nitrogen is a volatile anesthetic The main route of elimination is by lungs They are largely metabolized by liver They have rapid action and recovery They are non-inflamable and non-irritant They require especial equipment to deliver They are stored and used in gas form Enflurane is not used anymore because it is not potent
- 62. Intravenous anesthetics Ketamine, Propofol, Etomidate Called inducing anesthetics: Used to cause rapid anesthesia from stage 1 to stage 3 Shows analgesic action within 1 min but lasts for short duration only (10-25 min, 5 min, 3 min) Major elimination is through liver and kidney not lungs Ketamine Inhibits glutamate at NMDA receptor Profolol Enhances effect of GABA at GABAa receptor Etodimate Enhances effect of GABA at GABAa receptor
- 63. How ketamine causes bad dreams for upto 24 hrs post recovery? It gets metabolized into norketamine, which also has mild CNS depressing effect Etomidate has no analgesic ability ie can’t take away pain. How can it be used an GA? It is used because it has good inducing property. The lack of analgesic activity can be compensated from preanesthetic medicines. Plus it does not lower BP and has special advantage in Coronary artery disease Why is propofol made into an emulsion? Because It has poor water/blood solubility
- 66. Two types of reflex action a) Jerking of knee when hit by a hammer b) Drawing hand away from fire when feeling burnt
- 67. How agonist differes from antagonist?
- 68. How allosteric drugs differ in their Mechanism from agonist or antagonist?
Editor's Notes
- GABA and glycine for chlorine, NMDA for Ca,
- Malignant hyperthermia (MH) is a pharmacogenetichypermetabolic state of skeletal muscle induced in susceptible individuals
- limbic system controls emotions, motivationthalamocortical system controls consiouness
- StageI - option 5, StageII - option 2,7 and 8, StageIII - option 1,3 and 6, StageIV – option 4 and 9
- 1,3,5 are wrong answer
- Answers: N2O, halothane, Iodine, Enflurane, Flourine, N2O, Etomidate, geometrical isomer,
- N02
- F,T,F,T,T,T,F,F
