Histology of oral mucous membrane and gingiva
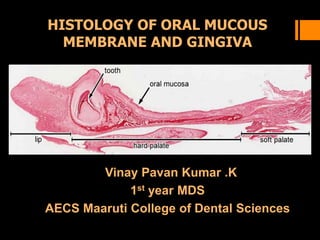
- 1. HISTOLOGY OF ORAL MUCOUS MEMBRANE AND GINGIVA Vinay Pavan Kumar .K 1st year MDS AECS Maaruti College of Dental Sciences
- 2. HISTOLOGY OF ORAL MUCOUS MEMBRANE AND GINGIVA Definition Functions Classification Structure Organization Histology of gingiva Prosthetic consideration Biological width
- 3. The oral cavity is in many respects a very interesting part of the human body . Many different kind of tissue from the hardest teeth to the softest, the salivary glands are found therein. The oral cavity is lined with an uninterrupted mucosa which is continuous with the skin near vermillion border of the lips and with the pharyngeal mucosa in the region of soft palate INTRODUCTION
- 4. Functions of oral mucosa Protection : Barrier for mechanical trauma and microbiological insults Sensation : Temperature (heat and cold), touch, pain, Reflexes such as swallowing, gagging and salivation Absorption : Nitrates are absorbed sublingually
- 5. Secretion: Salivary secretion creates a moist oral cavity helps in speech, swallowing, mastication and in the perception of taste. Thermal regulation: Important in dogs not in humans Excretion: excretion of certain metabolites Esthetics : Lips and gingiva enhance facial esthetics
- 6. Classification of oral mucosa Based upon primary function served 1. Masticatory Mucosa (25%) 2. Lining Mucosa (Covers 60% of total area) 3. Specialised Mucosa (15%) Based upon keratinisation 1. Keratinised Orthokeratinized Parakeratinized 2. Non-keratinised.
- 7. Based upon Location 1. Buccal Mucosa. 2. Lingual Mucosa. 3. Palatal Mucosa. 4. Labial Mucosa. 5. Alveolar Mucosa.
- 8. Structure of Oral Mucosa Epithelium Lamina Propria. Submucosa
- 9. Epithelium Epithelium of the oral mucosa is stratified squamous epithelium. It may be 1.Keratinized 2.Non keratinized Keratinized layer ortho keratinized Para keratinized
- 10. Oral epithelium Consists of two populations of cells: Progenitor population Maturing population Progenitor cells function is to divide and provide new cells Maturing cells continually undergo a process of differentiation or maturation to form a protective layer
- 11. Amplifying CellsStem cells Progenitor Cells • Slow dividing • Maintain basal cell layer • Rapidly dividing • Form other cell layers.
- 12. Turn over time Skin : 52 – 75 days Gut : 4 – 14 days Gingiva : 41 – 57 days Cheek : 25 days Junctional Epithelium : 5 - 6 days The time taken for a proginetor cell to pass through the entire epithelial thickness and reach the surface
- 13. Keratinized oral mucous membrane
- 16. Basal layer made of cell that synthesize DNA & undergo mitosis. Stratum Basale Basal cells show ribosomes & elements of rough endoplasmic reticulum indicative of protein synthesizing activity.
- 17. Structureless zone seen under light microscope is basement membrane. 1 – 4 microns wide. Under electron microscope, Basal lamina lamina lucida – light zone lamina densa – dark zone
- 18. Basal cells are attached to basal lamina by hemidesmosomes. Epithelial cell-cell contact is made through desmosomes - macula adherens. These are anchored intracellularly by tonofibrils.
- 19. i) Serrated- heavily packed with tonofilaments which are adaptations for attachment. ii) Non-serrated – stem cells – slowly dividing cells which serve to protect genetic information of the tissue.
- 20. Stratum spinosum or prickle cell layer: It is a layer of relatively large irregular polyhedral cells. Show first sign of maturation. Nuclei stains less intense the intercellular spaces of the prickle layer are large and distended, with more prominent desmosomes
- 21. Stratum granulosum Flatter & wider & nuclei show signs of degeneration & pyknosis.
- 22. Active in protein synthesis. Involucrin - soluble precursor protein of the cornified envelope appears first in the spinosum. Protein synthesis rate progressively gets diminished as cell approaches stratum corneum. In the upper part cells of stratum granulosum, shows granules called ODLAND BODIES.
- 23. Keratinosome or odland bodies or membrane containing granules Modified lysosomes 0.25µm in length. Rich in phospholipids. Structure - layers of parallel lamellae, probably originating from golgi apparatus. Lamellar granules discharge their contents - permeability barrier.
- 24. Stratum corneum Made up of keratinised squamae, which are larger & flatter than the granular cells. Nuclei & other organelles disappear.
- 25. Cell surfaces in this layer are more regular & more closely adapted to adjacent cell surfaces. The filaggrin a non fibrous inter-filamentous matrix protien helps in this close adaptation.
- 26. Types of keratinized epithelium Parakeratinized Epithelium :The superficial cells are dead but retain the nucleus Orthokeratinized Epithelium : The nuclei are lost in epithelium
- 28. Non – keratinized epithelium Nonkeratinized epithelial cells in the superfacial layers do not have keratin filaments in the cytoplasm The surface cells also have nuclei This epithelium is associated with lining of the oral cavity
- 29. Difference Keratinized Layers - basal, spinosum, granular, cornified layer. Produce a cornified surface layer. Prickly appearance. Nonkeratinized Layers-basal,intermediate, surface layer. Do not produce a cornified surface layer. Intercellular spaces not obvious-no prickly appearance.
- 30. No nuclei-orthokeratinised Pyknotic nuclei- parakeratinised Filaggrin present. Numerous tonofilaments,keratohyaline granules present. Lack filaggrin,but contain involucrin. Less developed and dispersed tonofilments,lack keratohyaline granules. Stratum superficiale contains nucleated cells
- 31. Lamina Propria Two Layers Papillary layer Close to epithelial ridges. Arranged loosely. Reticular layer Parallel to epithelium. Fibers are very thick. Consists of cells , blood vessels, neural elements & fibers embedded in amorphous ground substance.
- 32. Cells found in lamina propria Fibroblast Histiocytes Macrophages Mast cell Polymorph nuclear leucocytes Lymphocytes Plasma cells Endothelial cells
- 33. Submucosa It attaches the mucous membrane to the underlying structures – muscle or bone loose or a firm attachment and consists of glands, blood vessels, nerves, & adipose tissues. connective tissue of various thickness
- 34. Nonkeratinocytes Langerhan’s cells:Dendritic cells. Merkel cell: touch receptors Melanocytes: melanin systhesis Inflammatory cells
- 35. Organization of the Oral Mucosa 3 types according to function: Masticatory Mucosa:25% of total mucosa. Lining Mucosa:60% of total mucosa Specialized Mucosa:15% of total mucosa.
- 36. Lining mucosa Covers the floor of mouth, ventral (underside) tongue, alveolar mucosa, cheeks, lips and soft palate. Lip Lip is covered by lining mucosa
- 37. Vermilion border Junction between the skin and mucous membrane of the lip
- 38. Floor of the mouth Loosely attached to the underlying structures Submucosa – adipose tissue
- 39. Ventral surface of the tongue The mucous membrane is tightly bound to the muscle bundles of the tongue smooth and relatively thin
- 40. Cheek Submucosa contains fat cells and small mixed salivary glands
- 41. Mucosa of the Tongue - Specialised mucosa Anatomical division It is divided into two parts by a V-shaped groove known as sulcus terminalis. Anterior 2/3rd or papillary portion or body of the tongue contains lingual papillae. Posterior 1/3rd is lymphatic portion or base of the tongue contains lingual tonsil.
- 42. The different papillae found on the dorsal surface of the tongue are: 1. Filliform papillae 2. Fungiform papillae 3. Circumvallate papillae 4. Foliate papillae
- 43. 1. Filliform papillae Pointed extensions of the keratinized epithelial cells Most numerous papillae of the tongue Not associated with taste buds Scanning electron micrograph of Filliform papillae(arrow)
- 44. 2. Fungiform papillae Fewer than the filliform papillae and are scattered over the dorsal surface of the tongue Rounded elevations above the surface of the tongue Have taste buds on their superior surfaces Not keratinized
- 46. 3. Circumvallate papillae Located at the junction of the anterior two thirds (body) and posterior one thirds (base) of the tongue There are eight to twelve in number Lined with taste buds and also openings of serous glands The secretion from the serous glands washes away food for renewal of taste
- 48. 4. Foliate papillae Located in the furrows along the posterior sides of the tongue Lined with taste buds Not prominent in human beings
- 49. Taste Buds They are small ovoid barrel shaped organs 40 micron thick and 80 micron high Their outer surface is covered by flat cells which surround a small opening called the Taste Pore
- 50. Areolar mucosa The areolar mucosa is a reddish-pink tissue with blue vascular areas. The epithelium is extremely thin non- keratinized mucosa with a lamina propria
- 51. Hard Palate Covered by masticatory mucosa lateral regions of the posterior part contains palatine glands
- 52. Gingiva Covers the alveolar process of jaws and surrounds the cervical portion of teeth. It develops from the union of oral epithelium and reduced enamel epithelium Gingiva can be classified as Free gingiva, Attached gingiva and Interdental papilla
- 53. Part of the oral mucosa that surrounds the necks of the teeth and forms the free margin of the gingival tissue differentiated apically by the free gingival groove Free gingiva (marginal gingiva)
- 54. Attached gingiva Between the free gingival groove and the alveolar mucosa The junction of the attached gingiva and the alveolar mucosa is called mucogingival junction In healthy mouth attached gingiva shows stippling
- 55. Interdental papilla Appear in-between teeth apical to the contact points Valley like depression in the interdental papilla called Col.
- 56. Gingival sulcus Space or potential space between the tooth surface and the free gingiva. It is lined with sulcular epithelium Extends from free gingival margin to the junctional epithelium.
- 57. Junctional epithelium Forms the seal of the gingival epithelium and the tooth Floor of the gingival sulcus and extends apically to the enamel of the tooth Disturbances of epithelial attachment results in deepening of the sulcus which is a sign of gingival/periodontal disease
- 58. Sulcular epithelium It is nonkeratinized. No rete pegs in sulcular epithelium. Sulcular epithelium is continuous With gingival epithelium & the attachment epithelium
- 59. Gingiva contains dense fibers of collagen: Dentogingival : extends from the cervical cementum into the lamina propria of the gingiva. Circular: small group of fibers that circle the tooth & interlace with other fibers.
- 60. Dentoperiosteal: fibers can be followed from the cementum into periosteum of the alveolar crest & of the buccal & palatal or lingual surface of the alveolar bone. Alveologingival: fibers arise from the alveolar crest & extends into lamina propria.
- 61. Biologic Width
- 62. Biologic width The dimension of space that the healthy gingival tissues occupy above the alveolar bone is the biologic width. Connective Tissue attachment + junctional epithelium constitutes Biologic width 1.07mm +0.97mm= 2.04 mm Any restoration should be atleast 3mm above the alveolar crest to prevent the violation of the biologic width.
- 63. Passive Eruption
- 64. Effect Of Aging On The Oral Mucosa Epithelial thinning Decreased keratinization Less prominent rete pegs Decreased cellular proliferation Loss of submucosal elastin and fat Increased fibrotic connective tissue with degenerative alteration in the collagen.
- 66. Behaviour of oral mucosa under stress Under compression behaves in a viscoelastic fashion. Loaded epithelium demonstrates decrease in the depth of epithelial ridges & connective tissue papillae Care to be taken during impression procedures by applying minimal pressures.
- 67. Tissue response A. Recently made dentures: Inflammation . Soft tissue distortion. Impingement of gingival margin. Accumulation of dental plaque. B. Dentures in use for > 1 year Hyperkeratosis. Scarring of tissue in border area. Gross tissue distortion.
- 68. Soft tissue changes in oral mucosa due to prostheses soft tissue hyperplasia fibrous hyperplasia. epulis fissurata. papillary hyperplasia. inflammatory process under denture bases denture stomatitis. Candidiasis. ulcerative lesions angular chelitis.
- 69. Soft tissue hyperplasia Rolls of hyperplastic tissues under denture base Due to bone resorption, with lesion filling the space under denture base. Develops slowly, painless. Surgical removal. New dentures.
- 70. Papillary hyperplasia Granular type of inflammation seen in palatal region. Numerous papillary projections give a warty appearance. They show precancerous tendencies. Discontinue denture wearing. Surgery. New dentures
- 71. Epulis Fissuratum It is a pathologic condition that appears in the mouth as an overgrowth of fibrous connective tissue. Also known as inflammatory fibrous hyperplasia, denture epulis and denture induced fibrous hyperplasia. It is mainly caused due to ill fitting dentures
- 72. Denture stomatitis Chronic inflammation Ill fitting denture. Nocturnal denture wearing. Hypersensitivity. Poor oral hygiene. Infections –Candida albicans.
- 73. Candidiasis Debilitated patients. Systemic disease such as diabetes. Unhygienic conditions. - Discard the existing denture. - Anti fungal therapy - New dentures.
- 74. Angular chelitis SIGNS Bilateral lesion that develops at the angle of the lips. Deep fissure or crack may be seen. Appear ulcerated. Exudatve crust may be present. Anti fungal therapy.
- 75. Denture bearing area Points to be considered while fabrication of denture: Selective placement of forces by denture base on supporting tissues. Form and placement of denture borders to accommodate normal function.
- 76. Selective placement of force can be achieved by employing different impression techniques depending on the patients oral condition Minimal pressure technique/Mucostatic technique . Selective pressure technique. Pressure / Muco-compressive technique.
- 77. Crest of the residual ridge (maxillary) Firmly attached to the bone. Keratinized epithelium. Dense collagen fibers . Sub mucosa – fat or glandular cells. Primary support for denture.
- 78. Palatine rugae Irregularly shaped rolls of soft tissue in the anterior part of hard palate. Clinical considerations Secondary stress bearing area. Resists forward movement of denture. Tissue rebound phenomenon. Maxillary major connector should end into depressions between the rugae.
- 79. Mucous membrane of hamular notch Space between the posterior part of the maxillary tuberosity & pterygoid hamulus. It is thick and made of loose areolar tissue. Marks the distal end of denture.
- 80. Buccal shelf area Partially keratinized. Loosely attached. Bone – compact bone. Clinical implication Impression should cover the entire available area.
- 81. Slope of the residual ridge (mandibular) Keratinized epithelium . When the soft tissue is movable in the crest of the ridge ,impression should be recorded in its resting position.
- 82. F.P.D & oral mucosa Sub gingival finish esthetics. old restoration extending into the intracrevicular space. Insufficient vertical length or height Margins should be smooth with proper fit.
- 83. Esthetics & oral mucosa Case of Altered passive eruption(APE)
- 84. Implants and Biological width It has been found that the biological width need not be a vertical dimension but can have a horizontal component. Platform switching provides this horizontal distance and so preserves the crestal bone.
- 85. CONCLUSION
- 86. References Ten Cate A R, Oral histology development,structure and function, 5th edition, India, Mosby, 1999, pp 345- 385. Kumar G S, Orban’s oral histology and embryology, 12th edition,India, Elsevier,2006, pp 210-257 Zarb G.A, Bolender C L, Prosthodontic treatment for edentulous patients, 12th edition, India, Elsevier, 2004, pp 84-86, 211-223,233-241 Avery J K, Oral development and histology, 3rd edition, New York, Thieme, 2002, pp 243-252.
