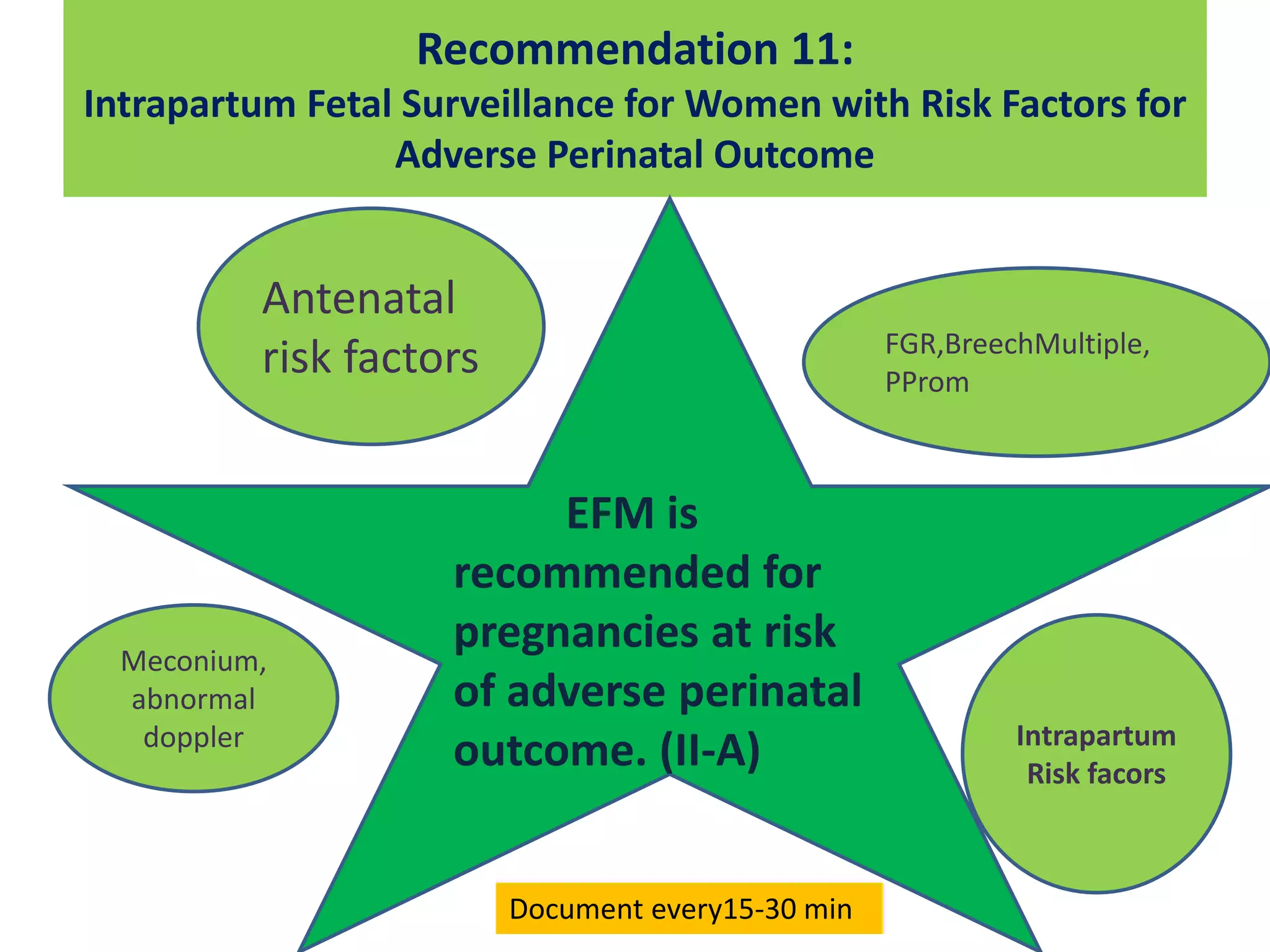
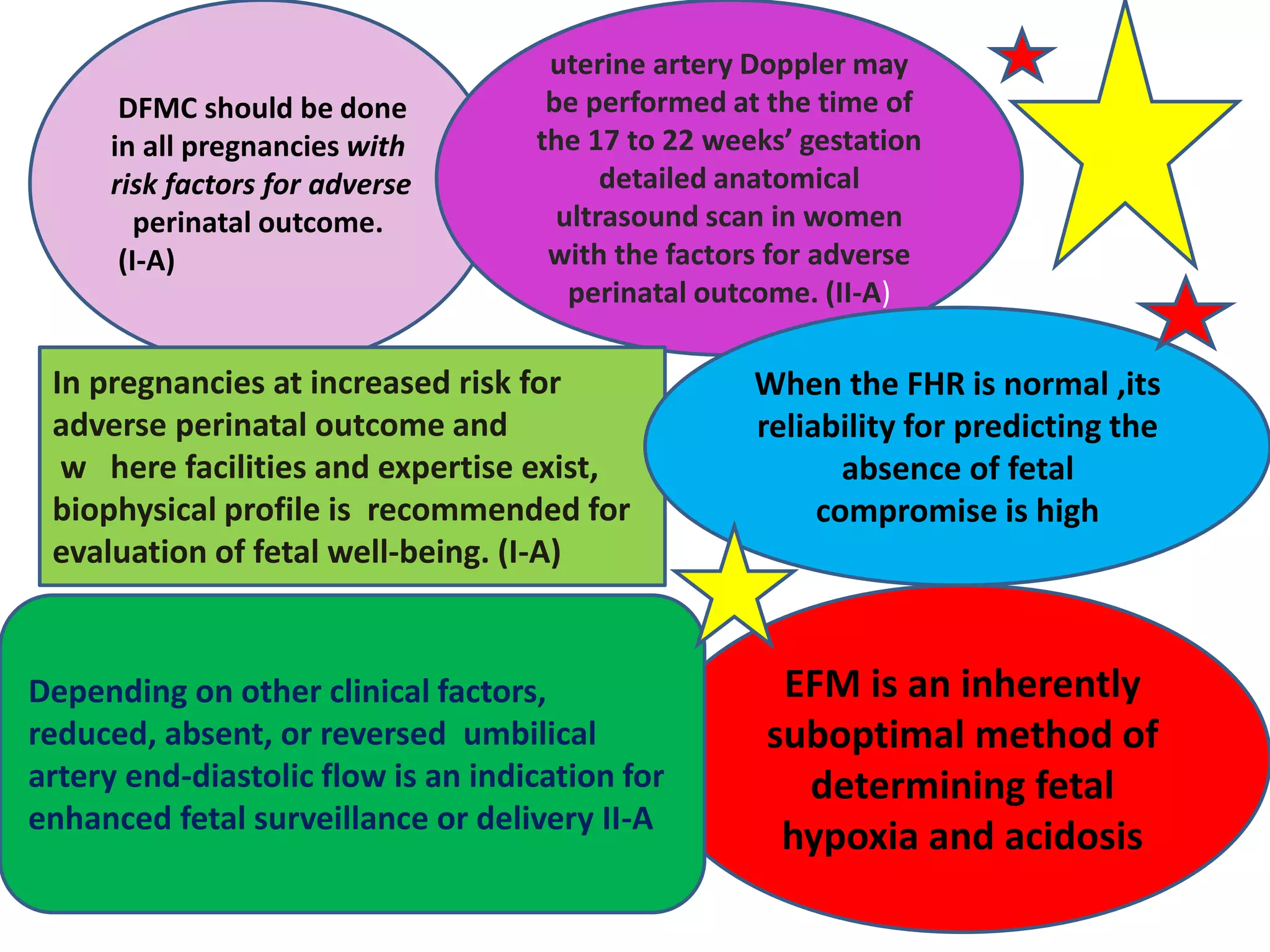
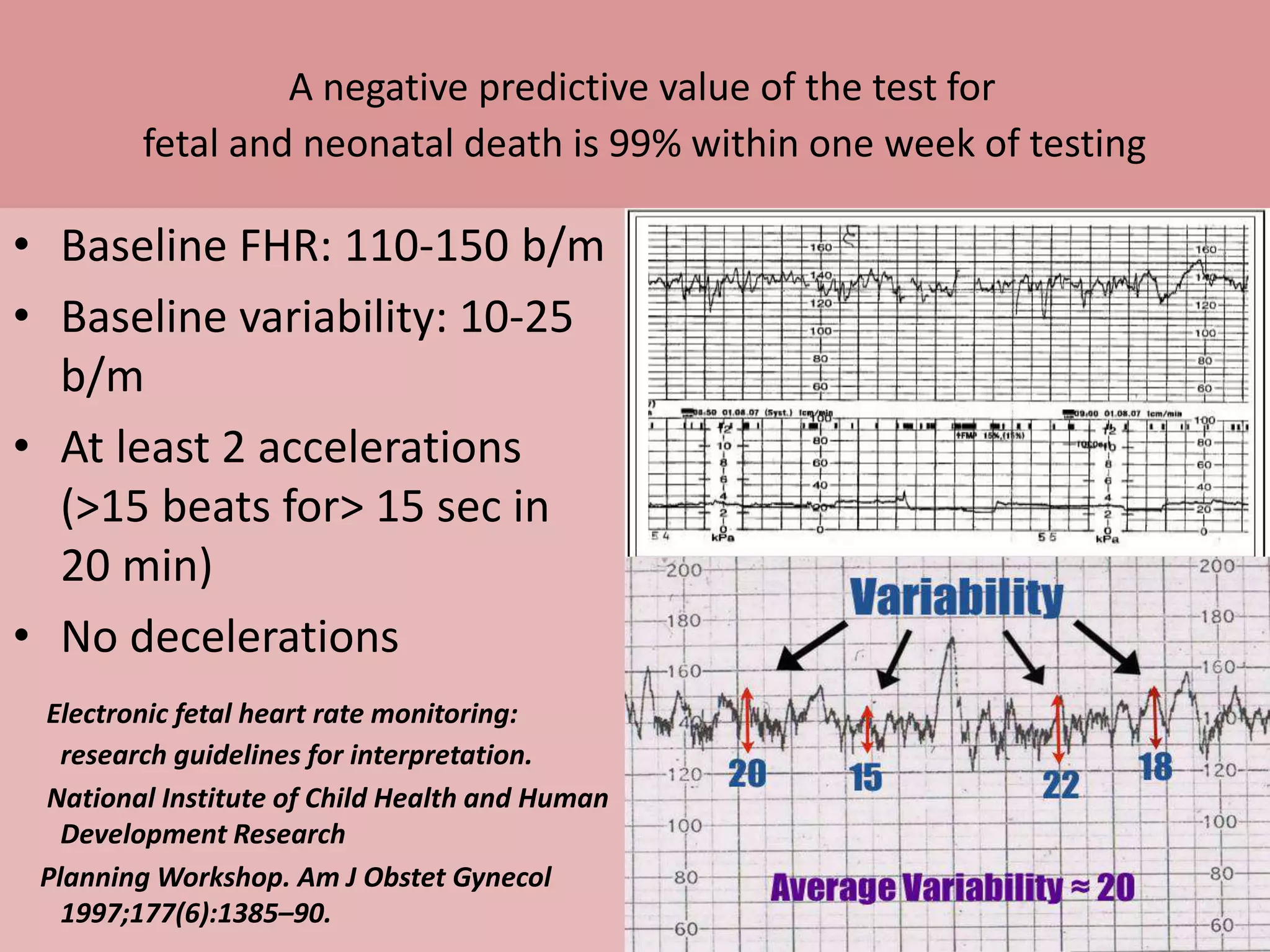
This document provides recommendations for antepartum and intrapartum fetal monitoring techniques based on evidence from studies and clinical experience. It summarizes various techniques for antepartum surveillance including fetal movement counting, non-stress tests, biophysical profiles, and Doppler assessments. For intrapartum monitoring, it recommends that intermittent auscultation be used for most low-risk pregnancies, while electronic fetal monitoring is appropriate for high-risk cases. It also provides guidance on interpreting fetal heart rate tracings and responding to atypical patterns through scalp stimulation or blood sampling. The overall goal is to prevent fetal injury through optimal timing of delivery while also avoiding unnecessary interventions.









![Non-Stress Test
Despite widespread use, there is poor evidence that
antenatal non-stress testing can reduce perinatal
morbidity or mortality.
Pattison N, McCowan L. Cardiotocography for antepartum fetal assessment [Cochrane review]. In: Cochrane
Database of Systematic Reviews1999 Issue 1. Chichester (UK): John Wiley & Sons, Ltd; 1999. DOI:
10.1002/14651858.CD001068.
In fact, the four blinded randomized trials evaluating
the non-stress test, although small, demonstrated a
trend to an increase in perinatal deaths in the
cardiotocography group (OR 2.85; 95% CI 0.99–
7.12).56](https://image.slidesharecdn.com/assessmentoffetalwellbeinginpregnancyandlabour-jaipur-150303105805-conversion-gate01/75/Assessment-of-fetal-wellbeing-in-pregnancy-and-labour-10-2048.jpg)








![.
Neilson JP, Alfirevic Z. Doppler ultrasound for fetal assessment in high risk pregnancies [Cochrane
review]. In: Cochrane Database of Systematic Reviews 1996 Issue 4. Chichester (UK): John Wiley &
Sons, Ltd; 1996.DOI: 10.1002/14651858.CD000073.
Umbilical Artery Doppler
Cochrane meta-analysis of randomized trials108
on the use of umbilical artery Doppler in
pregnancies with risk factors for adverse
perinatal outcome demonstrates a clear
reduction in perinatal mortality in normally
formed fetuses](https://image.slidesharecdn.com/assessmentoffetalwellbeinginpregnancyandlabour-jaipur-150303105805-conversion-gate01/75/Assessment-of-fetal-wellbeing-in-pregnancy-and-labour-20-2048.jpg)








![Common indications/contraindications for
intermittent auscultation
Preterm labour
Postdated labour
Epidural analgesia
VBAC
Neilson J. Electronic fetal monitoring plus scalp sampling vs intermittent auscultation
in labour[Revised May 1994]. In: Keirse M, Renfrew MJ, Neilson J, Crowther C,
editors. Cochrane Collaborative Issue 2. Oxford; 1995.
Incidence of other
pathologies is increased ….
So EFM](https://image.slidesharecdn.com/assessmentoffetalwellbeinginpregnancyandlabour-jaipur-150303105805-conversion-gate01/75/Assessment-of-fetal-wellbeing-in-pregnancy-and-labour-29-2048.jpg)

![ELECTRONIC FETAL MONITORING
• EFM compared with IA has not been shown to improve long-term
fetal or neonatal outcomes as measured by a decrease in morbidity
or mortality
• Continuous EFM during labour is associated with a reduction in
neonatal seizures but with no significant differences in long-term
sequelae, including cerebral palsy, infant mortality, and other
standard measures of neonatal well-being.
• EFM is associated with an increase in interventions, including
Caesarean section, vaginal operative delivery, and the use of
anaesthesia
Thacker SB, Stroup D, Chang M. Continuous electronic heart rate monitoring for fetal assessment during labor [Cochrane review]. In:
Cochrane Database of Systematic Reviews 2006 Issue 3. Chichester (UK): John Wiley & Sons, Ltd; 2006. DOI:
10.100214651858.CD000063.pub2.](https://image.slidesharecdn.com/assessmentoffetalwellbeinginpregnancyandlabour-jaipur-150303105805-conversion-gate01/75/Assessment-of-fetal-wellbeing-in-pregnancy-and-labour-31-2048.jpg)