Seminar on genitourinary system
- 1. SEMINAR ON GENITOURINARY SYSTEM -Suryakant Satpute F.Y.M.Sc
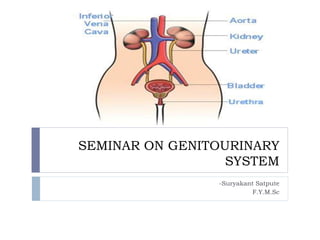
- 2. Anatomic and Physiologic Overview The urinary system comprises the kidneys, ureters, bladder, and urethra. Kidneys • The kidneys are a pair of brownish-red structures located retroperitoneally • The kidney consists of two distinct regions, the renal parenchyma and the renal pelvis. • The renal parenchyma is divided into the cortex and the medulla. • The cortex contains the glomeruli, proximal and distal tubules, and cortical collecting ducts and their adjacent peritubular capillaries.
- 4. Ureters, Bladder, and Urethra Urine, which is formed within the nephrons, flows into the ureter, a long fibromuscular tube that connects each kidney to the bladder. The ureters are narrow, muscular tubes, each 24 to 30 cm long, that originate at the lower portion of the renal pelvis and terminate in the trigone of the bladder wall. There are three narrowed areas of each ureter: the ureteropelvic junction, the ureteral segment near the sacroiliac junction, and the ureterovesical junction. The angling of the ureterovesical junction is the primary means of providing antegrade, or downward, movement of urine, also referred to as efflux of urine. This angling prevents vesicoureteral reflux, which is the retrograde, or backward, movement of urine from the bladder,
- 5. During voiding (micturition), increased intravesical pressure keeps the ureterovesical junction closed and keeps urine within the ureters. As soon as micturition is completed, intravesical pressure returns to its normal low baseline value, allowing efflux of urine to resume. Therefore, the only time that the bladder is completely empty is in the last seconds of micturition before efflux of urine resumes. The three areas of narrowing within the ureters have a propensity toward obstruction because of renal calculi (kidney stones) or stricture. Obstruction of the ureteropelvic junction is the most serious because of its close proximity to the kidney and the risk of associated kidney dysfunction
- 6. Nursing assessment: history, and physical examination Multiparous women delivering their children vaginally are at high risk for stress urinary incontinence Elderly women and persons with neurologic disorders such as diabetic neuropathy, multiple sclerosis, or Parkinson’s disease often have incomplete emptying of the bladder with urinary stasis, which may result in urinary tract infection increasing bladder pressure leading to overflow incontinence, hydronephrosis, pyelonephritis, renal insufficiency.
- 7. The patient’s chief concern or reason for seeking health care, the onset of the problem, and its effect on the patient’s quality of life The location, character, and duration of pain, if present, and its relationship to voiding Factors that precipitate pain, and those that relieve it History of urinary tract infections, including past treatment or hospitalization for urinary tract infection Fever or chills Previous renal or urinary diagnostic tests or use of indwelling urinary catheters
- 8. Dysuria and when it occurs during voiding (at initiation or termination of voiding) Hesitancy, straining, or pain during or after urination Urinary incontinence (stress incontinence, urge incontinence, overflow incontinence, or functional incontinence) Hematuria or change in color or volume of urine Nocturia and its date of onset Renal calculi (kidney stones), passage of stones or gravel in urine
- 9. Female patients: number and type (vaginal or cesarean) of deliveries; use of forceps; vaginal infection, discharge, or irritation; contraceptive practices Presence or history of genital lesions or sexually transmitted diseases Habits: use of tobacco, alcohol, or recreational drugs Any prescription and over-the-counter medications (including those prescribed for renal or urinary problems)
- 10. ASSESSMENT During physical examination for genitourinary dysfunction areas of emphasis include the abdomen, suprapubic region, genitalia and lower back, and lower extremities. Direct palpation of the kidneys may help determine their size and mobility The right kidney is easier to feel because it is somewhat lower than the left one Renal dysfunction may produce tenderness over the costovertebral angle, which is the angle formed by the lower border of the 12th, or bottom, rib and the spine.
- 11. The abdomen is auscultated to assess for bruits (lowpitched murmurs that indicate renal artery stenosis or an aortic aneurysm). The abdomen is also assessed for the presence of peritoneal fluid, which may occur with kidney dysfunction. The bladder should be percussed after the patient voids to check for residual urine Percussion of the bladder begins at the midline just above the umbilicus and proceeds downward. The sound changes from tympanic to dull when percussing over the bladder. The bladder, which can be palpated only if it is moderately distended, feels like a smooth, firm, round mass rising out of the abdomen, usually at midline Dullness to percussion of the bladder following voiding indicates incomplete bladder emptying.ich may occur with kidney dysfunction.
- 12. The prostate gland is palpated by digital rectal examination (DRE) Blood is drawn for PSA before the DRE because manipulation of the prostate can cause the PSA level to rise temporarily. The inguinal area is examined for enlarged nodes, an inguinal or femoral hernia, or varicocele (varicose veins of the spermatic cord) In female, the vulva, urethral meatus, and vagina are examined The patient is assessed for edema and changes in body weight. Edema may be observed, particularly in the face and dependent parts of the body, such as the ankles and sacral areas An increase in body weight commonly accompanies edema. A 1-kg weight gain equals approximately 1,000
- 13. UROLOGICAL OBSTRUCTIONS URETHRAL STRICTURES A urethral stricture is a scar in or around the urethra, which can block the flow of urine, and is a result of inflammation, injury or infection. Risk Factors Urethral strictures are more common in men because their urethras are longer than those in women. Thus men's urethras are more susceptible to disease or injury. A person is rarely born with urethral strictures and women rarely develop urethral strictures.
- 14. ETIOLOGY Stricture disease may occur anywhere from the bladder to the tip of the penis. The common causes of stricture are trauma to the urethra and infections such as sexually transmitted diseases and damage from instrumentation. Trauma such as straddle injuries, direct trauma to the penis and catheterization can result in strictures of the anterior part of the urethra. In adults, urethral strictures from instrumentation trauma may occur after prostate surgery and urinary catheterization. In children, urethral strictures most often follow reconstructive surgery for congenital abnormalities of the penis and urethra, cystoscopy and occasionally may be congenital.
- 15. Clinical Features Painful urination. Slow urine stream. Decreased urine output. Spraying of the urine stream. Blood in the urine. Abdominal pain. Urethral discharge. Urinary tract infections in men. Infertility in men.
- 16. Diagnostic Evaluation Evaluation of patients with urethral stricture includes a physical examination. Urethral imaging (X-rays or ultrasound). The retrograde urethrogram is an invaluable test to evaluate and document the stricture and define the stricture recurrence. Combined with antegrade urethrogram, length of the stricture can be determined.
- 17. Treatment Treatment options for urethral stricture disease are varied and selection depends upon the length, location and degree of scar tissue associated with the stricture. The main treatment options include enlarging the stricture by gradual stretching (dilation). Cutting the stricture with a endoscopic equipment (urethrotomy) and surgical repair of the stricture with reconnection and reconstruction called urethroplasty. Urethral Stents where a biocompatible hollow tube is placed on the inside of the stricture to allow for free passage of urine.
- 18. Renal Calculi Urolithiasis refers to stones (calculi) in the urinary tract. Stones are formed in the urinary tract when urinary concentrations of substances such as calcium oxalate, calcium phosphate, and uric acid increase. This is referred to as supersaturation and is depen- dent on the amount of the substance, ionic strength, and pH of the urine. Incidence The occurrence of urinary stones occurs predomi- nantly in the third to fifth decades of life and Affects men more than women. About half of patients with a single renal stone have another episode within 5 years. Most stones contain calcium or magnesium in combination with phosphorus or oxalate.
- 19. Types Of Stone Calcium stone Oxalate stone Cystiene stone Struvite stone
- 20. Calcium stone Most stones (75%) are composed mainly of calcium oxalate crystals. Increased calcium concentrations in blood and urine promote precipitation of calcium and formation of stones. Causes of hypercalcemia (high serum calcium) and hypercalciuria (high urine calcium) include the following: Hyperparathyroidism Renal tubular acidosis Cancers Granulomatous diseases (sarcoidosis, tuberculosis), which may cause increased vitamin D production by the granulomatous tissue Excessive intake of vitamin D Excessive intake of milk and alkali Myeloproliferative diseases (leukemia, polycythemia vera, multiple myeloma), which produce an unusual proliferation of blood cells from the bone marrow
- 21. Uric acid stones 5% to 10% of all stones Gout (inflammatory arthritis) myeloproliferative disorders Diet high in purines and abnormal purine metabolism Cystine stones 1% to 2% of all stones occur in patients with a rare inherited defect in renal absorption of cystine (an amino acid). Struvite stones 15% of urinary calculi form in persistently alkaline, ammonia-rich urine caused by the presence of urease splitting bacteria such as Proteus, Pseudomonas, Klebsiella, Staphy- lococcus, or Mycoplasma species. Predisposing factors for struvite stones (commonly called infection stones) include neurogenic bladder, foreign bodies, and recurrent UTIs.
- 22. Causes and predisposing factors: Chronic dehydration, poor fluid intake, and immobility Living in mountainous, desert, or tropical areas Infection, urinary stasis, and periods of immobility Inflammatory bowel disease and in patients with an ileostomy or bowel resection because these patients absorb more oxalate. Medications- antacids, acetazolamide (Diamox), vitamin D, laxatives, and high doses of aspirin
- 24. Clinical Features Pain Heamturia Dysuria Oedema Pyuria (Obstruction in urine flow, urinary retention ) Associated symptoms Nausea, vomiting, diarrhea, abdominal discomfort Chills and fever (may) Diagnostic Evaluation History Physical examination Urinanalysis Blood studies(Hyperuracemia,Hyperc alcemia Neutrophilia ) Stone chemistry Radiographic studies
- 25. NON SURGICAL MANAGEMENT Fluids are encouraged. This increases the hydrostatic pressure behind the stone, assisting it in its downward passage. A high, around-the-clock fluid intake reduces the concentration of urinary crystalloids, dilutes the urine, and ensures a high urine output. Cellulose sodium phosphate (Calcibind) may be effective in preventing calcium stones Sodium and protein restriction diet Allopurinol (zyloprim,zyloric tbs)may be prescribed to reduce serum uric acid levels and urinary uric acid excretion.
- 26. NON SURGICAL MANAGEMENT Ureteroscopy Ureteroscopy involves visualizing the stone and then destroying it. Access to the stone is accomplished by inserting a ureteroscope into the ureter and then inserting a laser, electrohydraulic lithotriptor, or ultrasound device through the ureteroscope to fragment and remove the stones ESWL (Extra Corporeal Shock wave lithotripsy) ESWL is a noninvasive procedure used to break up stones in the calyx of the kidney In ESWL, a high-energy amplitude of pressure, or shock wave, is generated by the abrupt release of energy and transmitted through water and soft tissues. Repeated shock waves focused on the stone eventually reduce it to many small pieces. These small pieces are excreted in the urine, usually without difficulty.
- 27. Endoscopic Procedures A percutaneous nephrostomy or a percutaneous nephrolithotomy may be performed, and a nephroscope is introduced through the dilated percutaneous tract into the renal parenchyma. Depending on its size, the stone may be extracted with forceps or by a stone retrieval basket. Alternatively, an ultrasound probe may be introduced through the nephrostomy tube. Electrohydraulic Lithotripsy an electrical discharge is used to create a hydraulic shock wave to break up the stone. A probe is passed through the cystoscope, and the tip of the lithotriptor is placed near the stone This procedure is performed under topical anesthesia. Chemolysis Chemolysis, stone dissolution using infusions of chemical solutions (eg, alkylating agents, acidifying agents) A percutaneous nephrostomy is performed, and the warm irrigating solution is allowed to flow continuously onto the stone.
- 28. Surgical Management Nephrolithotomy - Incision into the kidney with removal of the stone Nephrectomy – removal of kidney Pyelolithotomy - removal of stone from renal pelvis Ureterolithotomy - removal of stone from ureter Cystostomy – removal of stone from bladder Cystolitholapaxy - an instrument is inserted through the urethra into the bladder, and the stone is crushed in the jaws of this instrument
- 29. GLOMERULONEPHRITIS ,ACUTE (ACUTE NEPHRITIC SYNDROME ) Definition – Acute glomerulonephritis refers to a group of kidney diseases in which there is an inflammatory reaction in the glomeruli. It is not an infection of the kidney, but rather the result of the immune mechanisms of the body Risk factors – Group A beta- hemolytic streptococcal infection of the throat Impetigo (infection of the skin) Acute viral infections- upper respiratory tract infections, mumps, varicella zoster virus, Epstein-Barr virus, hepatitis B, and human immunodeficiency virus [HIV] infection). Antigens outside the body (eg, medications, foreign serum) In other patients, the kidney tissue itself serves as the inciting antigen.
- 30. Categories – Primary: Disease is mainly in glomeruli Secondary: Glomerular diseases that are the consequence of systemic disease Idiopathic: Cause is unknown Acute: Occurs over days or weeks Chronic: Occurs over months or years Rapidly progressing: Constant loss of renal function with minimal chance of recovery Diffuse: Involves all glomeruli Focal: Involves some glomeruli Segmental: Involves portions of individual glomeruli Membranous: Evidence of thickened glomerular capillary walls Proliferative: Number of glomerular cells involved
- 32. CLINICAL FEATURES Hematuria - The urine may appear cola-colored be- cause of red blood cells (RBCs) and protein plugs or casts; RBC casts indicate glomerular injury. Edema and hypertension Oliguria Anemia from loss of RBCs into the urine In the more severe form of the disease, patients also complain of headache, malaise, and flank pain. Elderly patients may experience circulatory overload with dyspnea, engorged neck veins, cardiomegaly, and pulmonary edema. Atypical symptoms include confusion, somnolence, and seizures, which are often confused with the symptoms of a primary neurologic disorder
- 33. Diagnostic Evaluation History On examination- kidney is large, tender, edematous and congested Urinanalysis- protienuria, hematuria , oliguria Blood studies Serum creatinine, BUN increased Hypoalbuminemia, hyperlipidemia Elevated serum IgA level Antistreptolysin O titers are usually elevated in post streptococcal glomerulonephritis Electron microscopy and immunofluorescent analysis help identify the nature of the lesion Kidney biopsy may be needed for definitive diagnosis.
- 34. TYPES OF MANAGEMENT Non pharmacological management Complete bed rest – as excessive activity may increase the protienuria and hematuria. It should be encouraged until the urine clears and BUN, creatinine and BP return to normal. Strict intake out put charting. Fluid restrictions Plasmapheresis to decrease the serum anti body level Dialysis if, uremic symptoms are severe. Dietary management- Protein restricted diet as the level of BUN and creatinine is high in blood Low fat diet due to hyperlipidemia Sodium restriction if hypertension, edema or congestive heart failure are present. Increased carbohydrate diet to provide energy and to prevent the catabolism of protein.
- 35. Pharmacological management- Residual streptococcal infection is suspected, penicillin is the agent of choice. Diuretics and antihypertensive agents may be given to control hypertension. Corticosteroids and cytotoxic agents are used to reduce the inflammation. H2 blockers (to prevent stress ulcers) Phosphate binding agents (to reduce phosphate and elevate calcium).
- 36. NURSING MANAGEMENT- Monitor vital signs, intake and output, and maintain dietary restrictions during acute phase. Encourage rest during the acute phase as directed until the urine clears and BUN, creatinine, and blood pressure normalize. (Rest also facilitates diuresis.) Administer medications as ordered, and evaluate patient's response to antihypertensives, diuretics, H2 blockers, phosphate-binding agents, and antibiotics (if indicated). Regular monitoring of blood pressure, urinary protein, and BUN concentrations to determine if there is exacerbation of disease activity. Carefully monitor fluid balance Replace fluids according to the patient's fluid losses (urine, respiration, feces) Daily body weight as prescribed. Monitor pulmonary artery pressure and CVP, if indicated. Monitor for signs and symptoms of heart failure: distended neck veins, tachycardia, gallop rhythm, enlarged and tender liver, crackles at bases of lungs. Observe for hypertensive encephalopathy, any evidence of seizure activity. Encourage patient to treat any infection promptly. Tell patient to report any signs of decreasing renal function and to obtain treatment immediately
- 37. ACUTE PYELONEPHRITIS Definition- Pyelonephritis is a bacterial infection of the renal pelvis, tubules, and interstitial tissue of one or both kidneys. Commonest microorganism- Enteric bacteria, such as E. coli, is most common pathogen other gram-negative pathogens include Proteus species, Klebsiella, and Pseudomonas. Gram-positive bacteria are less common, but include Enterococcus and Staphylococcus aureus
- 38. Clinical features- Fever, chills, headache, malaise Flank pain (with or without radiation to groin) Nausea, vomiting, anorexia Costovertebral angle tenderness Urgency, frequency, and dysuria may be present
- 39. DIAGNOSTIC EVALUATION- History – urinary obstruction, systemic infection Physical examination- pain and tenderness in the area of the costovertebral angle Urinalysis- pyuria, bactriuria, RBCs and WBCs in urine Hematology- elevated WBC count An ultrasound study or a CT scan may be performed to locate any obstruction in the urinary tract. An IV pyelogram may be indicated with pyelonephritis if functional and structural renal abnormalities are suspected Urine culture and sensitivity tests
- 40. MANAGEMENT- For severe infections (dehydrated, cannot tolerate oral intake) or complicating factors (suspected obstruction, pregnancy, advanced age), inpatient antibiotic therapy is recommended. Usually immediate treatment is started with a penicillin or aminoglycoside I.V. to cover the prevalent gram-negative pathogens; subsequently adjusted according to culture results. An oral antibiotic may be started 24 hours after fever has resolved and oral therapy continued for 3 weeks. Oral therapy antibiotic therapy is acceptable for outpatient treatment. Co-trimoxazole (Bactrim, Septran) or a fluoroquinolone is used; 10 to 14 days is the usual length of treatment. Repeat urine cultures should be performed after the completion of therapy. Supportive therapy is given for fever and pain control and hydration.
- 41. Nursing Management- Administer or teach self-administration of antibiotics as prescribed, and monitor for effectiveness and adverse effects. Assess vital signs frequently, and monitor intake and output; administer antiemetic medications to control nausea and vomiting. Administer antipyretic medications as prescribed and according to temperature. Report fever that persists beyond 72 hours after initiating antibiotic therapy; further testing for complicating factors will be ordered. Use measures to decrease body temperature if indicated; cooling blanket, application of ice to armpits and groins, and so forth. Correct dehydration by replacing fluids, orally if possible, or I.V. Monitor CBC, blood cultures, and urine studies for resolving infection
- 42. NEPHROTIC SYNDROME Definition Nephrotic syndrome is a clinical disorder characterized by marked increase of protein in the urine (proteinuria), decrease in albumin in the blood (hypoalbuminemia), edema, and excess lipids in the blood (hyperlipidemia). These occur because of increased permeability of the glomerular capillary membrane.
- 43. Classification Of Nephrotic Syndrome ETOLOGICAL CLASSIFICATION Primary NEPHROTIC syndrome. Disease limited to kidney Secondary NEPHROTIC syndrome. Other systems involved HISTOLOGICAL CLASISIFICATION MCD (Minimal change disease ) FSGN (Focal segmental glomerulosclerosis ) MN (Membranous nephropathy) MPGN (membranous proliferative glomerulonephrosclerosis)
- 44. Etiology Membranous nephropathy (MN) Hepatitis B Systemic lupus erythematosus (SLE) Diabetes mellitus Sarcoidosis Syphilis Drugs Focal segmental glomerulosclerosis (FSGS) Hypertensive Nephrosclerosis Human immunodeficiency virus (HIV) Diabetes mellitus Obesity Kidney loss Minimal change disease (MCD) Malignancy, especially Hodgkin's lymphoma
- 46. Clinical Features The major manifestation of nephrotic syndrome is edema. It is usually soft and pitting and commonly occurs around the eyes (periorbital), in dependent areas (sacrum, ankles, and hands), and in the abdomen (ascites). Patients may also exhibit irritability, headache, and malaise. Diagnostic Evaluation Urinalysis- marked proteinuria, microscopic hematuria, 24-hour urine for protein (increased) and creatinine clearance (decreased) Protein electrophoresis and immunoelectrophoresis of the urine to categorize the proteinuria Needle biopsy of kidney for histologic examination of renal tissue to confirm diagnosis Serum chemistry- decreased total protein and albumin, normal or increased creatinine, increased triglycerides, and altered lipid profile
- 47. COMPLICATIONS Complications of nephrotic syndrome include- Infection (due to a deficient immune response) Thromboembolism (especially of the renal vein) Pulmonary emboli ARF(due to hypovolemia) Accelerated atherosclerosis (due to hyperlipidemia)
- 48. MANAGEMENT Treatment of causative glomerular disease Diuretics (used cautiously) and angiotensin converting enzyme inhibitors to control proteinuria Corticosteroids or immunosuppressant agents to decrease proteinuria General management of edema Sodium and fluid restriction; liberal potassium Infusion of salt-poor albumin Dietary protein supplements Low-saturated-fat diet
- 49. Nursing Management Monitor daily weight, intake and output, and urine specific gravity. Monitor CVP (if indicated), vital signs, orthostatic blood pressure, and heart rate to detect hypovolemia. Monitor serum BUN and creatinine to assess renal function. Administer diuretics or immunosuppressants as prescribed, and evaluate patient's response. Infuse I.V. albumin as ordered. Encourage bed rest for a few days to help mobilize edema; however, some ambulation is necessary to reduce risk of thromboembolic complications.
- 50. ACUTE RENAL FAILURE Definition- Acute renal failure is a sudden and almost complete loss of kidney function caused by failure of renal circulation or by glo Etiology Pre – renal (hypoperfusion of kidney) Intra – renal (actual damage to the kidney tissue) Post – renal (obstruction to urine flow) merular or tubular dysfunction.
- 51. ETIOLOGY Pre – Renal Volume depetion Hemorrhage Renal loses GI losses Impaired cardiac efficiency Vasodilation sepsis Anaphylaxis Antihypertensive medications Post – Renal Urinary tract obstructions Renal calculi Tumors BPH Blood clots Strictutres Intra – Renal Prolonged renal ischemia Pigment nephropathy Myoglobinuria Hemoglobinuria Nephrotoxic agents Aminoglycosides agents Radiopaque contrast agents Heavy metals,Solvents and chemicals
- 52. RISK FACTORS Advanced age Blockages in the blood vessels in your arms or legs Diabetes High blood pressure Heart failure Kidney diseases Liver disease
- 53. PHASES OF ARF Initiating phase Begins with the initial insult and ends when oliguria develops Oliguric phase Urine output less than 400 ml/day Diuretic phase Urine out put become normal but nitrogenous waste products still remain elevated in blood Recovery phase It signifies the improvement of renal function It takes 3-12 months to return normal
- 54. Clinical Features Vomiting and/or diarrhea, which may lead to dehydration. Nausea. Weight loss. Nocturnal urination. pale urine. Less frequent urination, or in smaller amounts than usual, with dark coloured urine Haematuria. Pressure, or difficulty urinating. Itching. Anorexia Pruritus Seizures (if blood urea nitrogen level is very high) Bone damage. Non-union in broken bones. Muscle cramps (caused by low levels of calcium which can cause hypocalcaemia) Abnormal heart rhythms. Muscle paralysis. Swelling of the legs, ankles, feet, face and/or hands. Shortness of breath due to extra fluid on the lungs Pain in the back or side Feeling tired and/or weak. Memory problems. Difficulty concentrating. Dizziness. Low blood pressure.
- 55. PREVENTION Provide adequate hydration to patient at high risk for dehydration Prevent and treat shock with blood and fluid replacement therapy Manage hypotension Monitor critically ill patient for central venous and arterial pressures and hourly urine output to detect the onset of renal failure as early as possible. Continuously assess the renal function Prevent and treat infections Cautiously administer the blood Closely monitor the all medications that metabolized and excreted by the kidney for dosage and blood levels for the toxic effects. Pay special attention to wound, burns and other precursors of sepsis.
- 56. COMPLICATIONS ARF can affect the entire body in the form of – Infection Hyperkalaemia, Hyperphosphataemia, Hyponatraemia Water overload Pericarditis Pulmonary oedema. Reduced level of consciousness. Immune deficiency MANAGEMENT To correct fluid and electrolyte balance. To correct dehydration. To Keep other body systems working properly
- 57. RENAL AGENESIS Bilateral renal agenesis - both mesonephric ducts fail to develop. Incompatible with life. UNILATERAL RENAL AGENESIS the mesonephric duct fails to develop. Usually there is absent ureter, trigone, kidney and (in boys) vas deferens.
- 58. Horseshoe Kidney • Both metanephros are fused together. Both kidneys rotated & their lower poles are joined in the shape of a horseshoe. As the fetus grows, the joined kidneys are held up by the inferior or superior mesenteric arteries at L3.
- 59. Pelviureteric Junction Obstruction Obstruction of the junction between the renal pelvis & ureter. Clinical Features may present at any time (before birth, in childhood, or in adulthood) by: abdominal mass. abdominal pain. Haematuria after fairly minor abdominal trauma.
- 60. Diagnostic Evaluation IVU(intravenous urogram) - shows delay in appearance of contrast and dilated renal pelvis and calices. Renal scan -shows differential renal function and confirms obstruction Management Surgery is indicated for: 1. obstructive symptoms, 2. stone formation, 3. recurrent urinary infection, 4. progressive renal impairment. Pyeloplasty is the treatment of choice Nephrectomy is performed if the affected kidney is <10% of total renal function.
- 61. Vesicoureteric Junction Reflux Reflux can be defined as the retrograde flow of urine into upper urinary tract. Incidence of reflux is equal in both sexes. Reflux can be classified into 5 grades
- 62. Diagnostic Evaluation Micturating cystourethrography is the gold standard for diagnosis and evaluation of VUR grade. Diuretic Renal scan (DMSA) is used to visualize scarring and quantify differential renal function. Management antibiotic prophylaxis is recommended for children with reflux of grades I-II. Surgery (uretro - vesical reimplantation or endoscopic injection) is recommended in reflux of grades III-V and persistent reflux despite a trial of antibiotics.
- 63. Ectopic Ureter An ectopic ureter is one that opens in some location other than the bladder. 80% associated with duplicated system. 20% associated with single system. Most common sites (in female): urethra, vestibule, and vagina • In female present as urinary incontinence. Most common sites (in male): posterior urethra and seminal vesicles.
- 64. Uretrocele A congenital cystic ballooning of the terminal submucosal ureter. It is classified as simple or ectopic. Simple ( Orthotopic ) Ureterocele : in trigone. Ectopic Ureterocele : can obstruct bladder neck or even prolapse from female urethra.
- 65. Hypospadias It is a condition in which the opening of the urethra is on the underside of the penis, instead of at the tip. congenital condition results in underdevelopment of urethra. affects 3 per 1000 male infants. Consists of 3 anomalies: 1.Abnormal ventral opening of the urethral meatus. 2.Ventral curvature of the penis ( chordee ). 3.Deficient prepuce ventrally Treatment The child should be referred for urological assessment and surgical treatment. The ideal age for surgery is 6–12 months.
- 66. Epispadias Congenital condition in which the urethra opens on dorsal surface of penis.. Usually associated with bladder extrophy (ectopia vesicae). Bladder Extrophy (Ectopia vesicae) Failure of development of the lower abdominal wall. Anomaly include defect in anterior abdominal wall, defect in anterior bladder wall and epispadias (dorsal penile opening).
- 67. CANCER OF KIDNEY Incidence Cancer of the kidney accounts for about 3.7% of all cancers in adults. It affects almost twice as many men as women. The most common type of renal tumor is renal cell or renal adenocarcinoma, accounting for more than 85% of all kidney tumors. These tumors may metastasize early to the lungs, bone, liver, brain, and contralateral kidney. The incidence of all stages of kidney cancer has increased in last two decades.
- 68. Risk factors Gender: Affects men more than women Tobacco use Occupational exposure to industrial chemicals, such as petroleum products, heavy metals, and asbestos Obesity Unopposed estrogen therapy Polycystic kidney disease regular use of NSAIDs such as ibuprofen and naproxen, faulty genes; a family history of kidney cancer; having kidney disease that needs dialysis; being infected with hepatitis C;
- 69. Clinical Features Many renal tumors produce no symptoms and are discovered on a routine physical examination as a palpable abdominal mass. The classic triad of signs and symptoms, comprises hematuria, pain, and a mass in the flank. The usual sign that first calls attention to the tumor is pain- less hematuria, which may be either intermittent and microscopic or continuous and gross. There may be a dull pain in the back from the pressure produced by compression of the ureter, extension of the tumor into the perirenal area, or hemorrhage into the kidney tissue. Colicky pains occur if a clot or mass of tumor cells passes down the ureter. weight loss, increasing weakness, and anemia.
- 70. Assessment and Diagnostic Findings The diagnosis of a renal tumor may require intravenous urography, cystoscopic examination, nephrotomograms, renal angiograms, ultrasonography, CT scan. Management-Surgical management A radical nephrectomy is the preferred treatment if the tumor can be removed. This includes removal of the kidney (and tumor), adrenal gland, surrounding perinephric fat and Gerota’s fascia, and lymph nodes. Radiation therapy, hormonal therapy, or chemotherapy may be used along with surgery. Immunotherapy Nephron-sparing surgery
- 71. Pharmacological Management use of biologic response modifiers such as interleukin-2 (IL2) and topical instillation of bacillus Calmette-Guerin (BCG) Patients may be treated with IL-2, a protein that regulates cell growth. This may be used alone or in combination with lymphokine-activated killer cells Interferon, another biologic response modifier, appears to have a direct antiproliferative effect on renal tumors. Renal Artery Embolization In patients with metastatic renal carcinoma, the renal artery may be occluded to impede the blood supply to the tumor and thus kill the tumor cells.
- 72. CANCER OF BLADDER Cancer of the urinary bladder is more common in people aged 50 to 70 years. It affects men more than women (3:1) There are two forms of bladder cancer: superficial (which tends to recur) and invasive. About 80% to 90% of all bladder cancers are transitional cell (which means they arise from the transitional cells of the bladder); the remaining types of tumors are squamous cell and ade- nocarcinoma.
- 73. Risk Factors Cigarette smoking: risk proportional to number of packs smoked daily and number of years of smoking Environmental carcinogens: dyes, rubber, leather, ink, or paint Recurrent or chronic bacterial infection of the urinary tract Bladder stones High urinary pH High cholesterol intake Pelvic radiation therapy Cancers arising from the prostate, colon, and rectum in males
- 74. Clinical Manifestations Bladder tumors usually arise at the base of the bladder and involve the ureteral orifices and bladder neck. Visible, painless hematuria is the most common symptom of bladder cancer. Infection of the urinary tract is a common complication, producing frequency, urgency, and dysuria. Any alteration in voiding or change in the urine, however, may indicate cancer of the bladder. Pelvic or back pain may occur with metastasis. Assessment and Diagnostic Findings The diagnostic evaluation includes – cystoscopy (the mainstay of diagnosis), excretory urography, a CT scan, ultrasonography, bimanual examination with the patient anesthetized. Biopsies of the tumor and adjacent mucosa
- 75. Management- Surgical Transurethral resection or fulguration (cauterization) may be per- formed for simple papillomas (benign epithelial tumors). eradicate the tumors through surgical incision or electrical current with the use of instruments inserted through the urethra. After this bladder-sparing surgery, intravesical administration of BCG is the treatment of choice. A simple cystectomy (removal of the bladder) or a radical cystectomy is performed for invasive or multifocal bladder cancer. Radical cystectomy in men involves removal of the bladder, prostate, and seminal vesicles and immediate adjacent perivesical tissues.
- 76. Management- Pharmacological Chemotherapy with a combination of methotrexate, 5-fluorouracil, vinblastine, doxorubicin (Adriamycin), and cisplatin Intravenous chemotherapy may be accompanied by radiation therapy. Topical chemotherapy (intravesical chemotherapy or instillation of antineoplastic agents into the bladder, resulting in contact of the agent with the bladder wall) is considered when there is a high risk for recurrence, when cancer in situ is present, or when tumor resection has been incomplete. Topical chemotherapy de- livers a high concentration of medication (doxorubicin, mitomycin, ethoglucid, and BCG) to the tumor to promote tumor destruction. BCG is now considered the most effective intravesical agent for recurrent bladder cancer because it enhances the body’s immune response to cancer. Management- Radiation Therapy Radiation of the tumor may be performed preoperatively to reduce microextension of the neoplasm and viability of tumor cells,
- 77. THANK YOU