EAU NMIBC RISK CALCULATOR.pptx
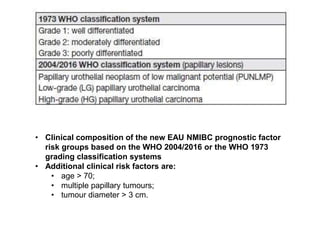
- 1. • Clinical composition of the new EAU NMIBC prognostic factor risk groups based on the WHO 2004/2016 or the WHO 1973 grading classification systems • Additional clinical risk factors are: • age > 70; • multiple papillary tumours; • tumour diameter > 3 cm.
- 2. Risk group Low Risk • A primary, single, Ta/T1 LG/G1 tumour < 3 cm in diameter without CIS in a patient < 70 years • A primary Ta LG/G1 tumour without CIS with at most ONE of the additional clinical risk factors (see above*) Intermediate Risk Patients without CIS who are not included in either the low, high or very high-risk groups High Risk • All T1 HG/G3 without CIS, EXCEPT those included in the very high-risk group • All CIS patients, EXCEPT those included in the very high-risk group Stage, grade with additional clinical risk factors: • Ta LG/G2 or T1 G1, no CIS with all 3 risk factors • Ta HG/G3 or T1 LG, no CIS with at least 2 risk factors • T1 G2 no CIS with at least 1 risk factor Very High Risk Stage, grade with additional clinical risk factors: • Ta HG/G3 and CIS with all 3 risk factors • T1 G2 and CIS with at least 2 risk factors • T1 HG/G3 and CIS with at least 1 risk factor • T1 HG/G3 no CIS with all 3 risk factors
- 4. EAU NMIBC RISK CALCULATOR 1. Age 1. ≤ 70 years >70 years 2. Tumor Status 1. Primary Recurrent 3. Number of Tumors 1. Single Multiple 4. Maximum Tumor Diameter 1. <3 cm ≥3 cm 5. Stage 1. Ta T1 6. Concomitent CIS 1. NO Yes Select Classification System 1. WHO Grade 2004/2016 1. LMP-LG HG 2. WHO Grade 1973 1. G1 G2 G3
- 8. Whenever a MIBC is detected during follow-up. BCG-refractory tumour 1. If T1G3/HG tumour is present at 3 months [196, 291, 294] (LE: 3). 2. If TaG3/HG tumour is present after 3 months and/or at 6 months, after either re- induction or first course of maintenance [43] (LE: 4). 3. If CIS (without concomitant papillary tumour) is present at 3 months and persists at 6 months after either re-induction or first course of maintenance. If patients with CIS present at 3 months, an additional BCG course can achieve a complete response in > 50% of cases [43, 44, 284] (LE: 1b). 4. If HG tumour appears during BCG maintenance therapy*. BCG-relapsing tumour Recurrence of G3/HG (WHO 1973/2004) tumour after completion of BCG maintenance, despite an initial response [288] (LE: 3). BCG unresponsive tumour Recurrence of G3/HG (WHO 1973/2004) tumour after completion of BCG maintenance, despite an initial response [295] (LE: 3). BCG intolerance Severe side effects that prevent further BCG instillation before completing treatment [266].
- 12. Guidelines for the treatment of TaT1 tumours and carcinoma in situ according to risk stratification
- 13. Treatment options for the various categories of BCG failure
- 14. 14 Progression of NMIBC • Recurrenace rate: 70% within 5yr • Progression: 10-20% • Mortality 1-15% • Upper tract tumor: 2% • Stage Ta: 70% – – – 50% will recur , 50% never recur If FC 3/12 show recurrence , risk of further recurrence 90% 5% progress • Stage T1: 20% – 20% 5yr mortality – 80% recur – 30% T1G3 progress – high progression 80% if concomittent CIS – 30% T1G3 is understage at RC – Become T2 if untreated in 2 years – 50% will progress to muscle invasive • • • CIS: 10% primary , 20% with tumor present Percentage of occult metastasis of T2 disease - 33% Percentage of patients submitted to radical cystectomy present with lymph node involvement at the time of surgery - 25%
- 16. 16 Adjuvant Intravesical Chemotherapy • One immediate post-op intravesical instillation • Additional intravesical chemo instillations • Optimizing intravesical Chemo • Adj IVBCG (indication) • Optiomal BCG schedule • BCG toxicity
- 17. Role of one, immediate, post-operative intravesical instillation of chemotherapy • Indication: everyone – – – As sole intravesical txn in low risk of recurrence and progression As initial stage of further intavesical therapy in intermediate risk Also indicated in high risk gp to reduce recurrence, although subsequent BCG is essential • MOA: Mitomycin C – – Alkylating and intercalating agent of DNA in bladder tumor cell Destruction of circulating tumour cells and chemoresection of residual microscopic tumor at the site of TURBT • Timing: Within 24 hours, EORTC: <6hrs Dosage: 40mg in 40ml NS/H20 Procedure: – Instill into empty bladder, clamp for 1hr then release • •
- 18. 18 To further improve the efficacy of intravesical chemotherapy • Completely bladder emptying • Changing the position of the patient • 6-h fasting period (do not drink in the morning) – Decreases urinary output – Prevents up to 20% drug dilution • Oral sodium bicarbonate (urine pH > 7) – Improve drug stability, cell uptake & penetration
- 19. 19 Local microwave hyperthermia • Induces bladder wall hyperthermia around 40C with a special catheter • Internal thermocouples to monitor the temperature • Used in combination with intravesical MMC (thermochemotherapy) showed superiority over MMC alone • Significantly more side-effects, though moderate and transient • Approved in US Colombo R et al. Multicentric study comparing intravesical chemotherapy alone and with local microwave hyperthermia for prophylaxis of recurrence of superficial transitional cell carcinoma. J Clin Oncol 2003;21:4270–6
- 21. 21 Mechanism of IVBCG • • • First use in TCC bladder by Morales in 1976 Live attenuated Mycobacterium bovis Many strains (Pasteur, Connaught, Tice, Tice / RIVM, RIVM, A. Frappier) - All strains same MOA: • – – – – – Precise mechanism remains unknown Attachment of BCG to urothelial cell Promotes a local acute inflammatory & sub-acute granulomatous reaction with macrophage leukocyte infiltration in the urothelium and lamina propria Local inflammatory effects are associated with an elimination or reduction of superficial cancerous lesions of the urinary bladder – Induces accumulation of granulocytes and the influx of macrophages and lymphocytes into urothelium (maintainence therapy) • BCG granuloma consists of epitheloid cells, Langerhan’s giant cell and lymphocytes More recent evidence suggests that an increase nitric oxide synthetase activity may be implemented •
- 22. 22 Indication of IVBCG • Low risk disease → No; due to over-treatment • High risk disease → Yes – First line treatment for high risk bladder TCC, CIS, G3pT1 and multifocal G2pT1 • Intermediate-risk disease → Yes – BCG with 1 yr of maintenance is more effective then chemo for preventing recurrence – However , BCG has more side effect then chemo – Thus both BCG & chemo remains an options
- 24. 24 BCG • Adjuvant therapy – 2-4 week after TURBT • Connaught strain : 81mg in 50ml NS • Instillation via catheter, immediately removed • BCG held in bladder to up to 2 hour • After 2hour: increase fluid intake and void regularly
- 25. 25 BCG evidence: Better than TURBT alone • In terms of recurrence : Yes – Reduced time to first recurrence [Shelly BJU 2001] – Reduced recurrence rate by 47% [Meta-analysis of 6 trial, Shelley, BJU 2001] • In terms of progression: – Cannot conclude effect of BCG on tumor progression [Shelley BJU 2001] • Thus meta-analysis on progression is needed
- 26. 100 BCG evidence: Reduce risk of Progression • • • Meta-analysis of 24 trial EORTC [Sylvester JU 2002] TUR + BCG vs TUR alone vs other txn Result: – – 4% absolute risk reduction of progression (13%vs 9%) 27% relative risk reduction of progression • • • Only pt receiving maintenance BCG benefit The benefit of BCG is the same for papilary Ca and CIS NO significant difference in treatment effect for OS or death due to CaB Conclusion: • – – BCG significantly reduces the risk of progression to muscle invasive disease after transurethral resection in patients with NMIBC who receive maintenance BCG BCG is considered to be the drug of choice for adjuvant treatment after transurethral resection in intermediate and high risk patients with papillary tumors and is the best intravesical treatment for carcinoma in situ.
- 27. 27 BCG evidence: BCG better then MMC • In terms of recurrence: Yes – Absolute risk reduction of 20% & relative risk reduction of recurrence of 60% [MA Sylvester JU2005] – Only in those patients at high risk of tumour recurrence [Cochrane 2008] – Only with BCG maintenance: 32 % reduction in the risk of recurrence [MA Sylvester EU2009] • In terms of progression: Yes – 4% decrease in preventing tumor progression , but only if maintenance is given [MA of 9 trial Bohle JU2004] – 26% reduction in the risk of progression [MA Sylvester 2005] – However, no difference in term of progression in one MA [Sylvester EU2009] • In terms of overall survival and cancer specific survival – No difference [Sylvester EU2009] • In particular , BCG is more effective than MMC in CIS: – – Response rate: 70% vs 50% Overall disease free rate: 50% in BCG group and 25% in chemo group (median Fu 4yr)
- 28. 28 BCG evidence: Maintenance • • • • SWOG 85-07 (RCT by Lamm, J Uro 2000) Ta/1 high risk pt Receive primary treatment + 6w induction → randomized if no recurrence Randomized: – Maintenance: 3 weekly BCG @ 3, 6, 12, 18, 24, 30, 36m – No maintenance • Result: Maintenance therapy is able to: – – – Reduce and delay recurrence Delay time to progression Suggestion of survival benefit : 5yr OS (83% vs 78%) • Only patients receiving maintenance BCG benefited in terms of recurrence and progression • The downside of that study was that only 16% of patients randomized to maintenance BCG completed the full course
- 29. 29 Lamm’s Regime • • • • Post –TURBT : 6-week induction course 3-week course at 3 months 3-week course at 6 months 3 week course every 6 months up to 3 years (total 27) – cytokine response with second 6 week course peaks by week three and may be suppressed during weeks 4-6 – Lymphocytic infiltration and delayed cutaneous hypersensitivity response weaken after 6 month – Repeated stimulation of immune system
- 30. 30 Rationale - 3 weekly maintanence • After exposure to an antigen, the secondary immune response occurs more rapidly and is more vigorous. • Induction course: 6 week for peak immune response (urinary cytokine excretion) • Maintanence course: 3 weeks for peak immune response (and is suppressed in week 4,5 and 6)
- 31. 31 Rationale – 6 monthly afterwards • Duration of immune stimulation and protection from recurrence following BCG instillation appears to be long term • However, lymphocytic infiltration, delayed cutaneous hypersensitivity response and immunoproliferative response persist as little as 6 months • TF: 6 monthly maintenance schedule may be biological significance
- 32. 32 Rationale – 3 years • Should consider, safety, cost and biology of the immune response • In an RCT of 1,355 patients, the EORTC has shown that when BCG is given at full dose, three years' maintenance (3-weekly instillations 3, 6, 12, 18, 24, 30 and 36 months) reduces the recurrence rate compared to one year in high - but not in intermediate-risk patients.
- 33. 33 2nd Induction course • The complete response of those who failed to respond to the first course of BCG was 60% by a second course
- 34. 34 Conclusion • Most effective intravesical agent for preventing NMIBC recurrence • Role in progression still controversial • BCG as alternative to IVCT in intermediate risk NMIBC • Recommended as standard of care for high risk NMIBC • Reduction in risk of progression in high and intermediate risk [EAU 2020] • Requires maintenance schedule for benefit • No maintenance → no benefit in High Risk
- 35. 35 Role of reduced dosage of IVBCG • • Connaught 81mg vs 27mg The Spanish CUETO trial concluded that low dose BCG is equally effective to high dose BCG. Except marginal superiority of standard dose in G3 and high risk tumours of full dose Reduced toxicity in reduced dose arm Although fewer patients reported toxicity with the reduced dose, the incidence of severe systemic toxicity was similar in the standard- and reduced-dose groups This group suggested one-third of the standard dose of BCG may be the minimum effective dose in intermediate-risk tumours • • • •
- 39. 39 Precautions after IVBCG 1. Sitting down to void in order to avoid splashing 2. Hand washing after voiding 3. Rinsing toilet with undiluted bleach 4. Theoretical risk of BCG infection through genital tract during intercourse – – Should not have sex 48 hours after each treatment A condom is advised during the treatment till 6 weeks afterwards 5. Quinolones should be avoided due to anti-TB activity 6. BCG can be used in joint and valvular prosthesis with antibiotic cover for urethral instrumentation
- 40. 40
- 41. 41 Role of 2nd Induction therapy after failure of induction After induction BCG in CIS: • If Recurrence at 3m – Re-induction → 50% complete response • If Recurrence at 3m and 6m (i.e. BCG - refractory) – 30% progress, 50% metastasis • If Late recurrence after >6m success – Re-induction → 80% complete response at 6m, → 50% at 5yr In T1 failure: – re-BCG → 70% progress to MI – No evidence that repeat induction improve out come of T1G3
- 42. 42 BCG failure Options • Early Cystectomy (80% cure before MI) – Early cystectomy show survival benefit than conservative treatment (don’t wait till MI) [Raj JU2007] – Cystectomy also better in primary MI gp than progression to MI gp • Intravesical chemotherapy – Gemcitabine, docetaxel (investigational) • Device assisted instillation – EMDA, HYMN (recurrence 15% at 1 year) • Immunotherapy (interferon + BCG 45% tumor free at 4yr)
- 43. 43 Indication of cystectomy for NIMBC • High risk of progression. According to the risk tables of the EORTC 1. Multiple recurrent HG tumors: risk of progression ↑ to 80% 2. T1HG 3. HG tumor with concurrent CIS 4. BCG failure 5. Lymphovascular invasion 6. Involvement of distal ureters or prostatic urethra 7. Too large or anatomically inaccesible to be removed in their entirety endoscopically • A delay in cystectomy increases the risk of progression and cancer-specific death – Herr HW, et al. Does early cystectomy improve the survival of patients with high risk superficial bladder tumors?. J Urol 2001;166(4):1296-9.
- 44. 44 FU of patients with T1Ta disease • Result of 1stcystoscopy is a very important prognostic factor for recurrence and progression 1stcystoscopy should always performed 3m after TUR EAU 2020 low risk tumor after TURBT • • – Recurrence 20% at 1 year – Cystoscopy at 3 months – If –ve: FC 9 months later then yearly for 5 years. • Intermediate risk tumor after TURBT – Recurrence 40%@1year, 60%@2yr – In-between follow-up scheme using cystoscopy and cytology • High risk tumor after TURBT: – – – Recurrence 50% at 6m, 90% @1year Cystoscopy + cytology at 3m If –ve: FC+ Cytology Q3m x 2 year FC + Cytology Q6m x 3 year (till 5yr) FC + cytology yearly + upper tract imaging yearly • AUA : – 3 monthly x 2yr – then 6 monthly x 2-3 yr – then yearly •
- 45. 45 CIS • • • Definition: Flat, non invasive high grade malignancy of the bladder 5-10% of NMIBC Classified: – – – Primary CIS: isolated CIS 2nd CIS: CIS with previous papillary tumor Concurrent CIS: CIS in the presence of papillary tumors • How does it behave? – – – – – Lead to invasive disease in 2 yr if not treated With BCG: complete response 70% 14% progress to T1 Progression: 50% if alone, 80% if with G3 disease 7% dies of Ca bladder • Dx: – – – Cytology : SV 94% , SP 96% White light FC: 53% of CIS missed Fluoresence FC: improve detection rate of CIS > 95%
- 46. 46 • Treatment: – – – – – – Mainstay of treatment is IVBCG With MIBC → treat as MIBC With Ta/T1→ TURBT + BCG Early cystectomy : 50% overtreatment RT: not an option BCG with maintenance up to 3 yr is more effective than MMC : [Sylvester JU 2005] • Response rate: 70% vs 50% • 5 yr Overall disease free rate: 50% vs 25% • 30% remain disease free at 10 yr – BCG reduced risk of progression by 35% vs MMC [Sylvester JU 2002] 50% who do not response to initial induction BCG will response to 2nd induction course (6 weekly) Alternating schedule of MMC and BCG is not superior to BCG alone [Nordic trail] Conclusion: BCG increase complete response rate, overall disease free rate & reduce progression in patient with CIS Upper tract CIS: txn with BCG asso with more BCS Cx as more systemic absorption • • • •
- 47. 47
- 54. 54 Micropapillary Variant • • • Male-predominant (5:1) Aggressive tumor, 85% present as metastasis Gross pathology – Highly variable, from a strikingly ulcerated mass to seemingly benign granular mucosa Not responsive to BCG Mostly with lymphovascular invasion • • • • Cystectomy treatment of choice 5-year and 10-year overall survival: 51% and 24% – MD Anderson Cancer Cancer: review of micropapillary Ca bladder (Cancer 2007)
- 55. 55 Risk of LN met according to T stage • Ta 6% • T1 10% • T2/3a 18% • T3b/4 30%
- 56. 56 SCC • Bilharzial (Schistosomasis ) – – – – – Exophytic, nodular, fungating lesions usually well differentiated & present as low grade disease relatively low incidence of lymph node and distant metastases. Ureteric involvement complicates 25% of cases of bladder bilharzias. The lower third of the ureter is most commonly affected (80%) and is usually bilateral • Nonbilharzial SCCs – caused by chronic irritation from urinary calculi, long-term indwelling catheters, chronic urinary infections, or bladder diverticula – Prognosis is poor because most patients have advanced disease at the time of diagnosis • Histology – Characteristically of keratinized islands that contain eccentric aggregates of cells called squamous pearls Cystoscopy: invasive ulcerative lesion at trigone or lateral wall Treatment: cystectomy 10% present as metastasis 5yr survival: 50% • • • •
- 57. 57 Adenocarcinoma • • <1% of bladder cancer 2 types: – – Primary: de novo (trigone, or post wall) Secondary: metastatic (bowel) or urachal remnant • Risk factor: – – – Bladder extrophy / bowel augmentation / bladder substitution ( after 10-20yr) Patent urachus Association with cystitis glandularis • Urachal tumor: – – – – More common in female Presentation: hematuria + mucous discharge from urachus Sharp demarcation between tumour and urothelium Histologically, adenoca (85%), sarcoma (8%), SCC (3%) or even TCC (3%) • 25% of bladder adenoca Radiologically (CT scan) there is a stipples calcification in 50% of them, when present is almost pathognomonic Treatment: either extended partial or radical cystectomy + excision of the urachus and umbilicus depending on the clinical staging Overall 5 year survival rate is 50% – – –
- 58. 58
- 59. 59 Evidence of fluorescence Cystoscopy for Ca Bladder • Meta-analysis [Kausch, EU 2010] – More sensitive than conventional procedures in detecting malignant tumour – 20% (95% CI, 8–35) more tumor-positive patients were detected with PDD in NMIBC – 40% (CI, 23–57) more in subgroup CIS only – Residual tumor was significantly less often found after PDD (odds ratio: 0.28; 95% CI, 0.15–0.52; p < 0.0001) – Recurrence-free survival was higher at 12 and 24mo in the fluorescence-guided TUR than in the WLI-only groups (p<0.0002) fluorescence guided TUR reduced recurrence up to 5 years (ALA) – Recurrence rate at 5 years 75% vs 59% (Danitchenko J Urol 2005) •