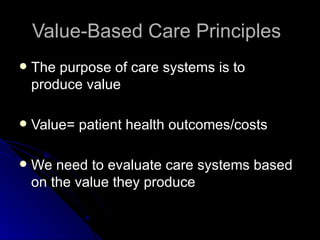
1) The document discusses aligning healthcare reimbursement systems with value-based care principles by focusing on patient outcomes over volume of services.
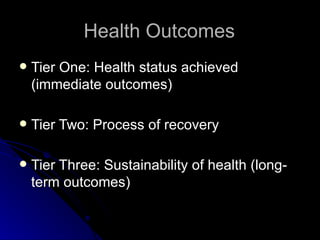
2) It proposes defining integrated practice units that take accountability for the full cycle of care for a condition and bundling payments based on outcomes achieved.
3) The project aims to develop and test an outcomes-based reimbursement model for rheumatoid arthritis care in Stockholm County Council by defining important outcomes, experimenting with a prototype using historical data, and evaluating its effects and risks.