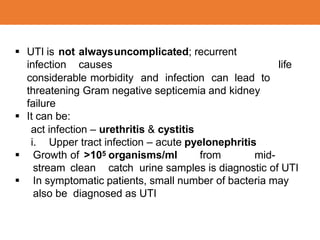
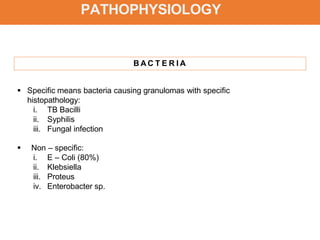
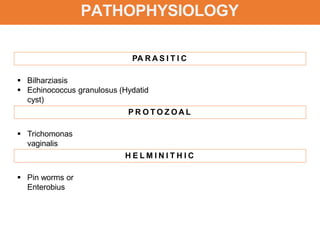
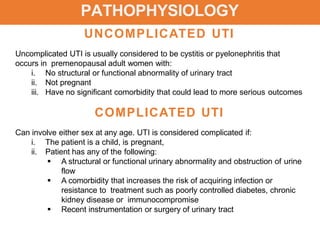
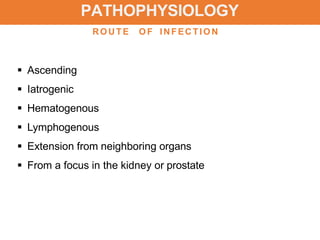
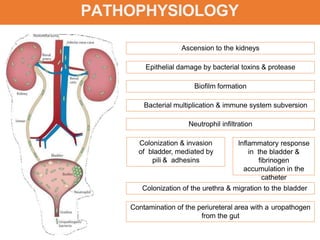
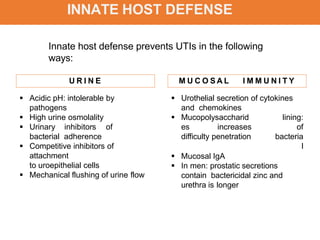
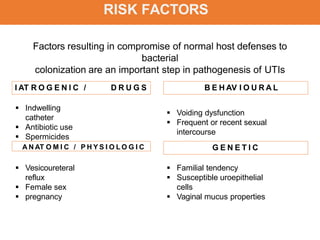
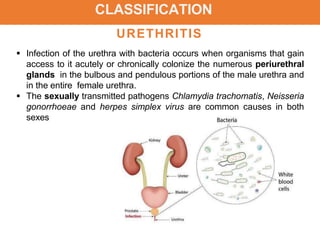
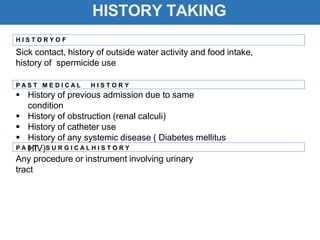
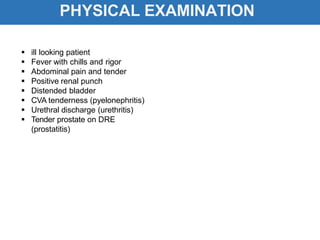
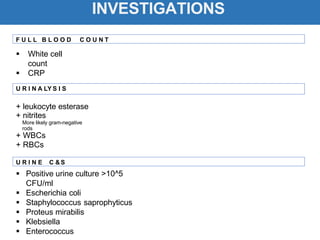
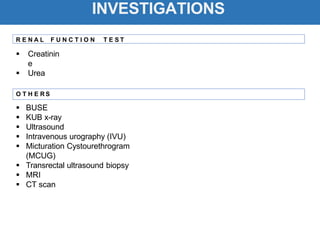
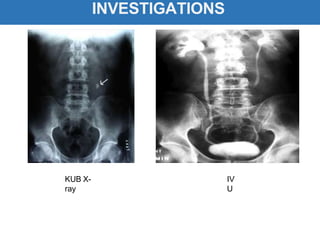
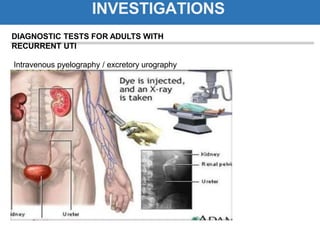
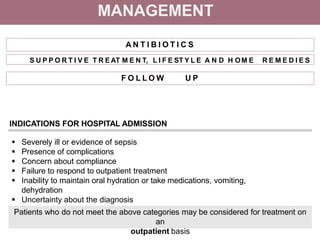
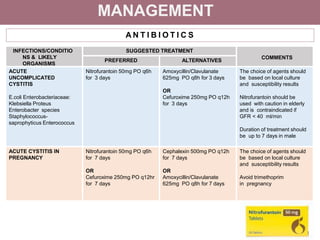
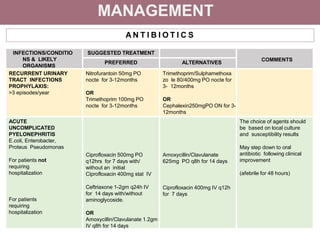
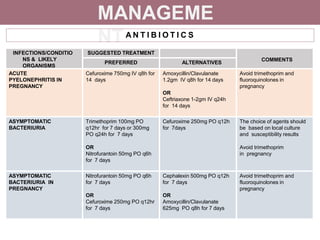
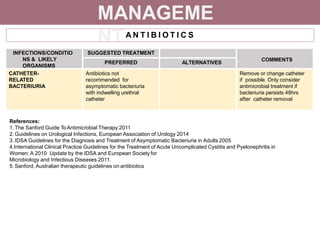
The document provides comprehensive information on urinary tract infections (UTIs), outlining their prevalence, classification, and pathophysiology, particularly highlighting differences between uncomplicated and complicated cases. It discusses the identification of causative organisms, risk factors, and recommended management strategies including antibiotic treatments and supportive care. The document emphasizes the importance of addressing underlying conditions and conducting follow-up investigations to mitigate recurrent infections.