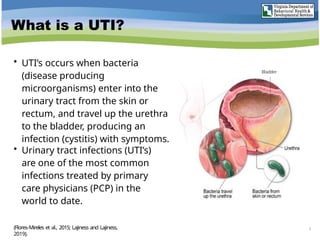
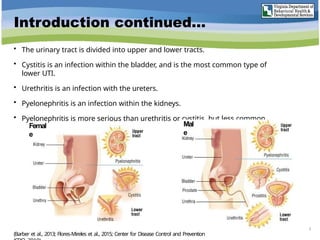
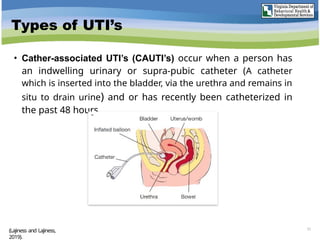
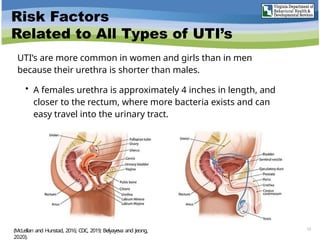
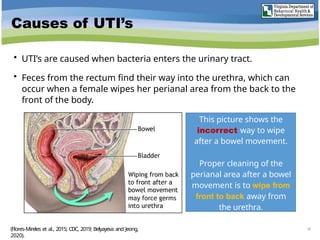
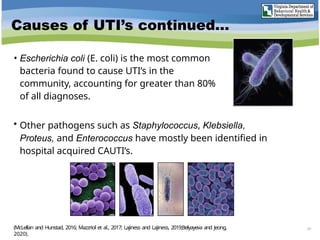
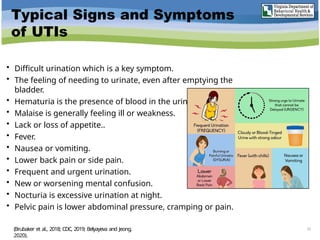
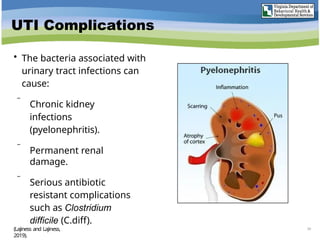
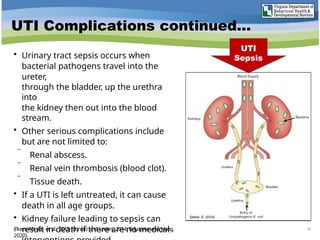
Urinary tract infections (UTIs) are caused by bacteria entering the urinary tract, leading to symptoms like painful urination and frequent urges to urinate. There are various types of UTIs, including uncomplicated, complicated, recurrent, and catheter-associated infections, with women being at higher risk due to anatomical factors. Effective treatment typically involves antibiotics, and prevention strategies include proper hygiene, hydration, and, in some cases, prophylactic antibiotic use.