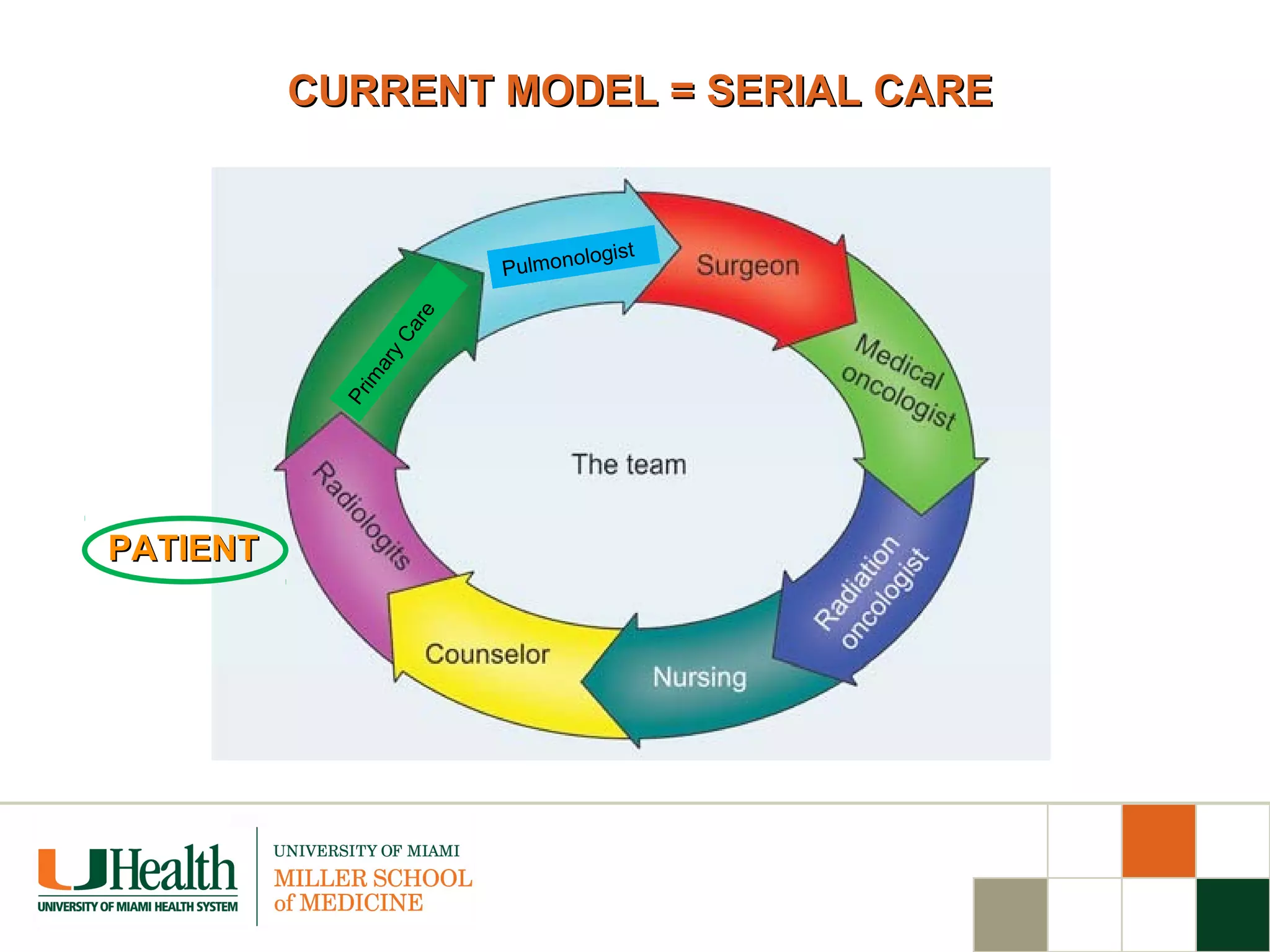
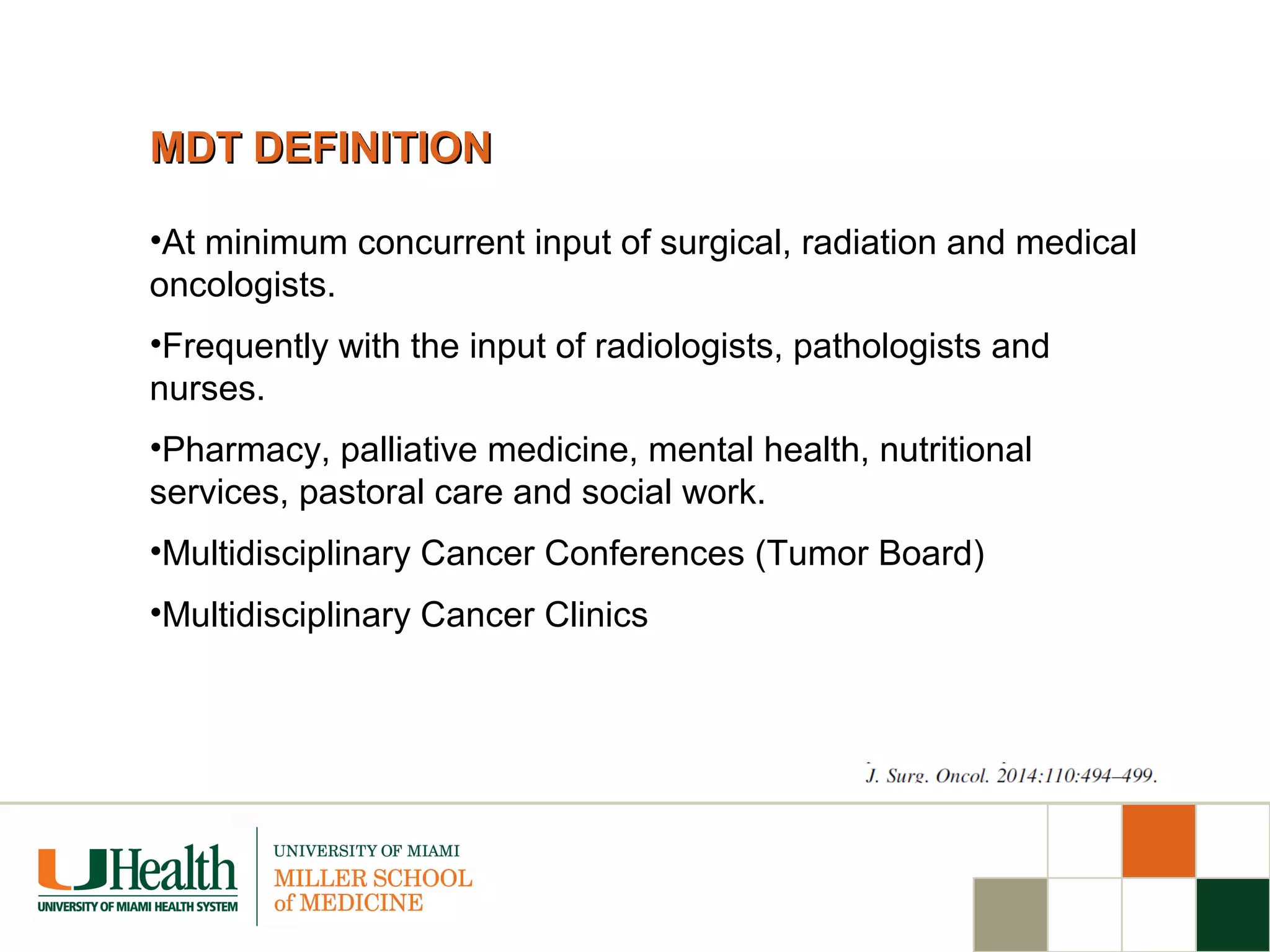
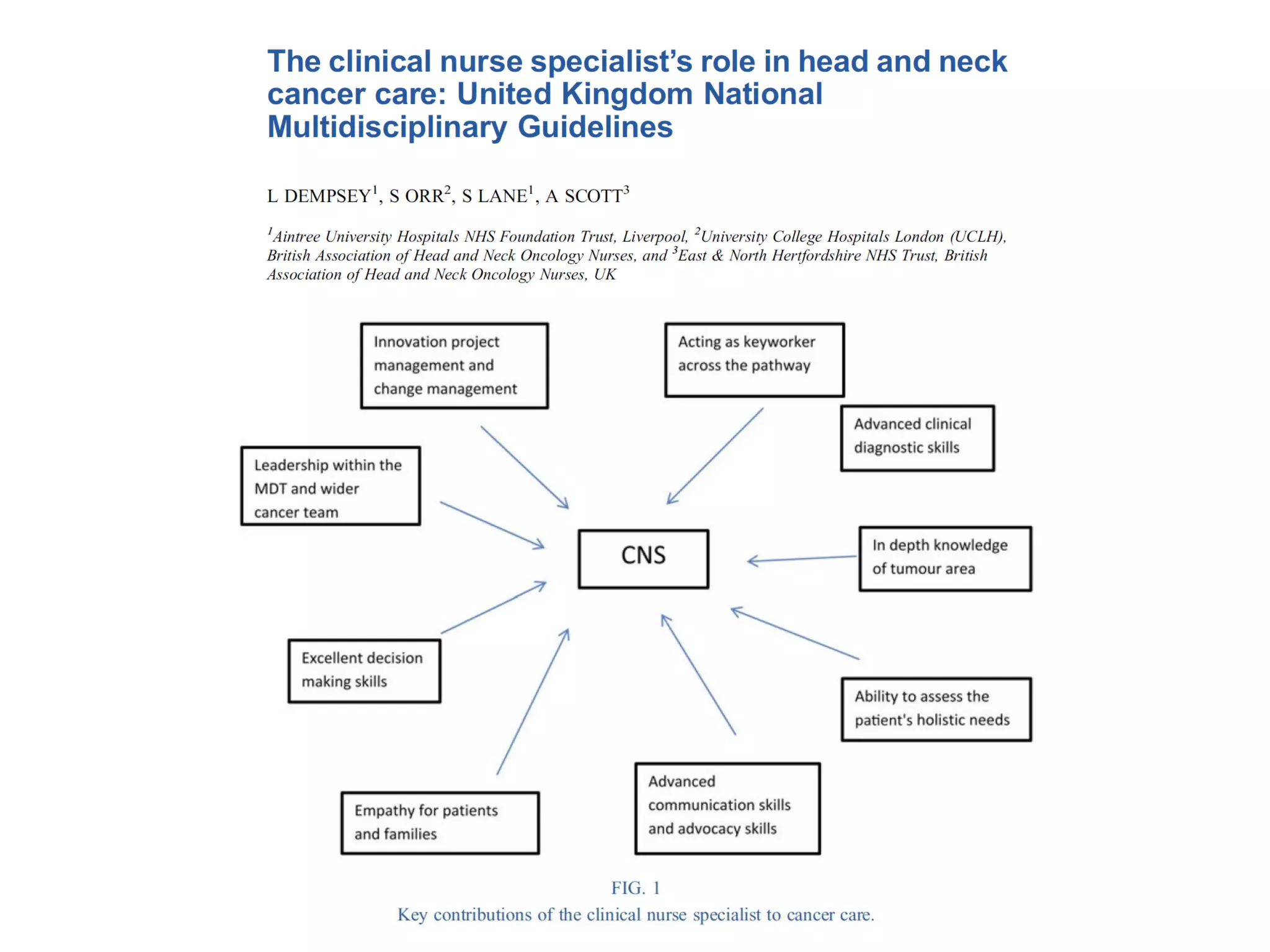
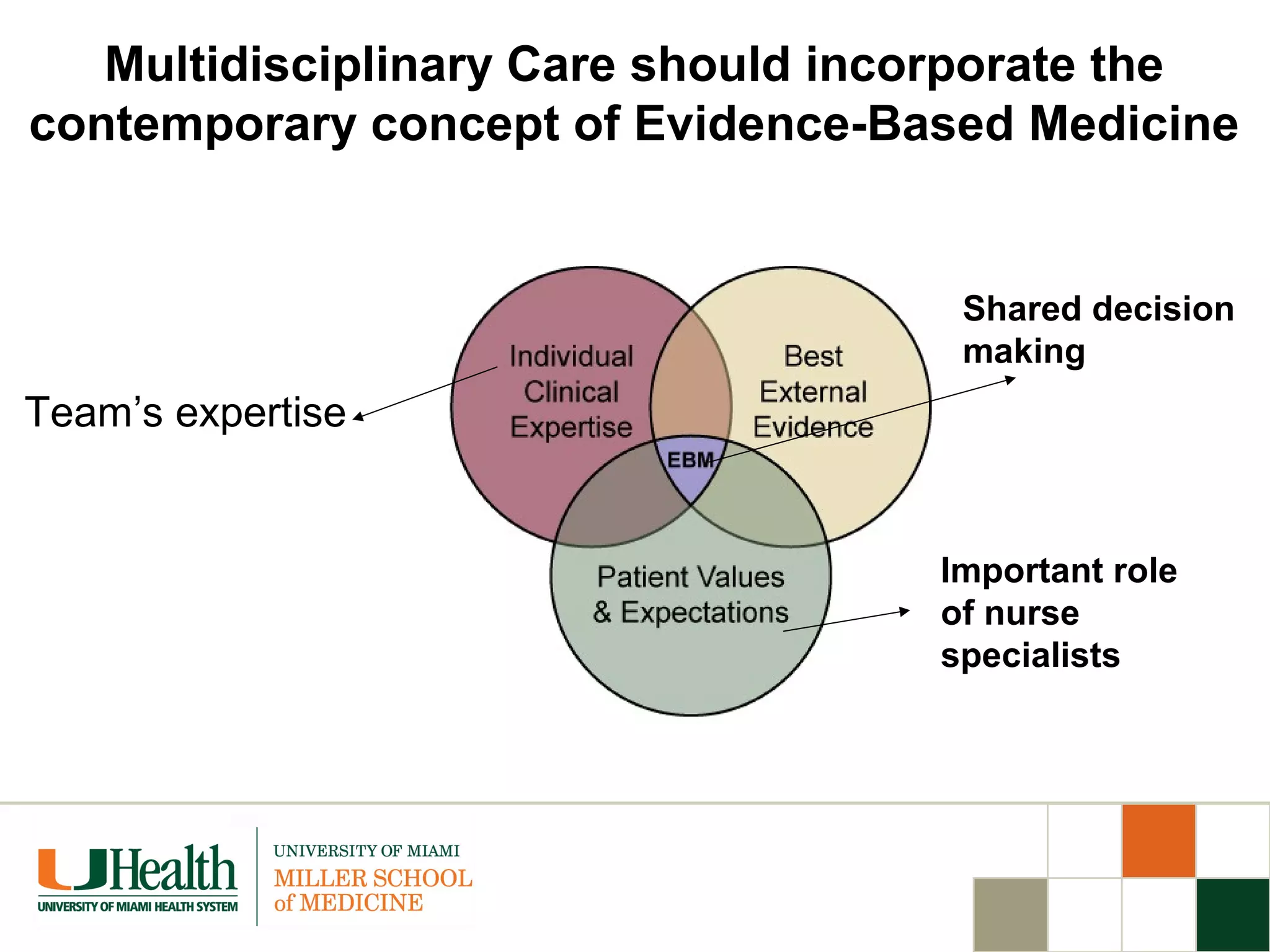
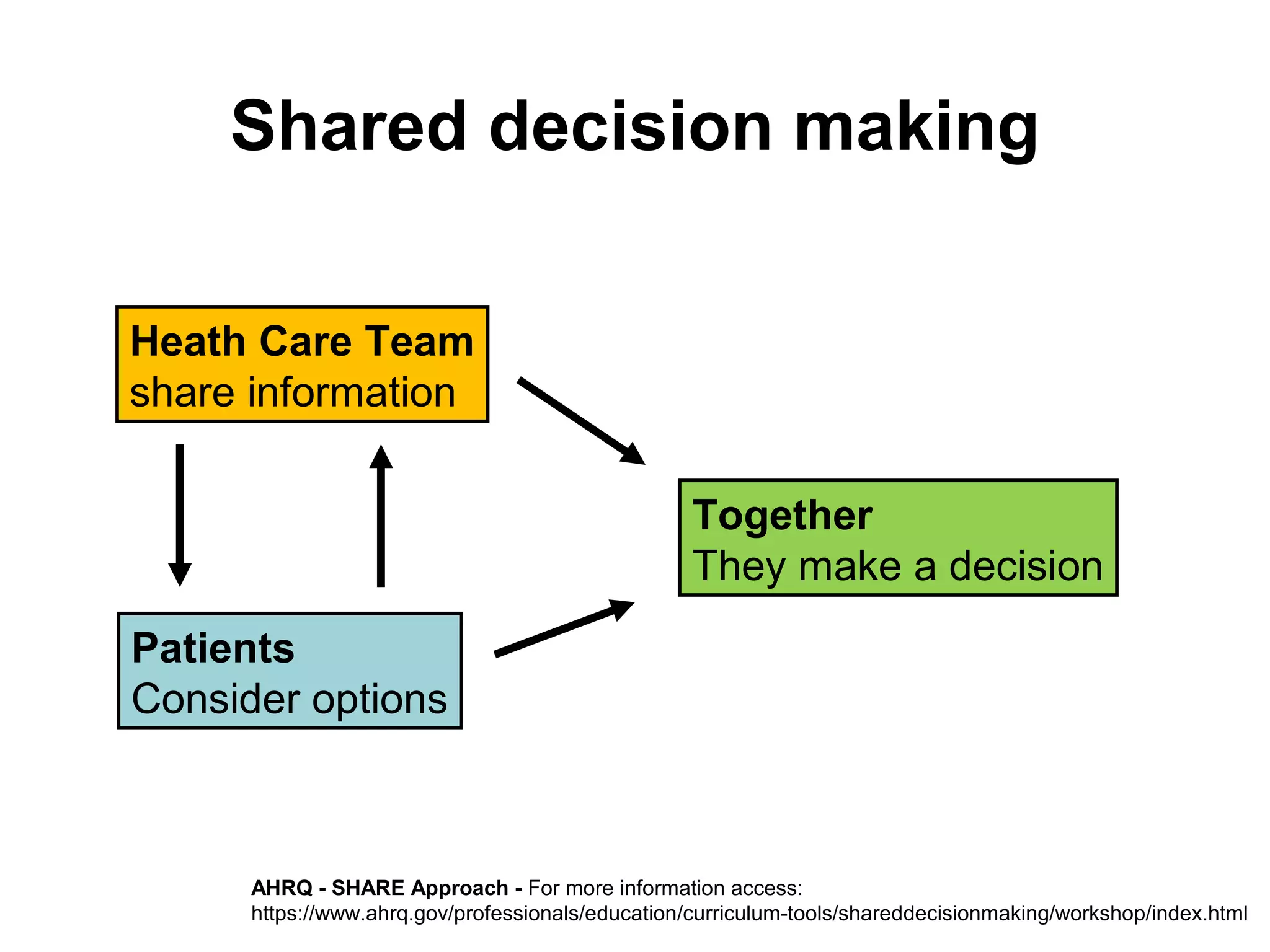
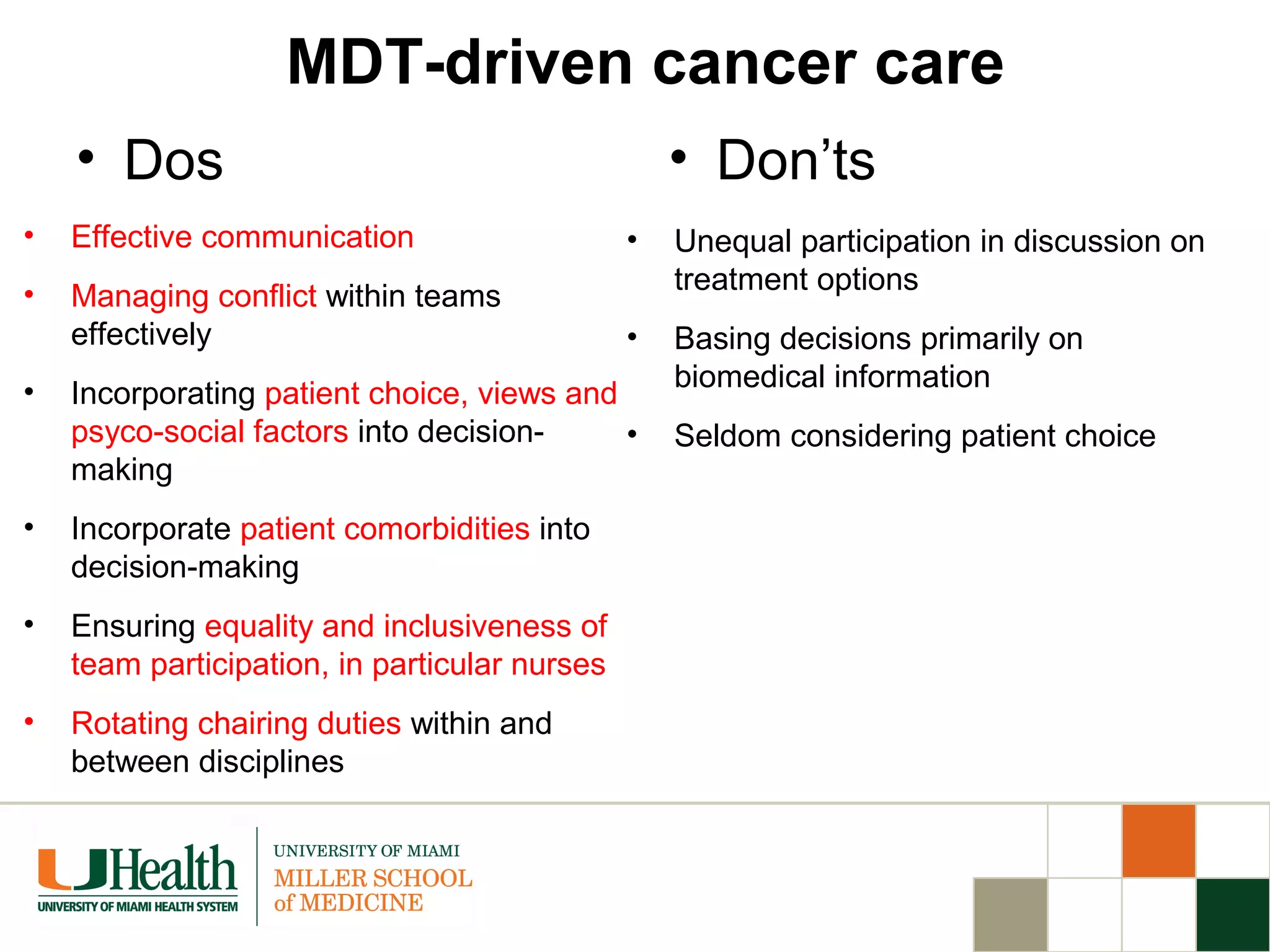
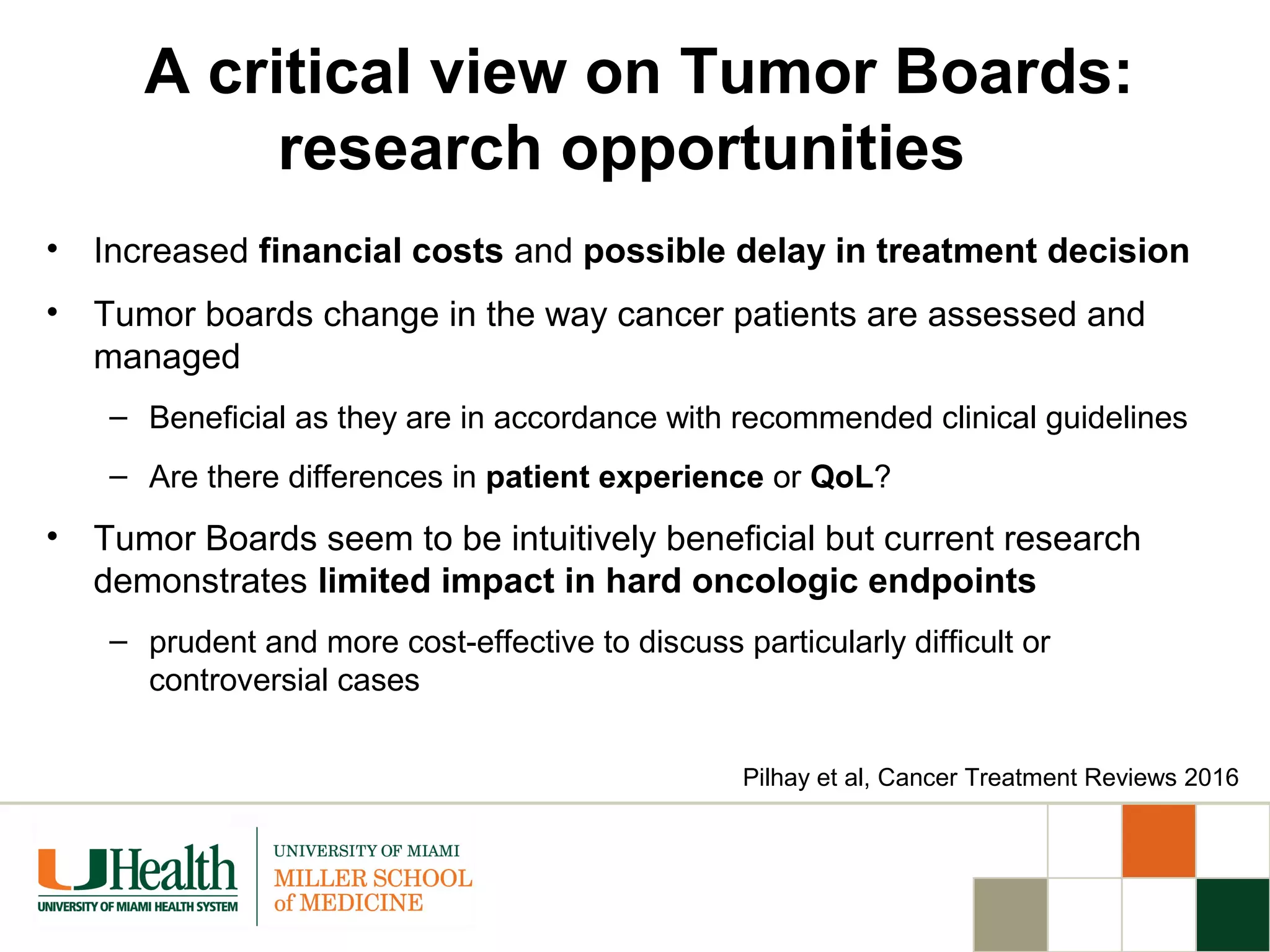
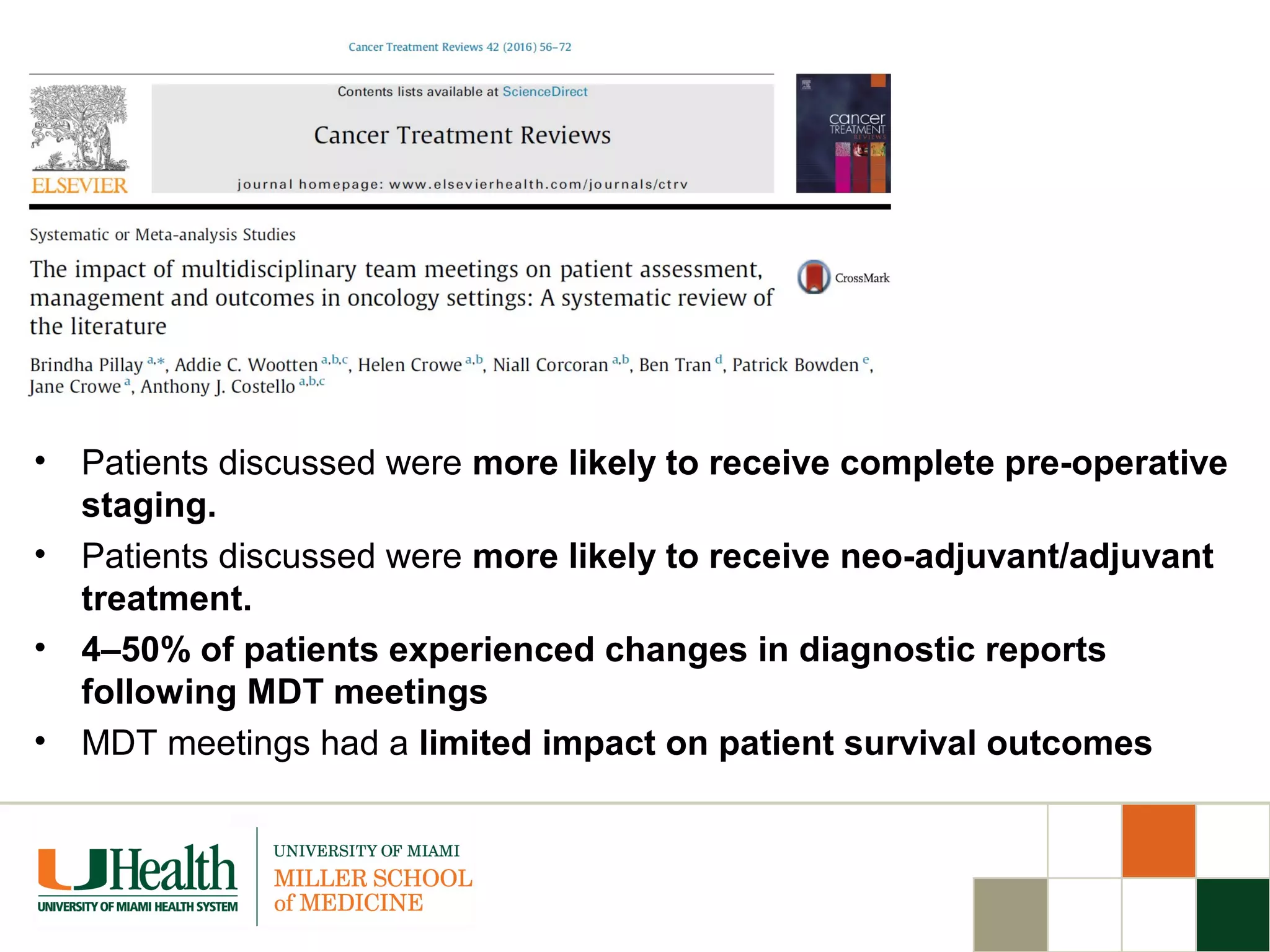
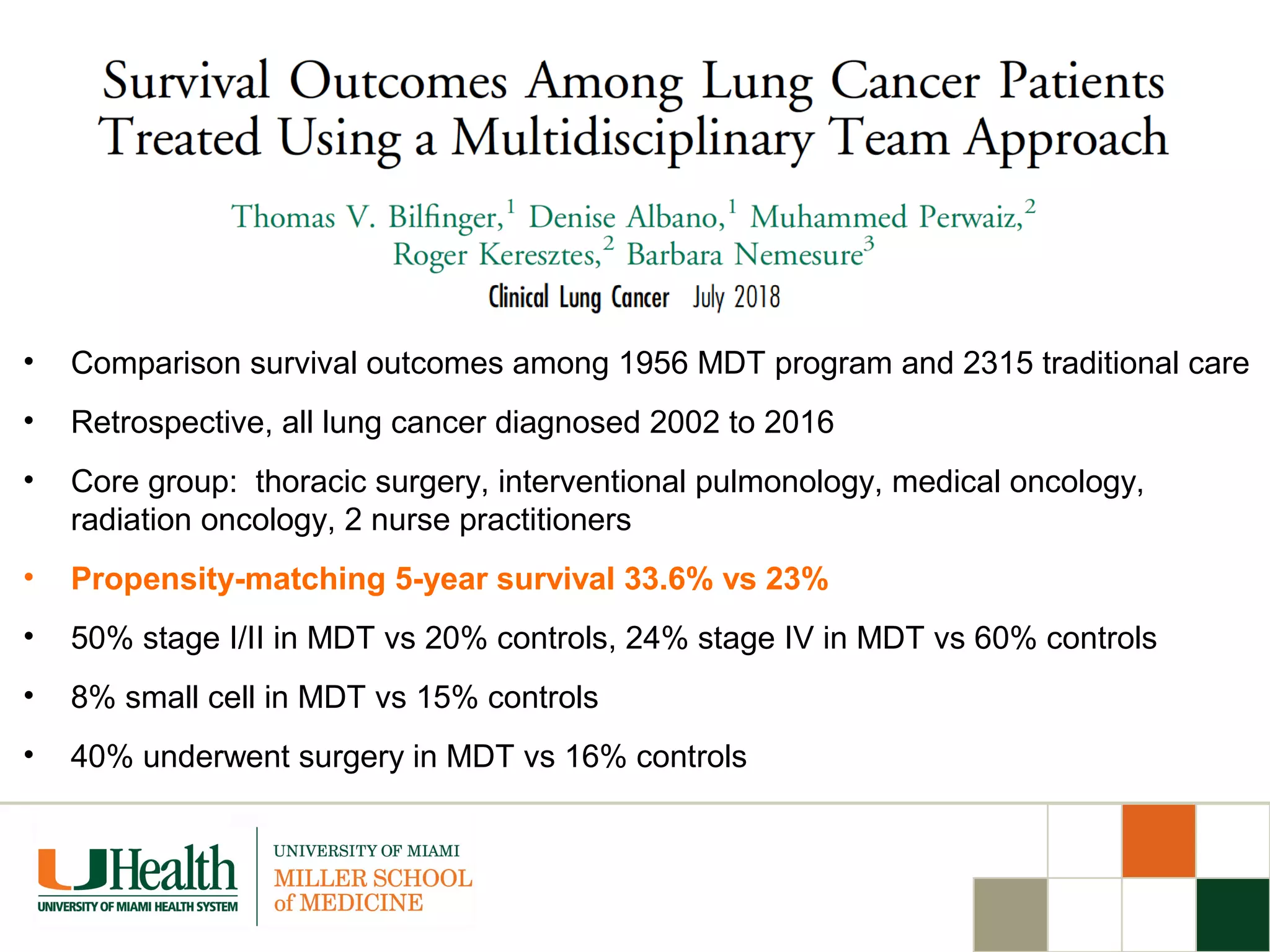
The document outlines the importance of the multidisciplinary team (MDT) approach in cancer treatment, particularly for lung cancer, highlighting the complexity and challenges of current care models. It emphasizes that MDTs improve patient outcomes through better communication, timely care, and collaboration among various specialists. However, it also points out barriers to widespread implementation of MDT care, including financial disincentives and resistance from providers.