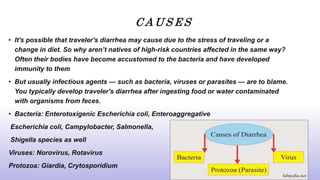
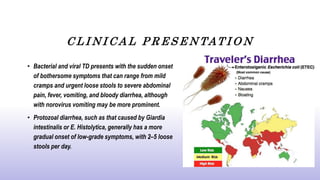
Traveler's diarrhea (TD) is a digestive disorder characterized by loose stools and abdominal cramps, typically occurring within the first week of travel due to contaminated food or water. Symptoms can range from mild to severe, and while it usually resolves without treatment, hydration and specific medications may be necessary, especially in high-risk areas. Preventative measures include careful food and drink choices, and maintaining hygiene to reduce the risk of infection.