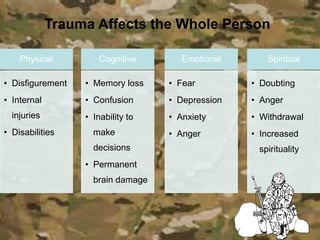
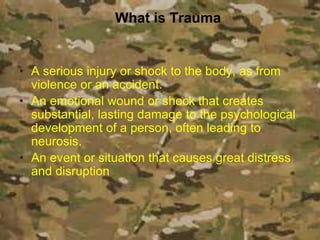
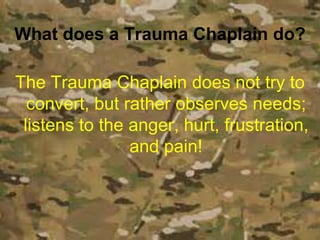
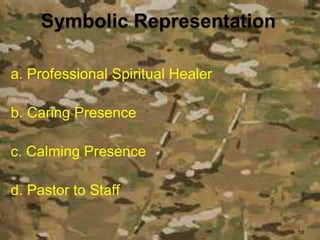
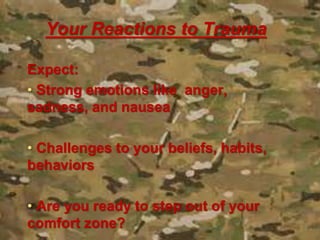
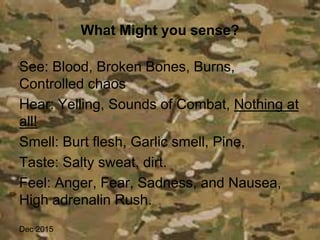
1. The video provides an overview of the role of a trauma chaplain in responding to mass casualty incidents and providing spiritual and emotional care. It discusses how trauma affects individuals physically, cognitively, emotionally, and spiritually.
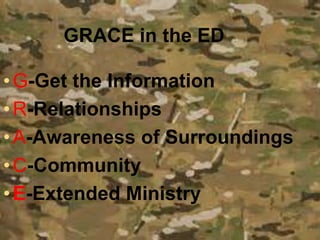
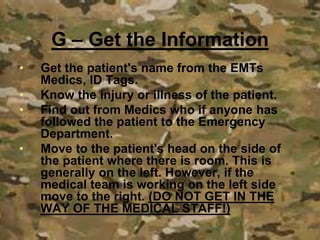
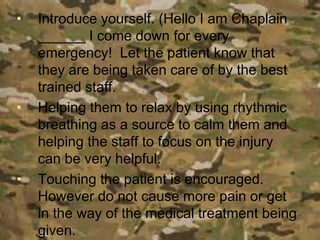
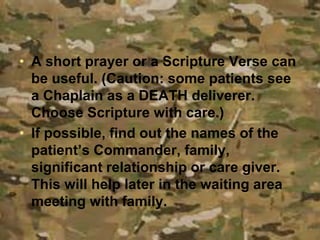
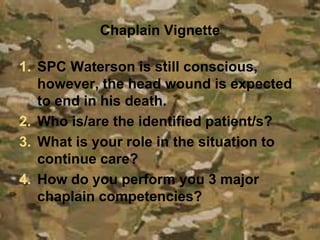
2. It outlines the GRACE model for trauma chaplaincy, which focuses on getting information, building relationships, maintaining awareness, supporting community, and providing extended ministry.
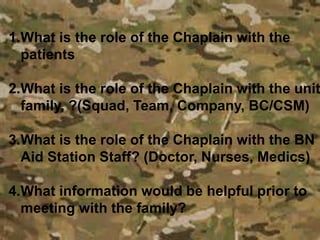
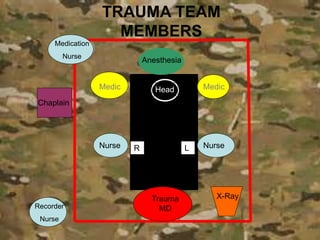
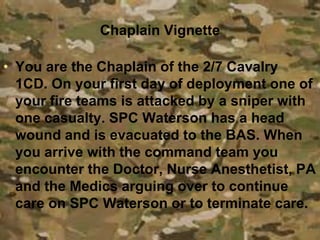
3. The video also includes a hypothetical scenario of a soldier sustaining a head wound and demonstrates how the chaplain might respond by providing presence, supporting medical decision making, and caring for the patient and their family.