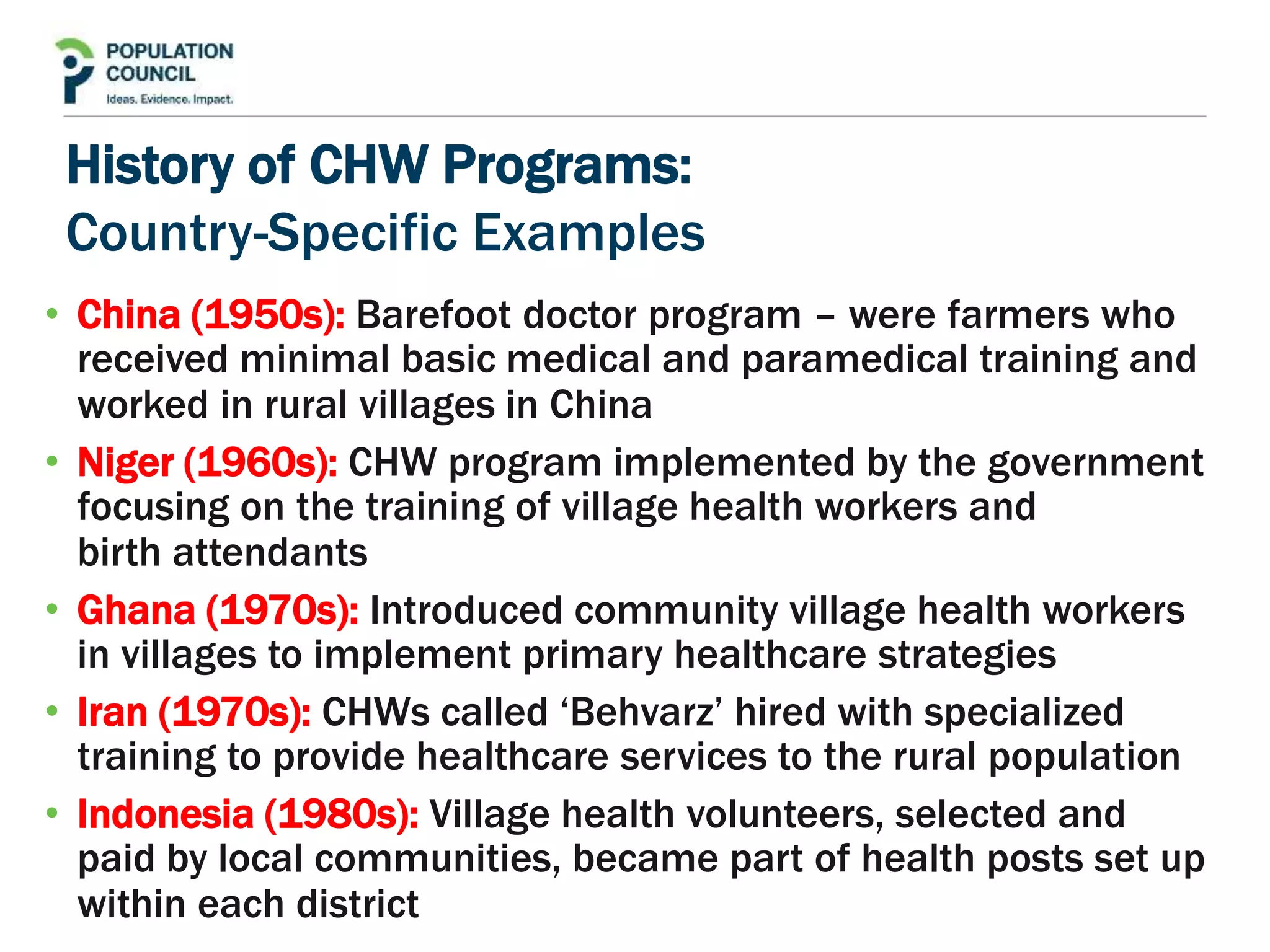
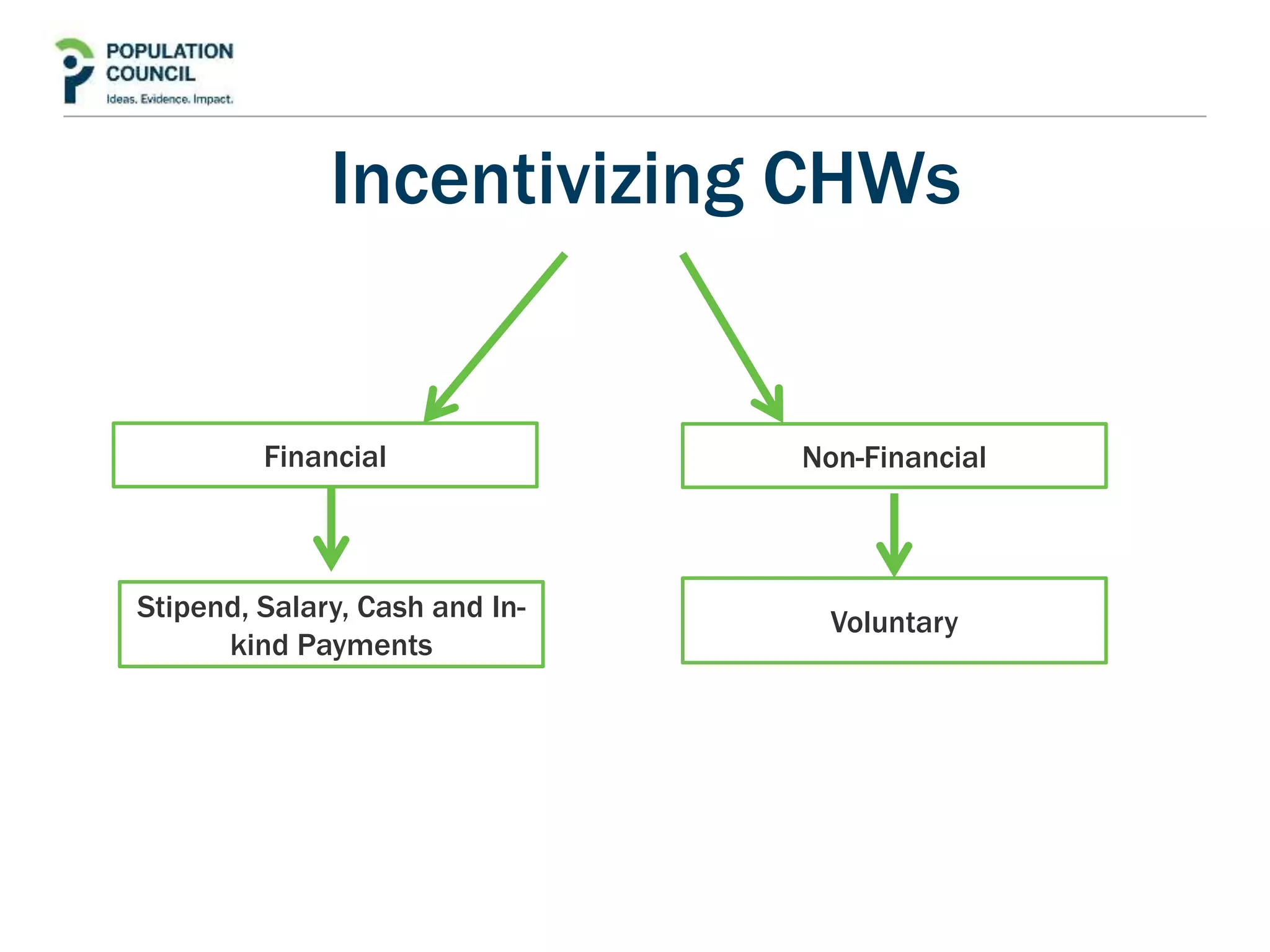
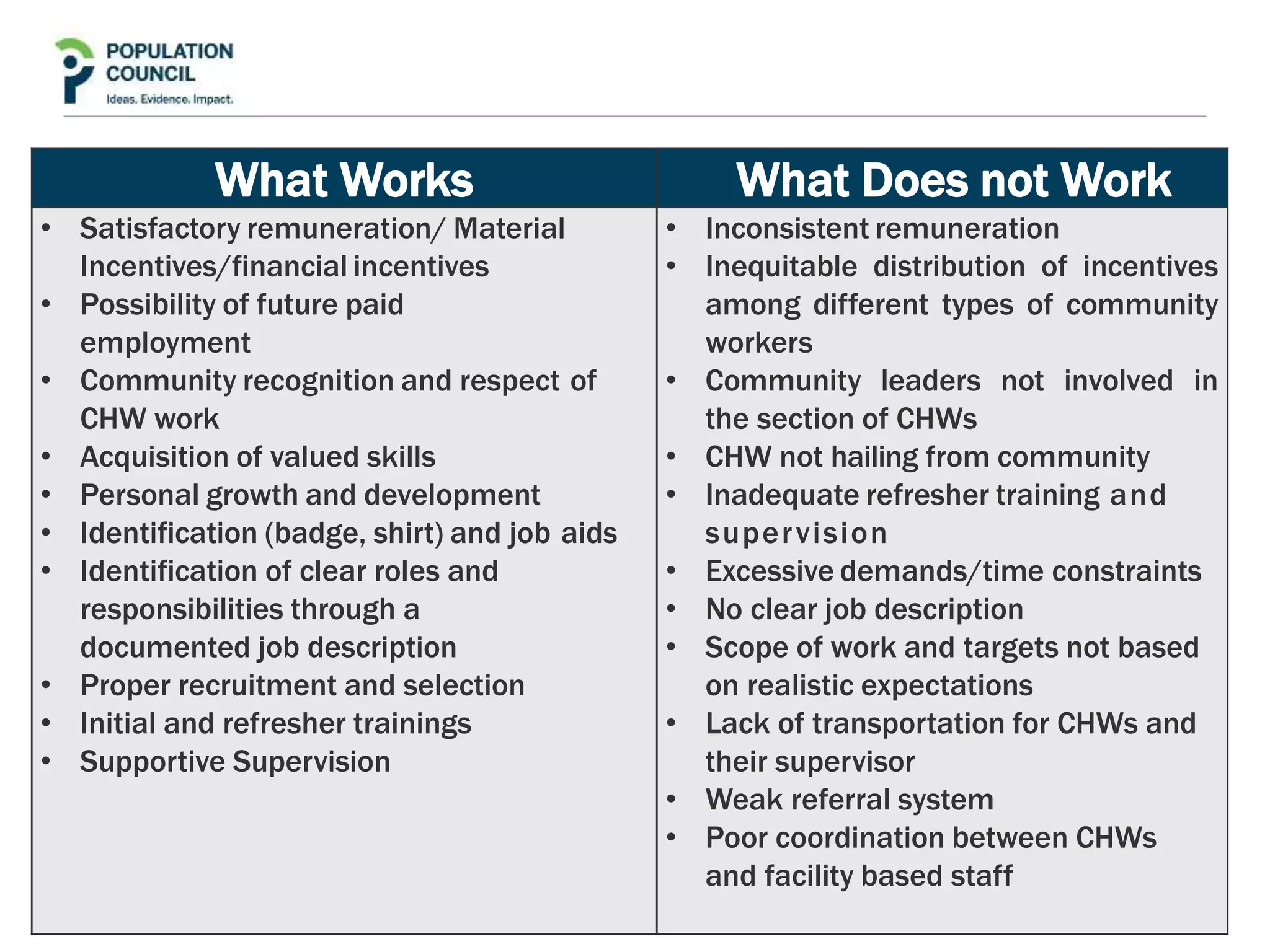
This document reviews the role of community health workers in delivering primary healthcare, particularly in resource-constrained settings. It defines community health workers as members of the communities they serve, selected by those communities to implement health interventions according to local norms. Globally there are approximately 1-5 million unpaid and paid community health workers. The review aims to identify strengths of community health worker programs, factors ensuring community acceptance and ownership, and factors relating to their effectiveness. It provides examples of successful community health worker programs from different countries and discusses incentives and factors that help or hinder community health workers. The document concludes by recommending Pakistan establish standards and integrate community health workers into its provincial health strategy to expand healthcare access.