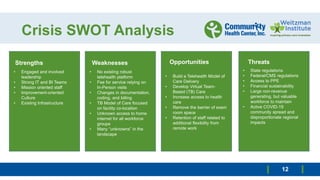
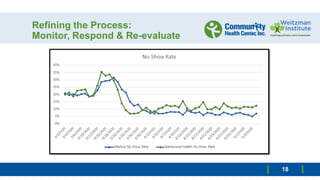
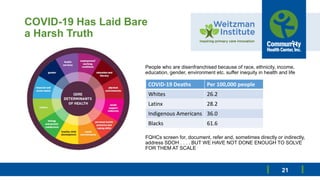
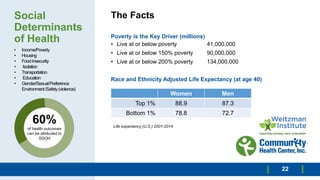
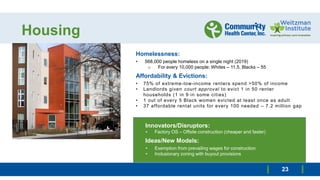
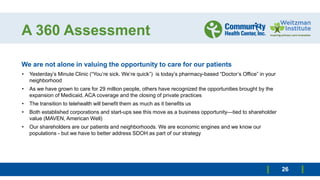
A health care organization laid out plans to reform its delivery system in response to the COVID-19 pandemic. It formed four teams to 1) assess the current crisis delivery model, 2) understand changes in the communities served, 3) develop a new delivery model, and 4) share lessons learned. The organization highlighted gaps in care for underserved groups and a need for more equitable access. It discussed strategies like telehealth, addressing social determinants of health, workforce flexibility, and collaborating with other organizations to build a sustainable system focused on community empowerment and improved outcomes.