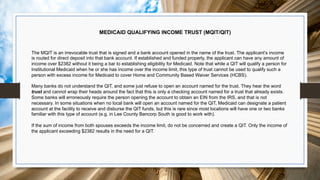
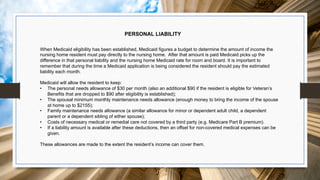
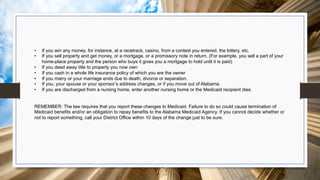
The document outlines the Medicaid application process for institutional coverage in Alabama, addressing eligibility considerations such as medical and financial criteria. It emphasizes the complexities of arranging nursing home placements, the importance of proper documentation, and the need for legal authority when completing applications. Additionally, it highlights important distinctions between Medicaid and Medicare coverage and the financial impact of nursing home expenses, providing resources and guidelines for successful applications.