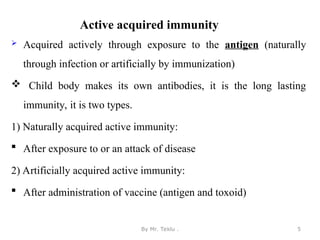
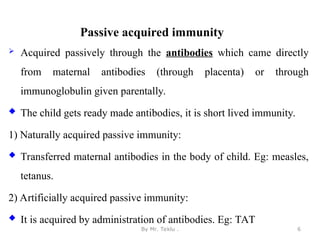
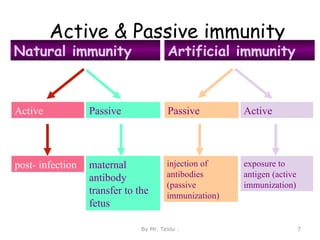
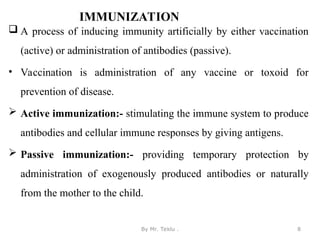
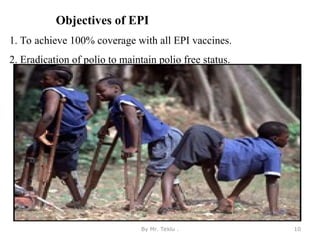
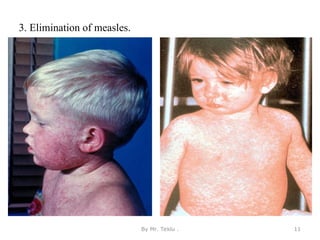
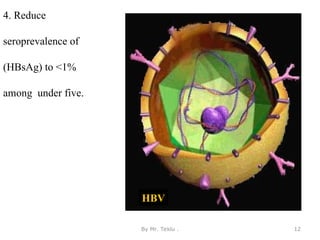
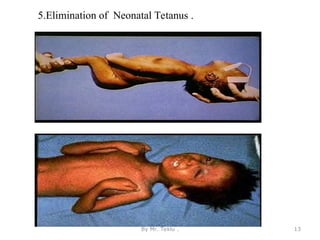
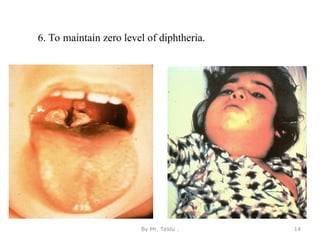
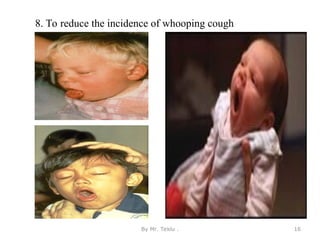
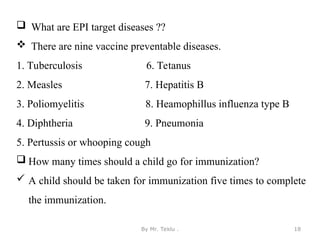
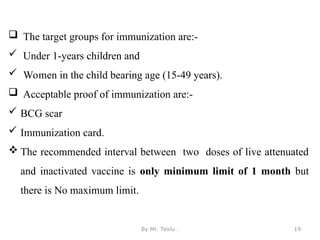
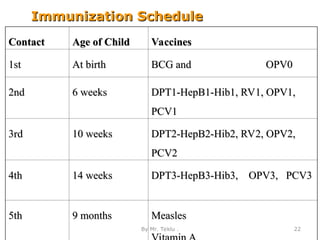
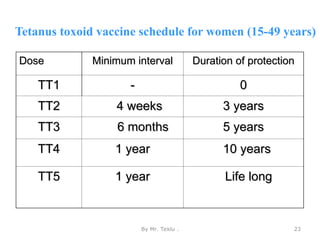
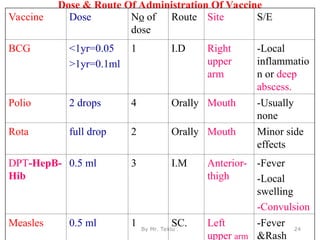
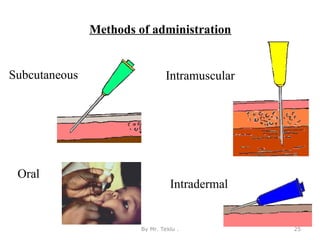
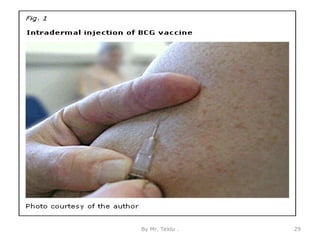
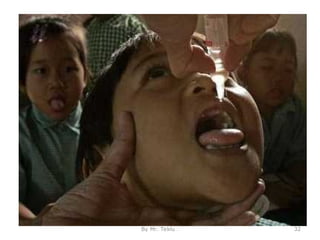
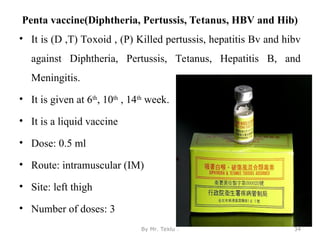
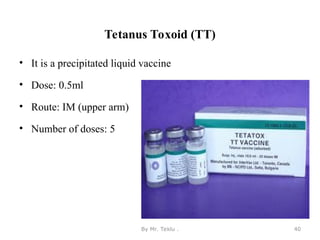
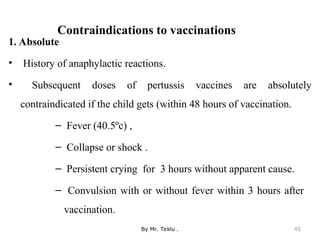
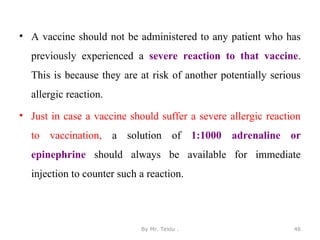
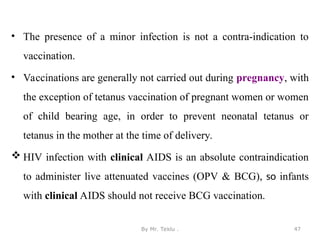
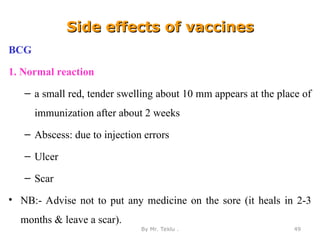
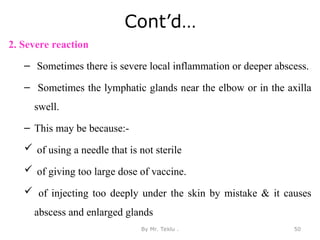
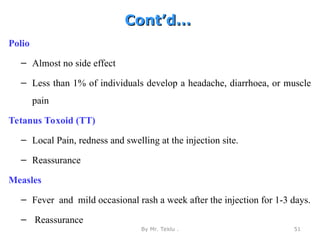
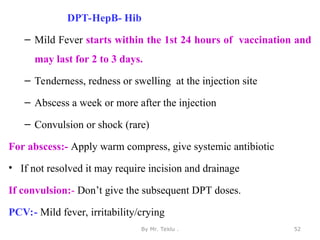
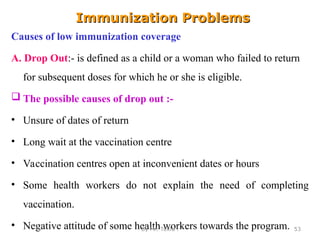
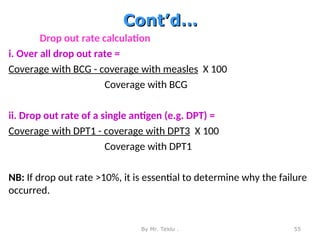
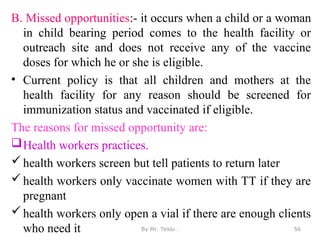
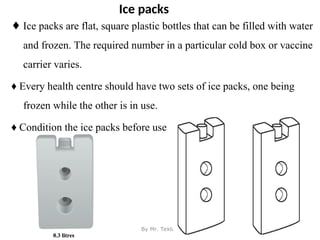
The document outlines the Expanded Program on Immunization (EPI), which aims to provide vaccines to all children under the age of one to prevent diseases and reduce child mortality. It explains types of immunity, immunization strategies, vaccination schedules, vaccine types, and specific vaccines for various diseases. Additionally, it addresses challenges in immunization coverage, such as dropouts and missed opportunities, and proposes solutions to improve immunization rates.