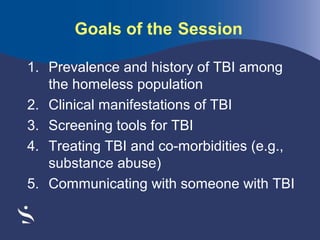
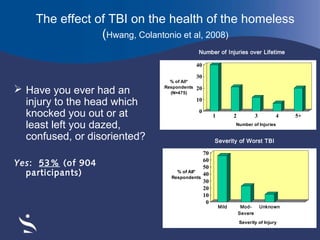
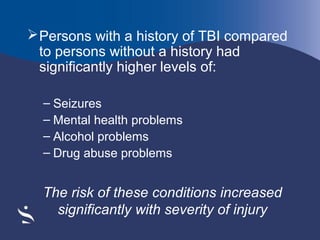
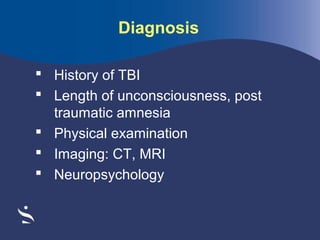
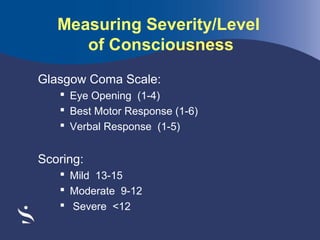
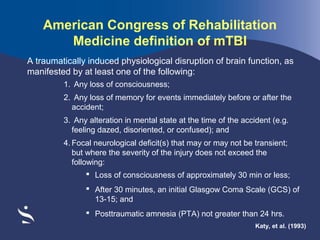
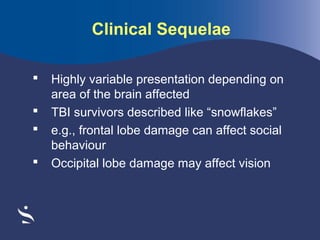
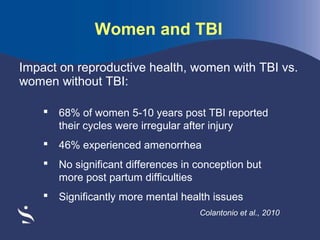
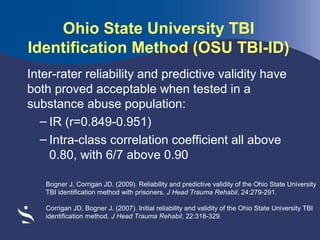
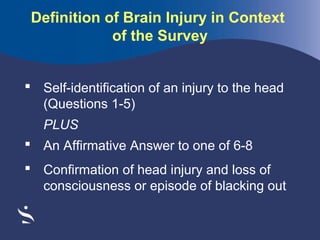
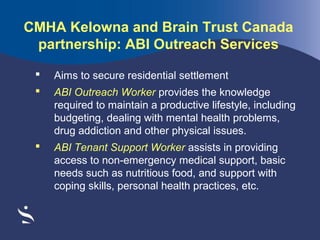
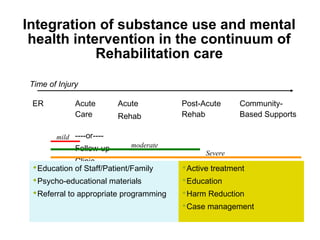
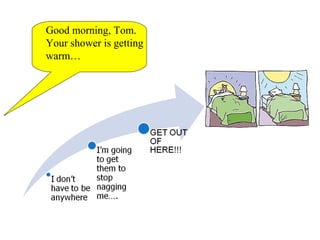
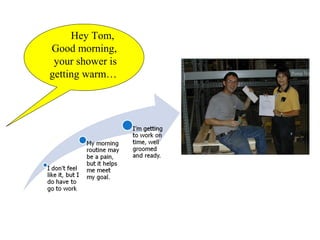
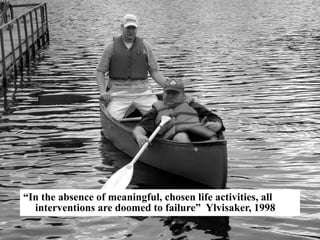
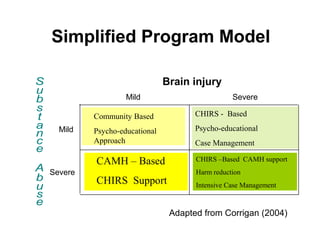
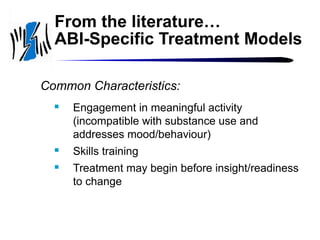
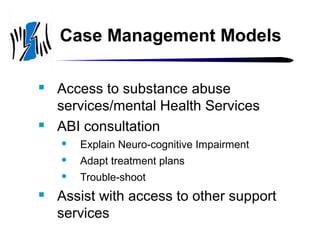
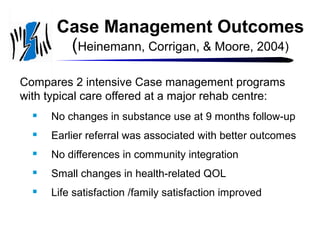
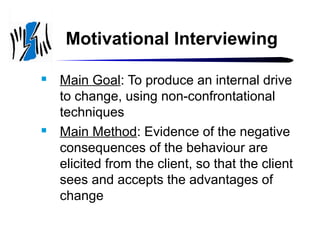
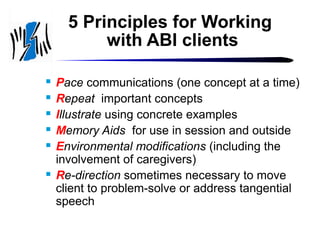
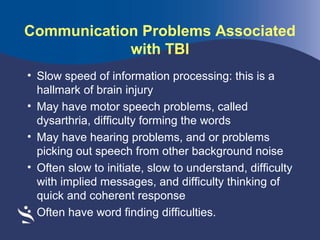
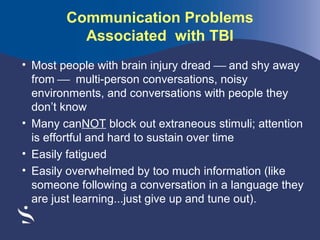
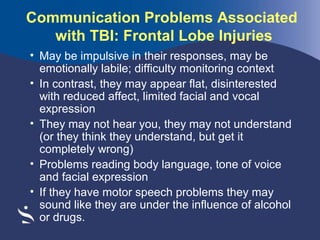
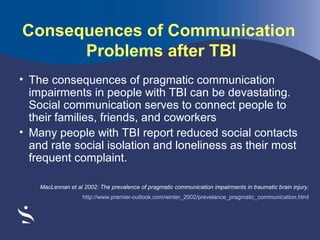
The document discusses diagnosis and treatment of traumatic brain injury (TBI). It begins by introducing the presenters, who are experts in acquired brain injury. They then discuss goals of the session, which include prevalence of TBI among the homeless population, clinical manifestations, screening tools, treating TBI and co-morbidities, and communicating with someone with TBI. The document provides information on defining and classifying TBI, diagnosing TBI through various methods, and treating TBI through multidisciplinary rehabilitation and a range of evidence-based approaches.