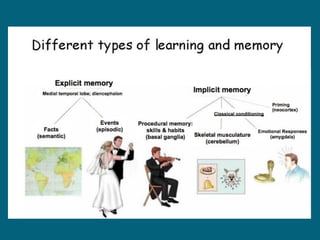
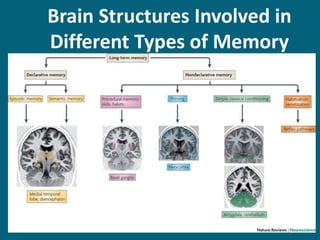
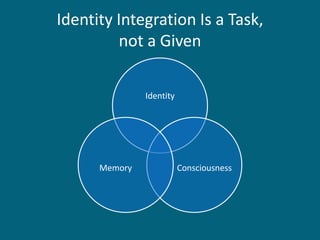
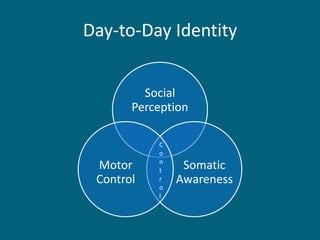
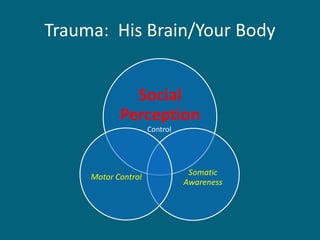
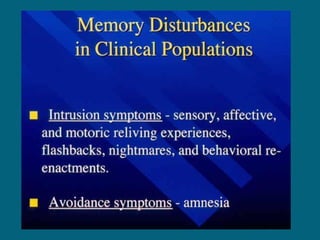
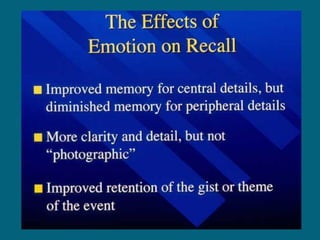
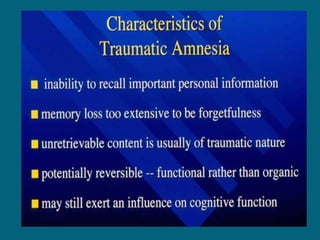
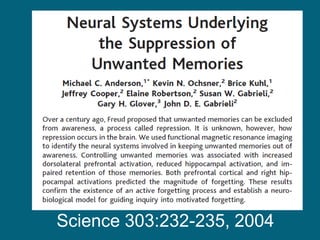
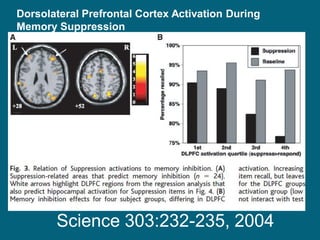
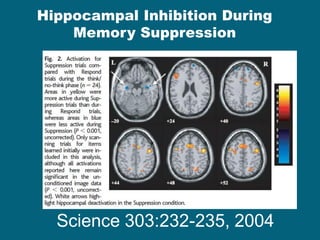
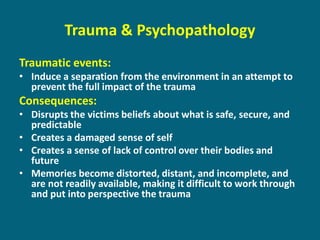
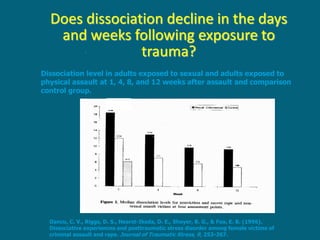
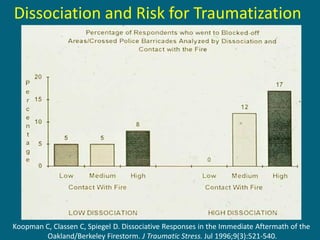
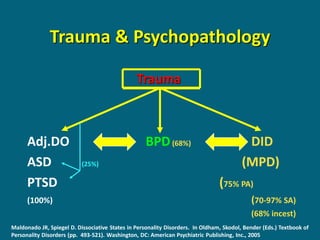
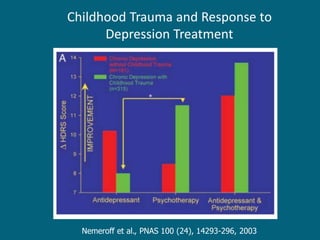
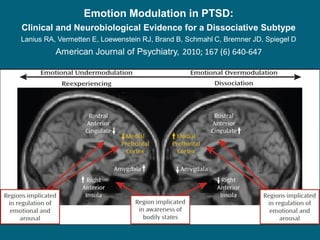
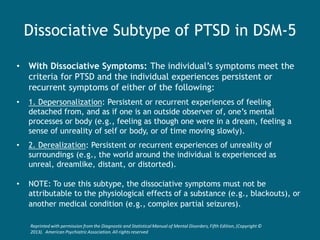
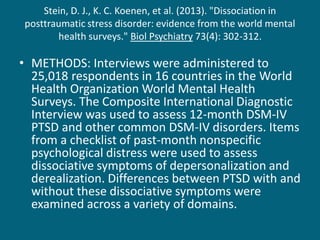
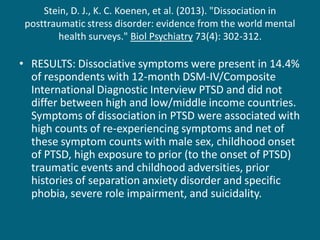
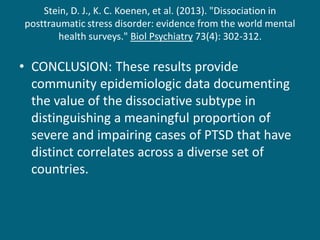
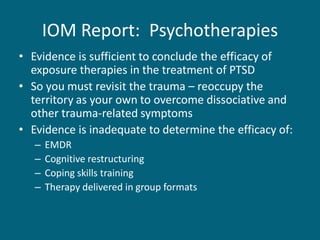
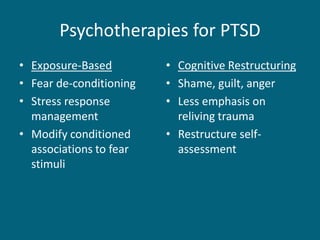
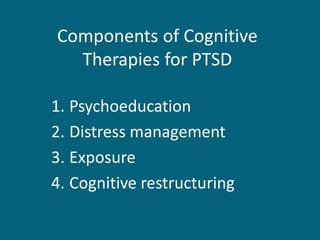
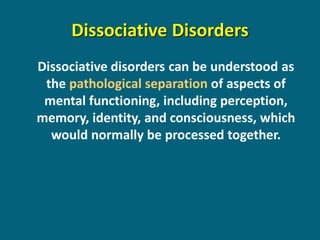
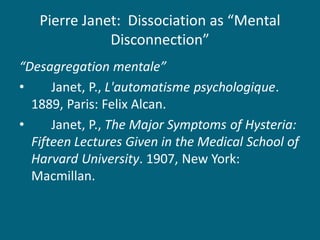
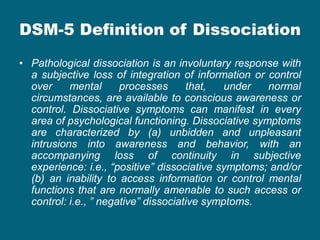
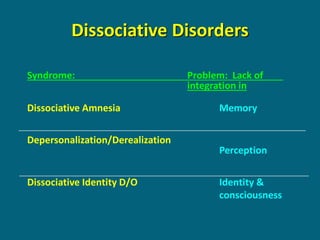
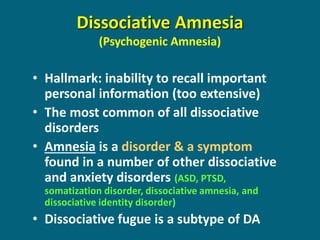
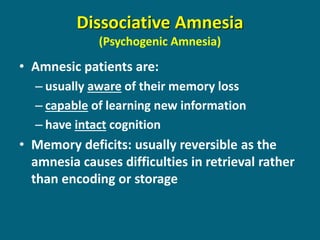
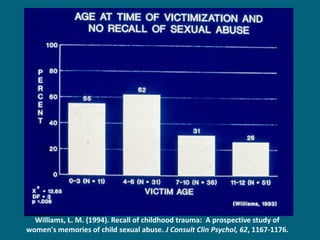
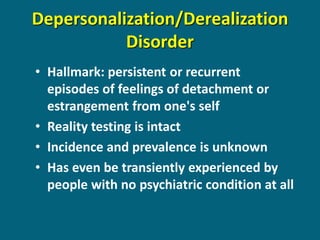
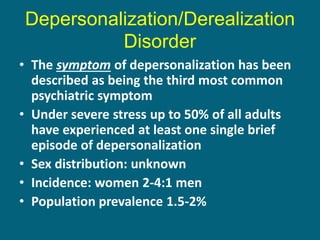
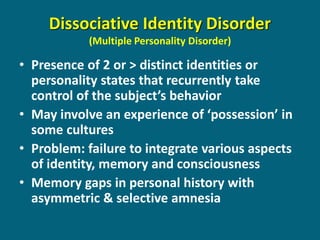
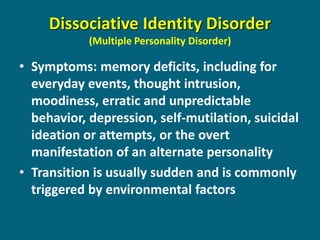
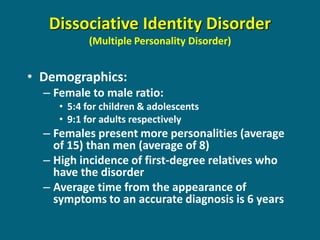
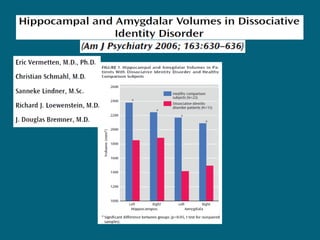
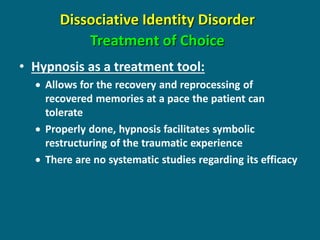
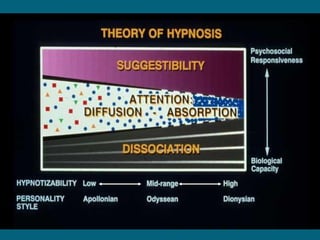
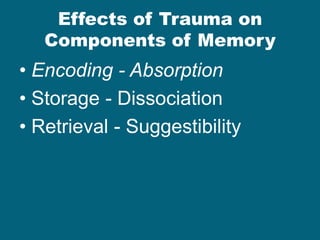
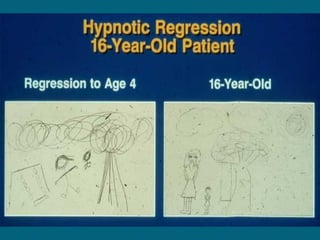
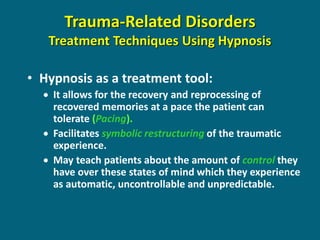
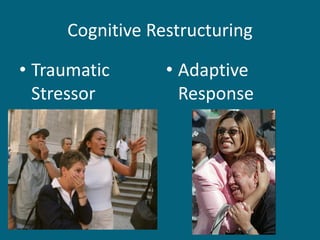
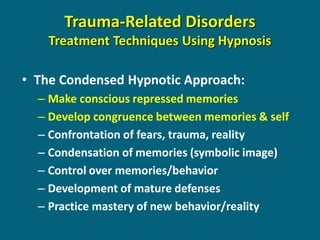
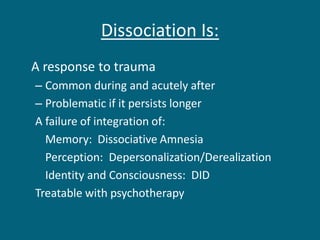
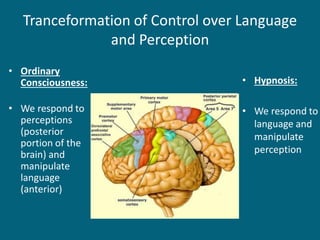
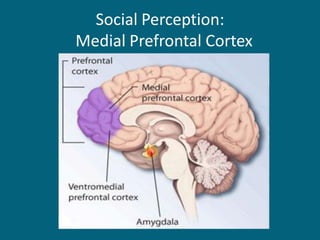
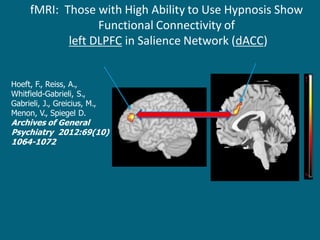
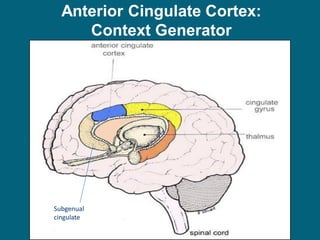
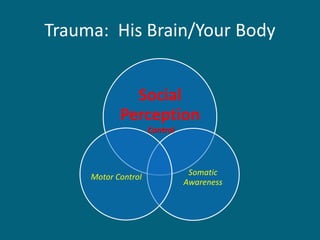
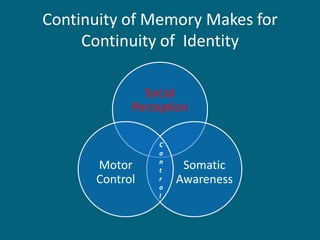
This document summarizes David Spiegel's work on memory, personal identity, trauma, and dissociation. It discusses how trauma can disrupt normal processing and force victims to reorganize mental processes. Dissociative defenses may be an adaptive response to overwhelming stress but also cause symptoms. The document reviews brain structures involved in memory, identity integration challenges after trauma, and treatments like exposure therapy to help process trauma memories and symptoms.