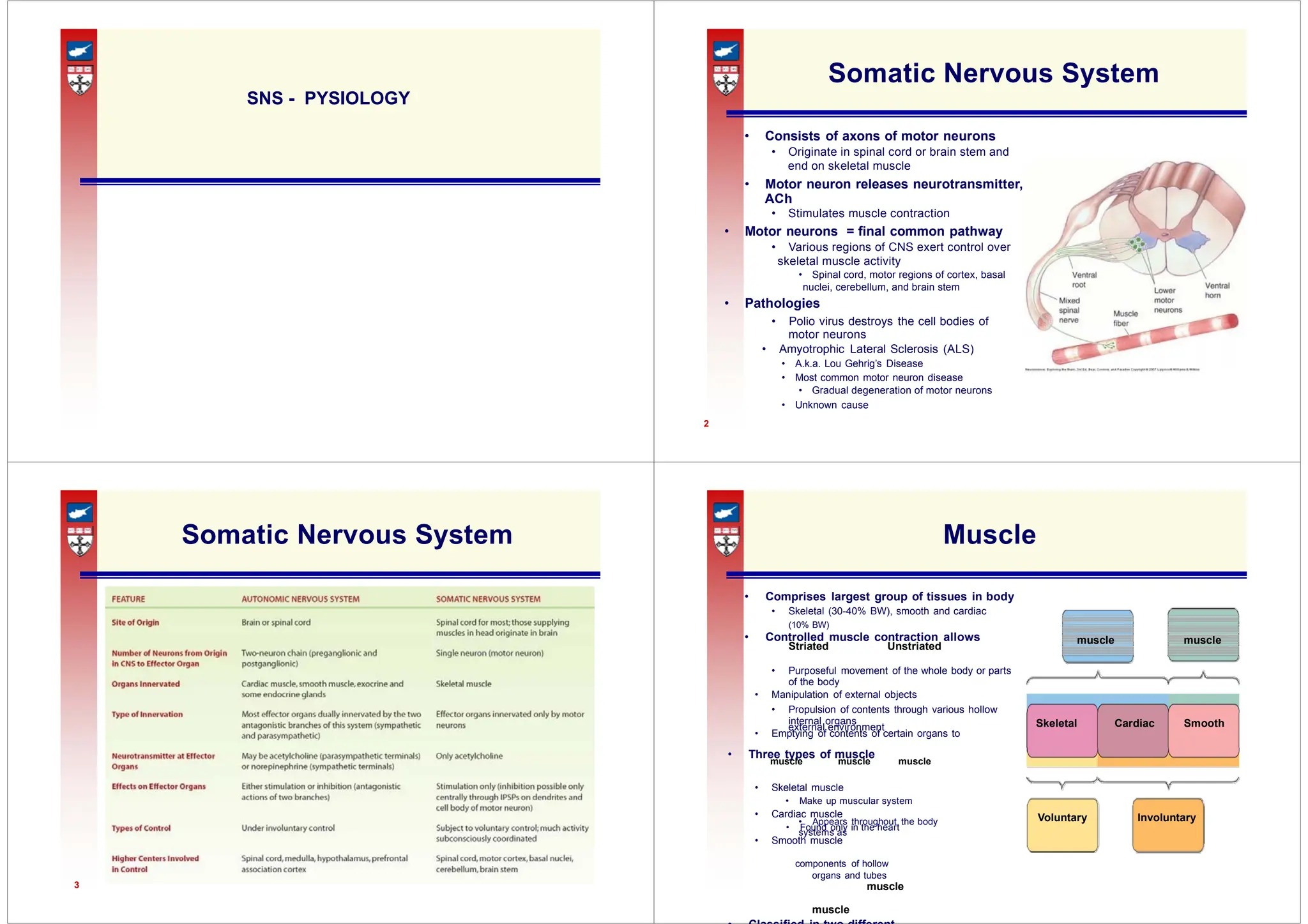
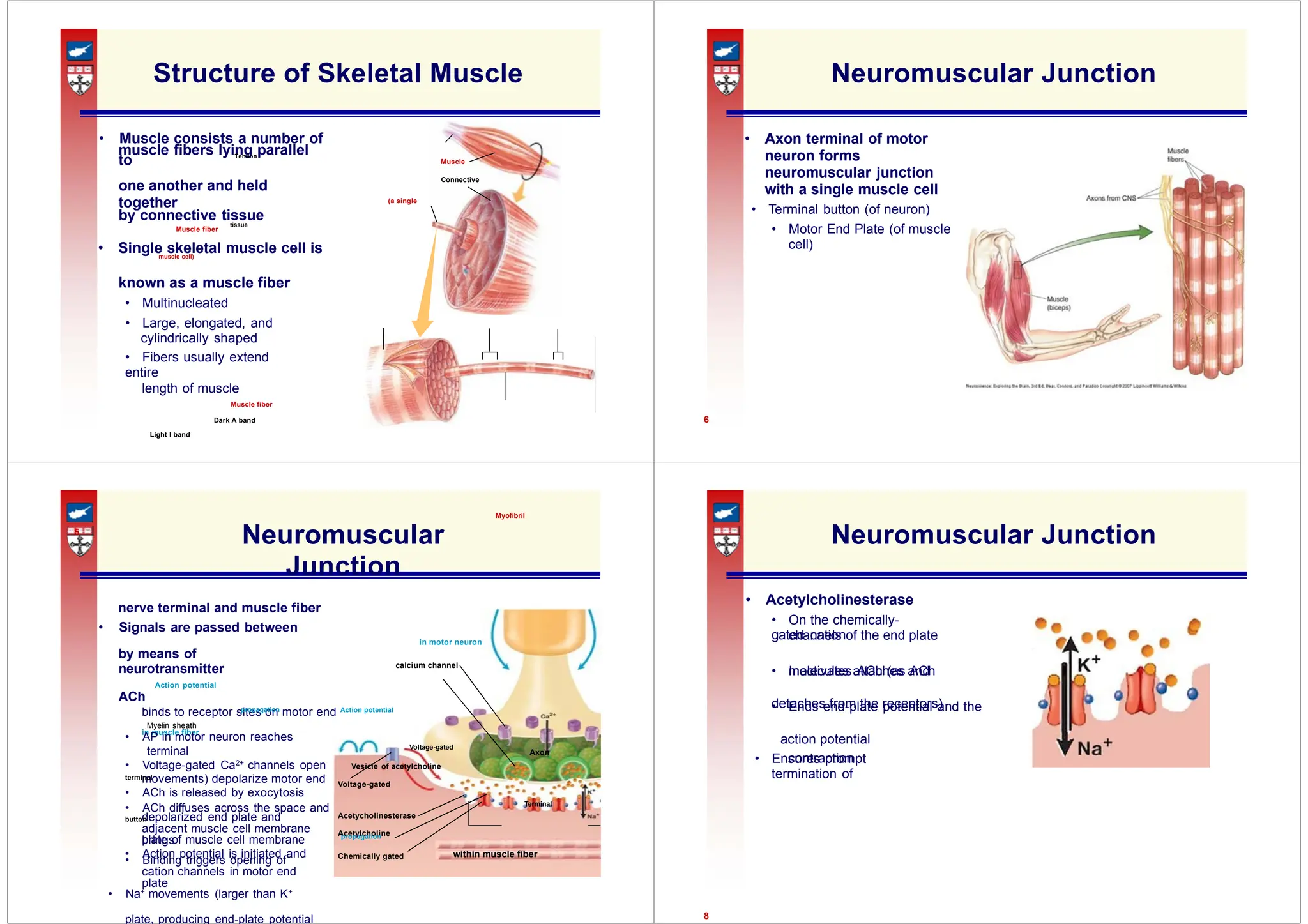
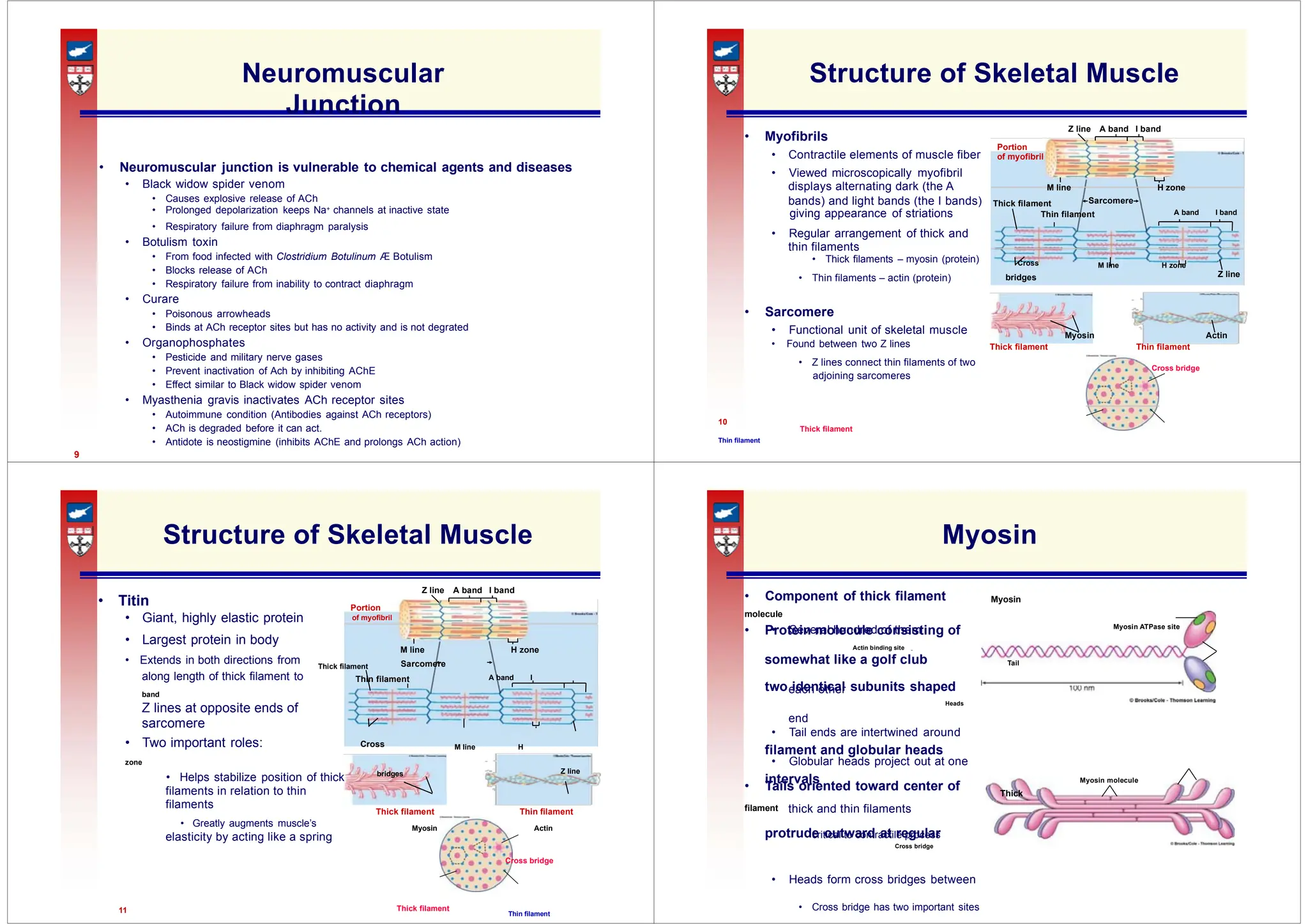
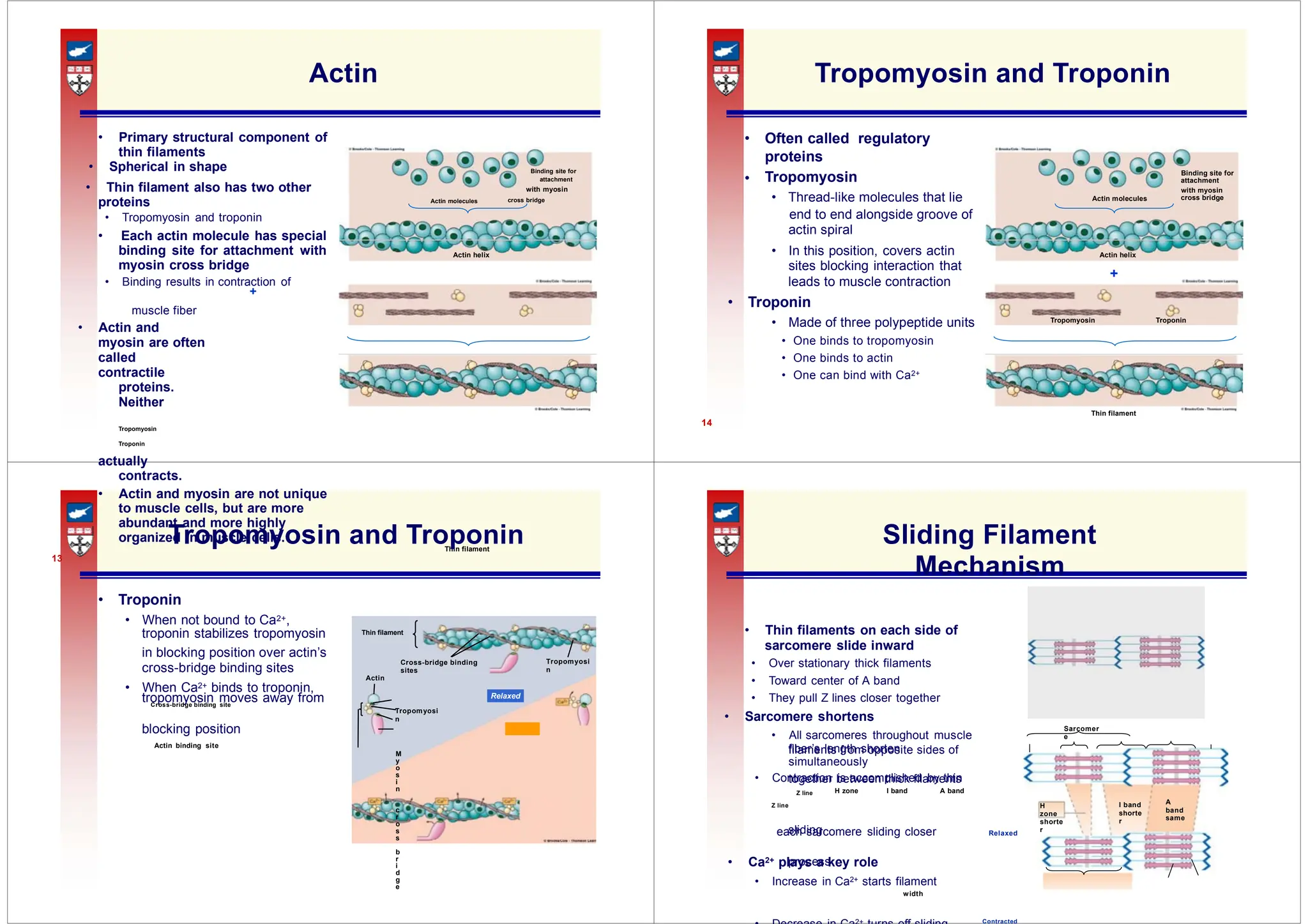
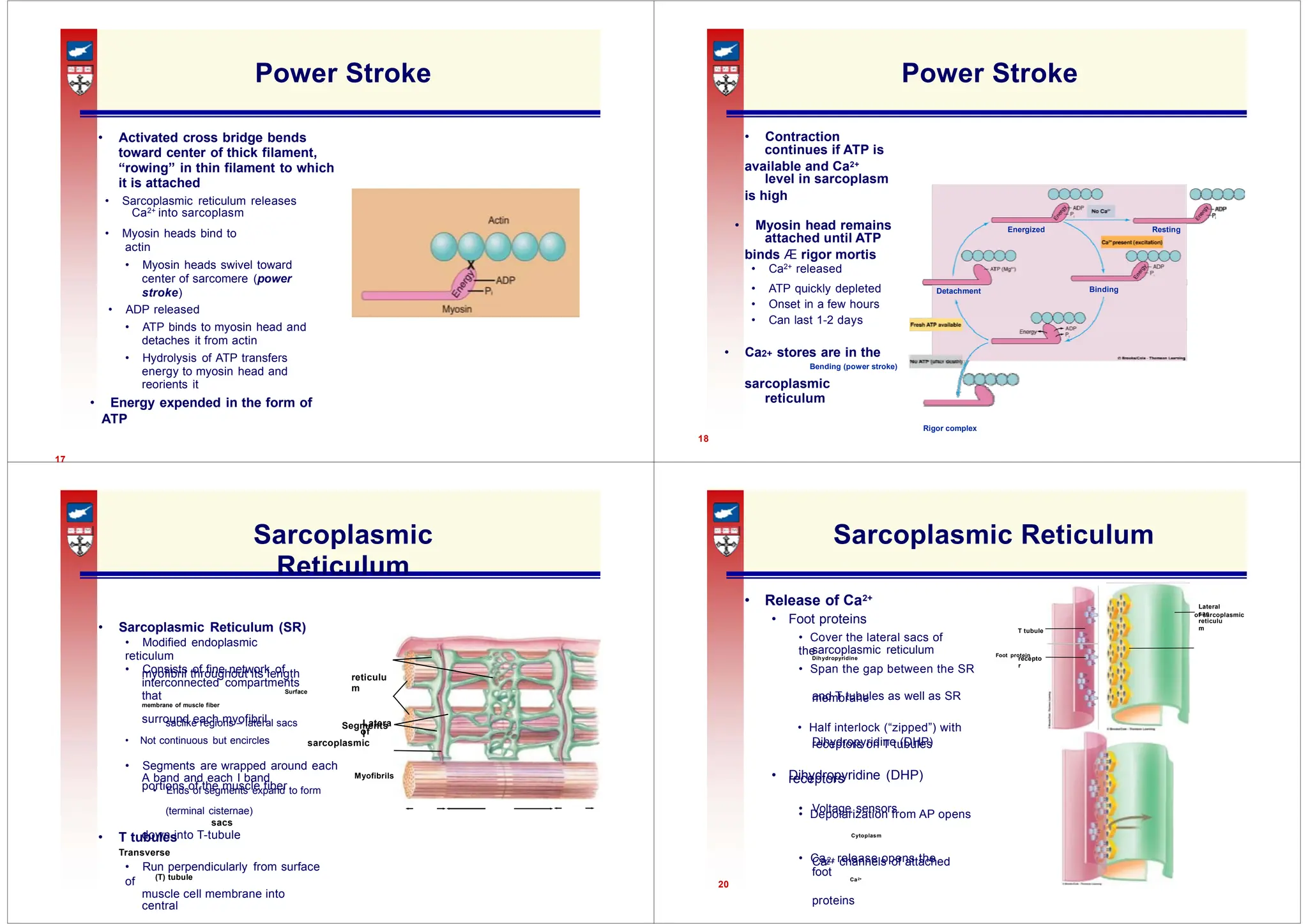
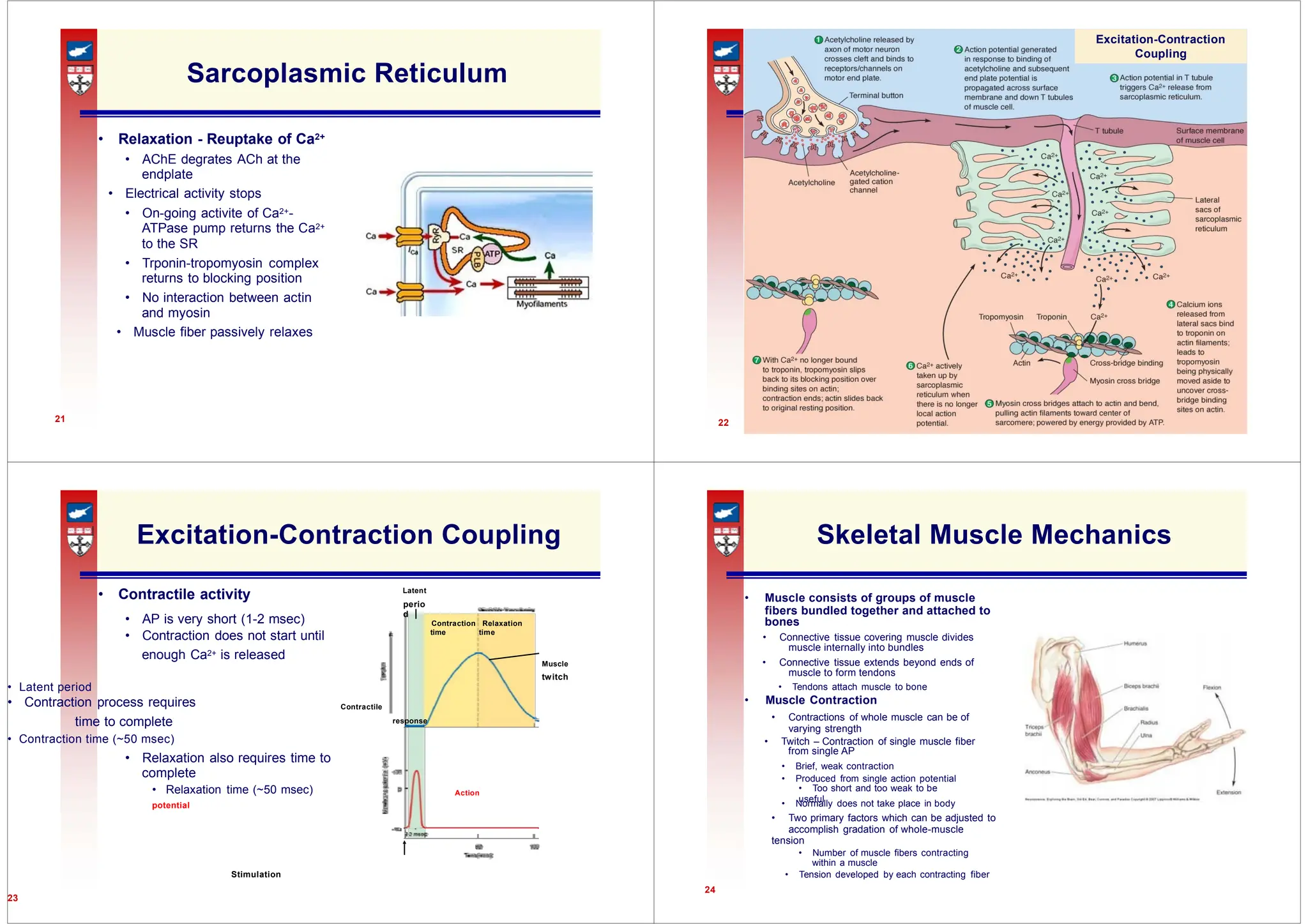
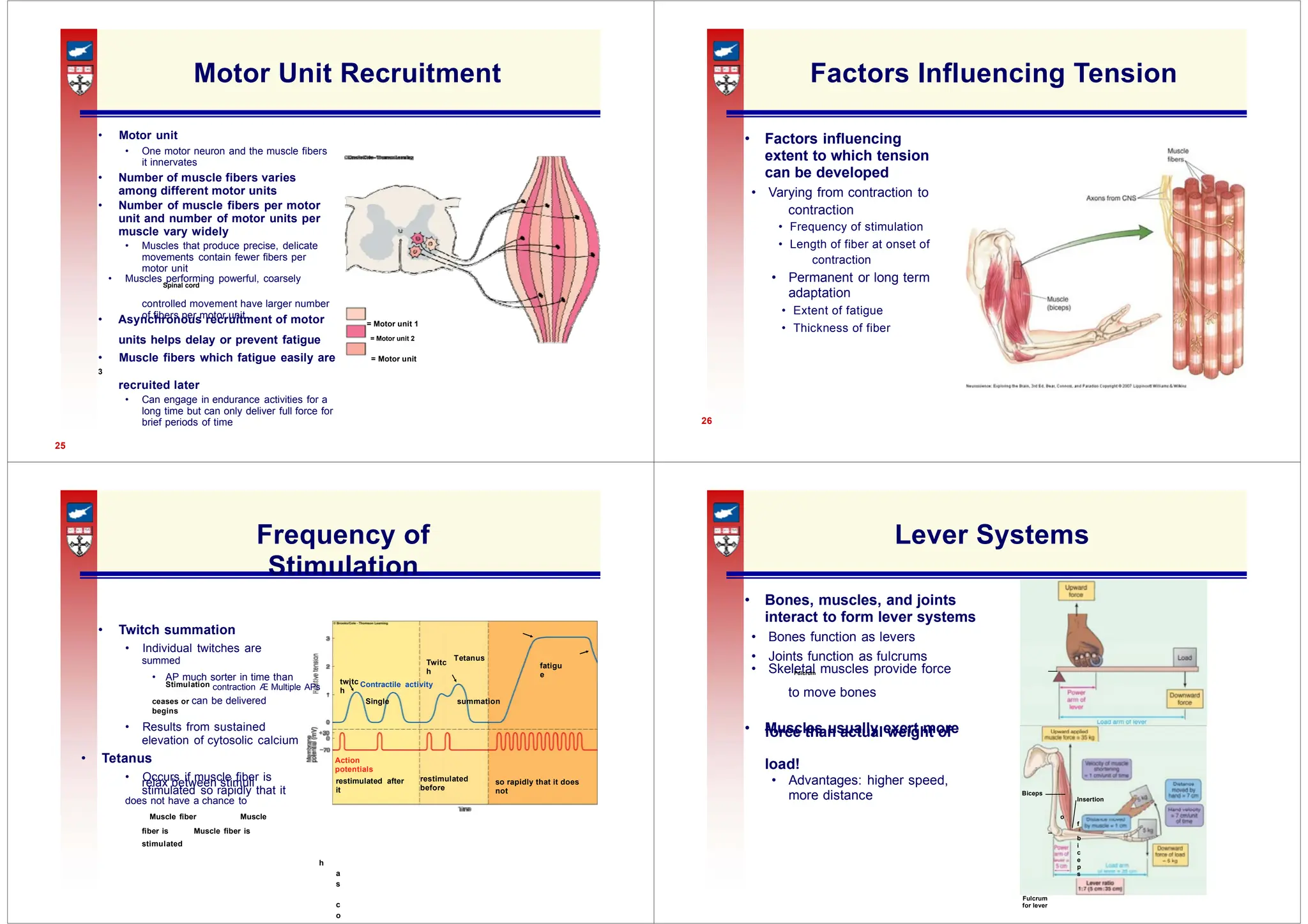
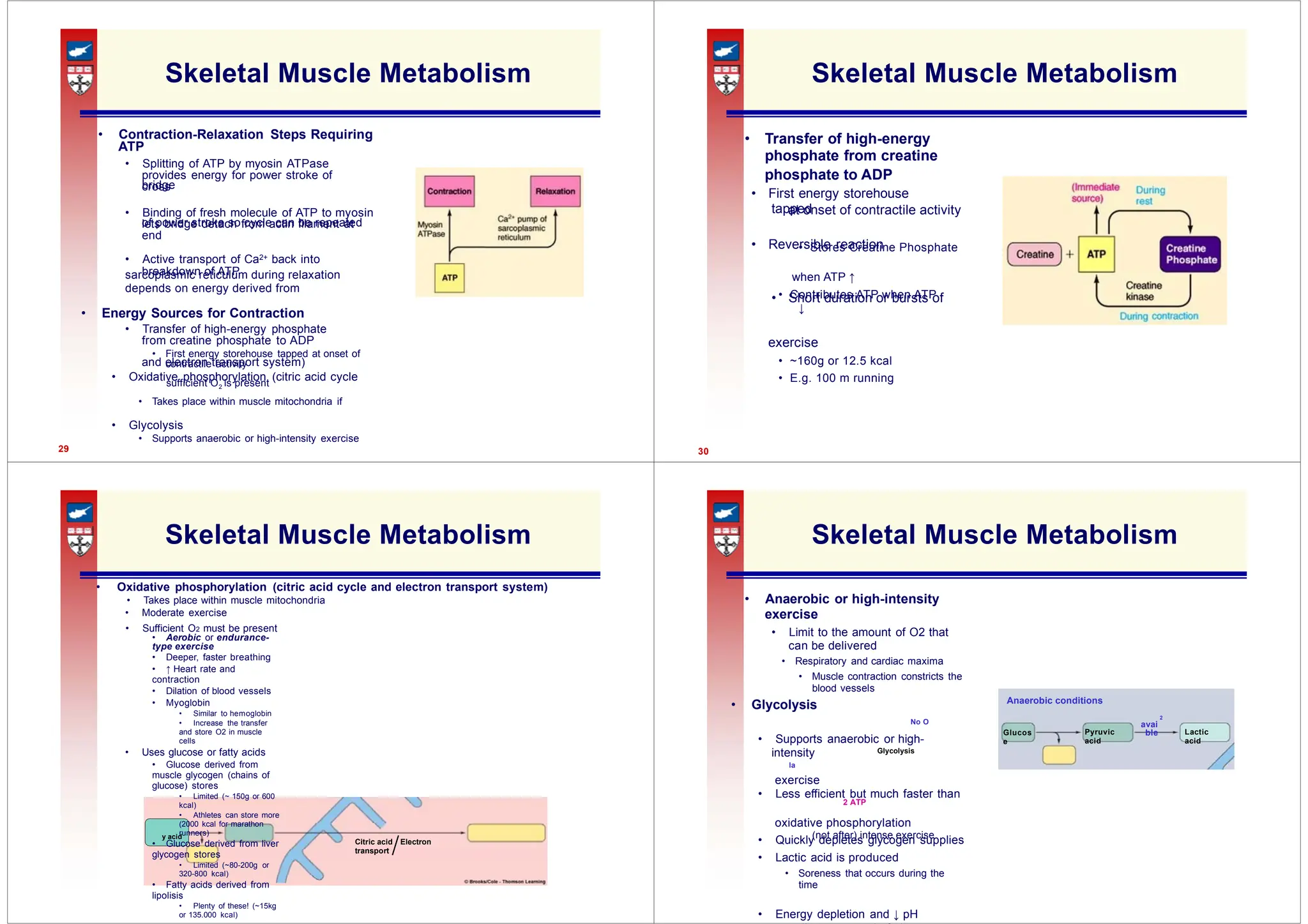
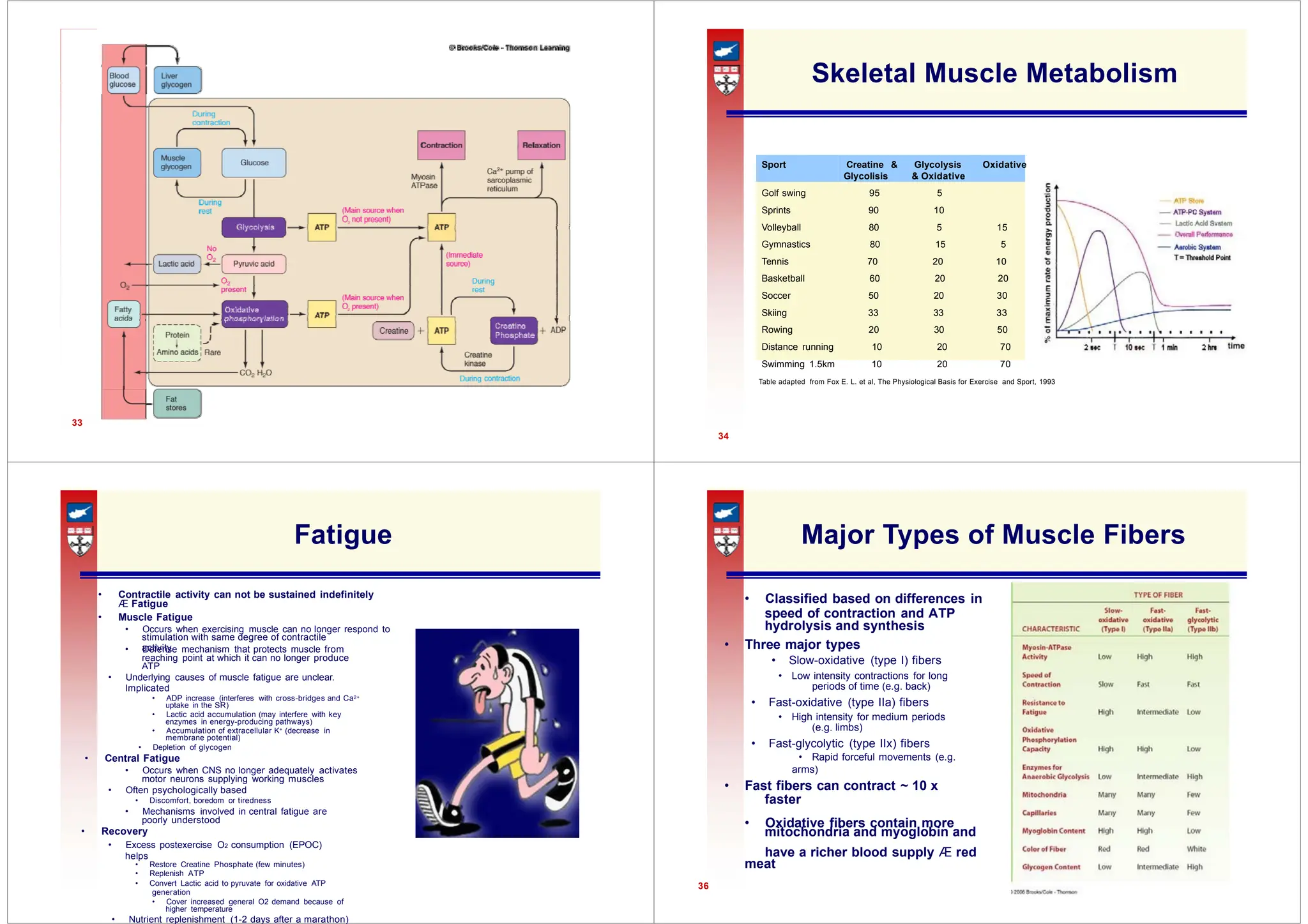
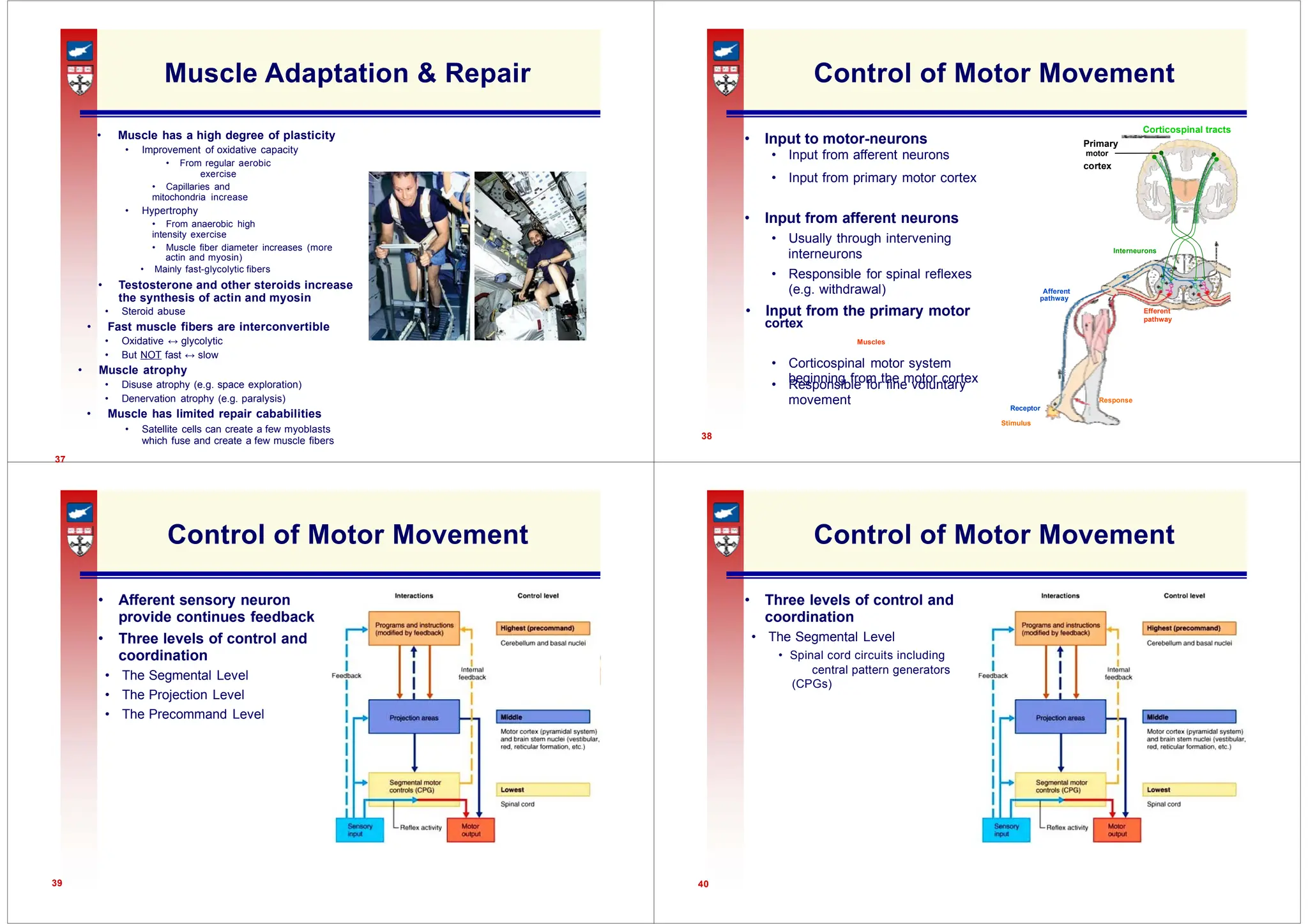
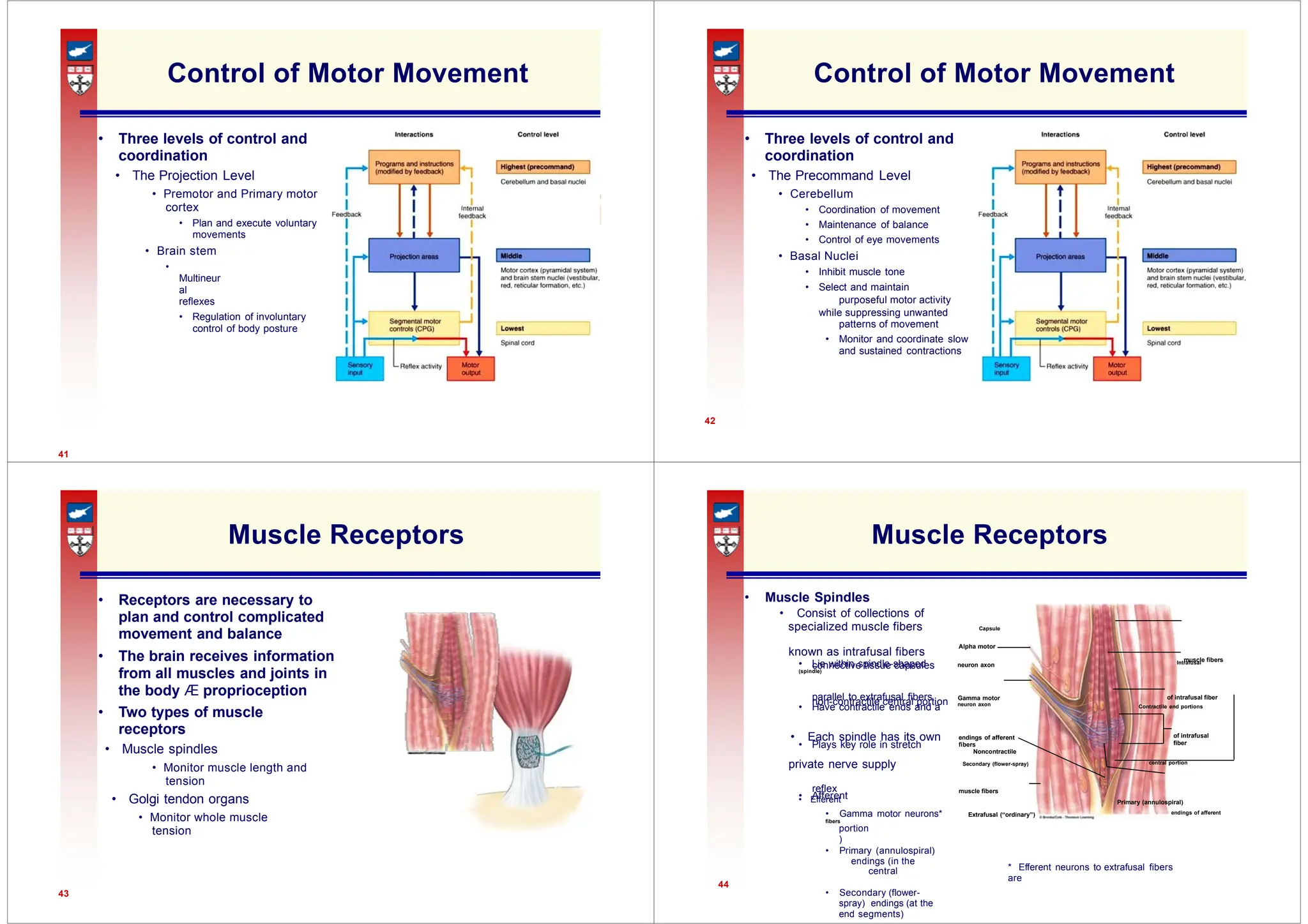
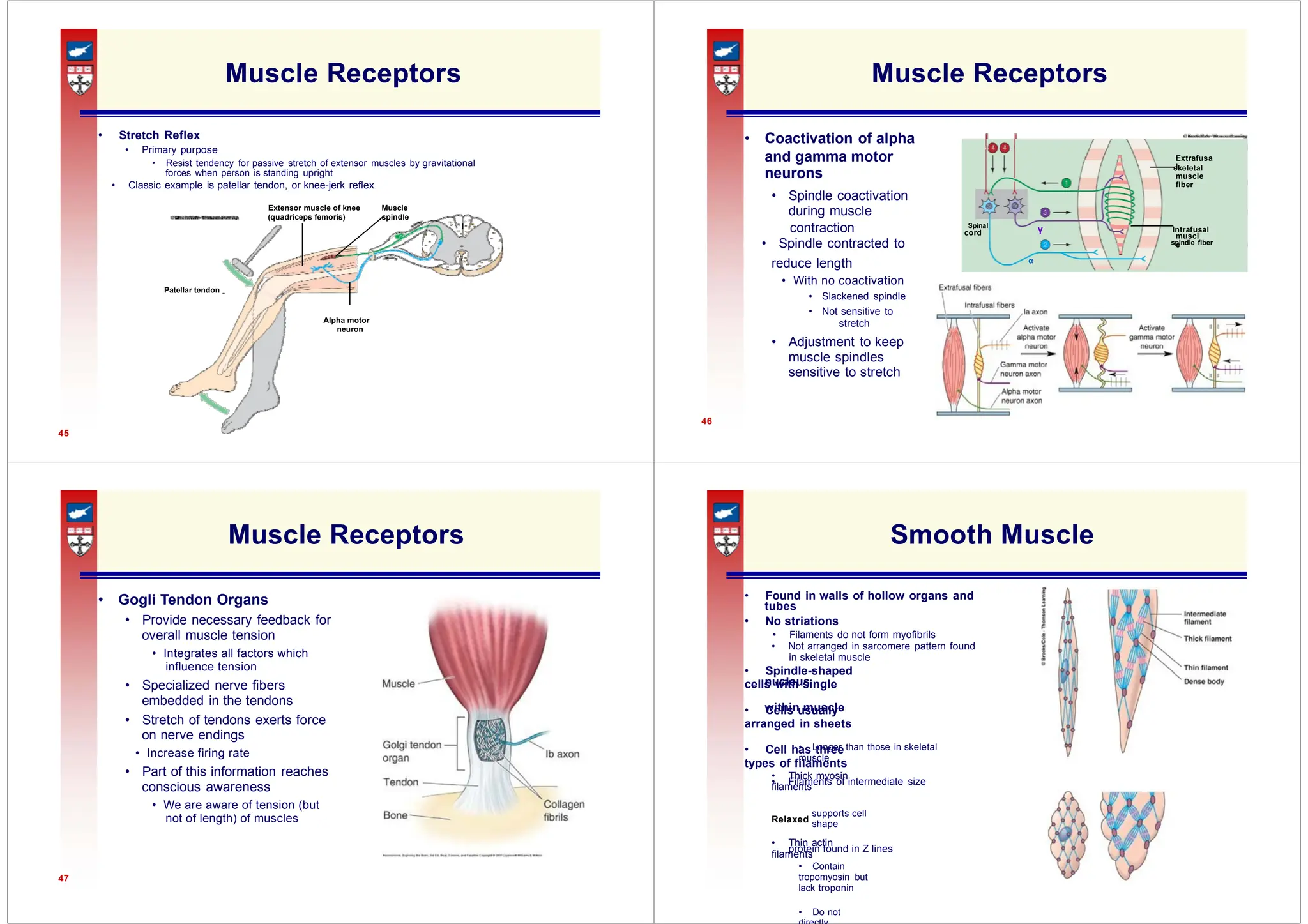
The document provides an in-depth overview of the somatic nervous system and muscle physiology, detailing the roles of motor neurons, muscle contraction mechanisms, and structure of skeletal muscle fibers. It discusses the neuromuscular junction and its susceptibility to various toxins and diseases while explaining the sliding filament theory and excitation-contraction coupling. Additionally, the document covers the types of muscle fibers, energy metabolism during muscle activity, and factors influencing muscle fatigue and performance.