This document provides information about various soft tissue sarcomas:
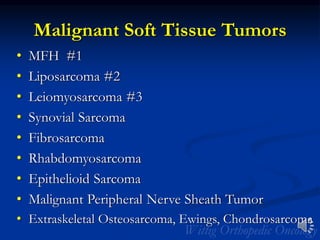
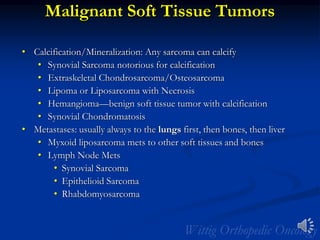
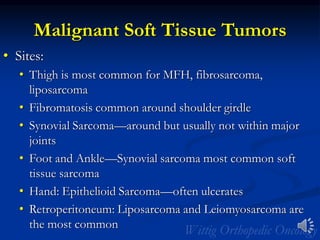
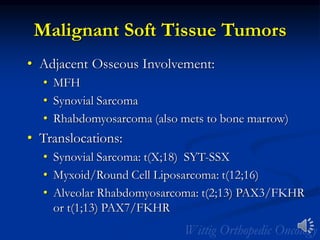
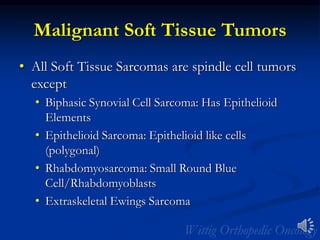
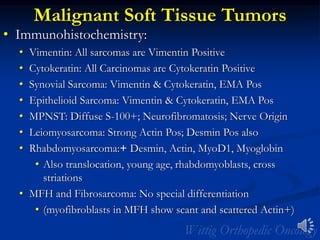
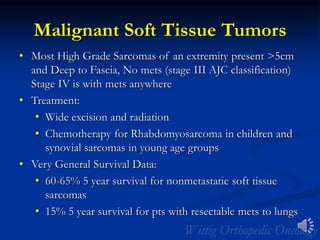
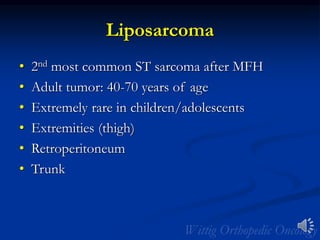
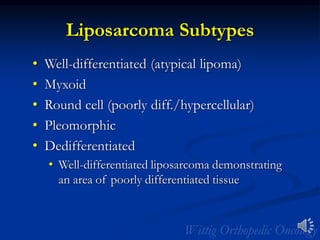
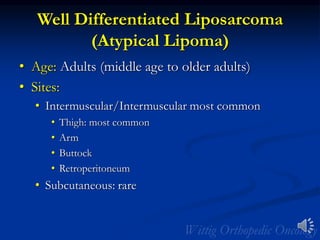
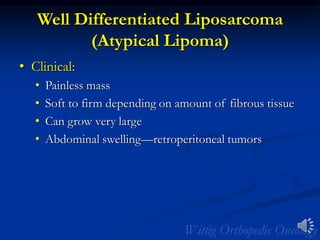
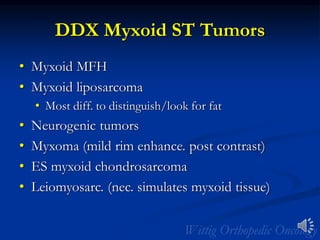
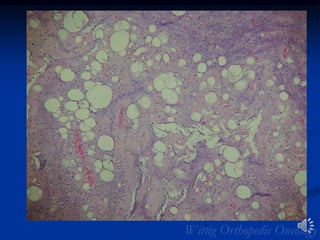
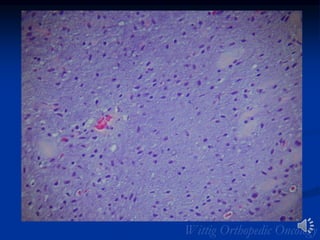
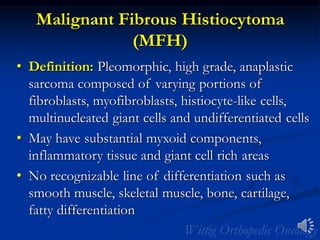
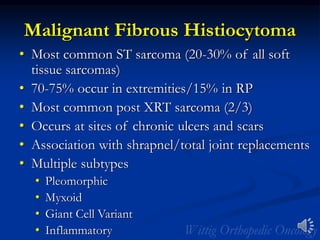
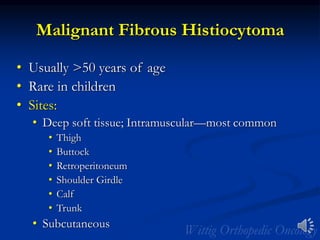
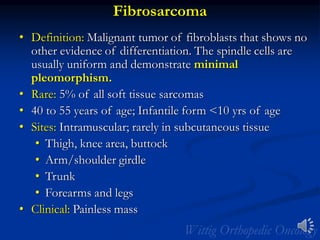
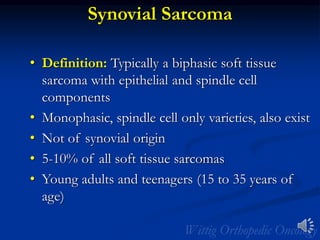
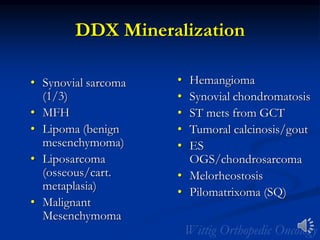
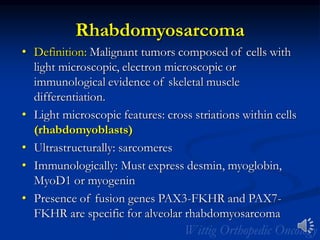
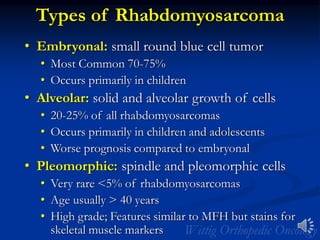
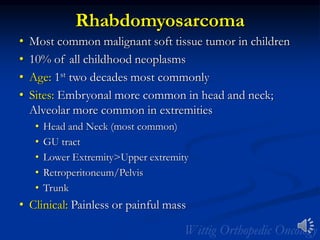
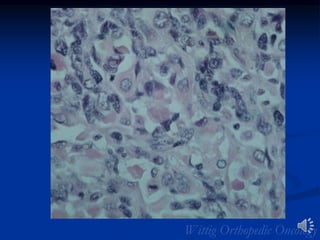
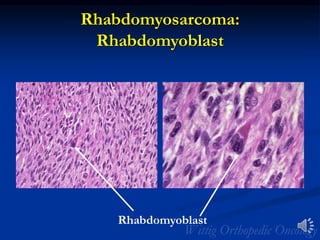
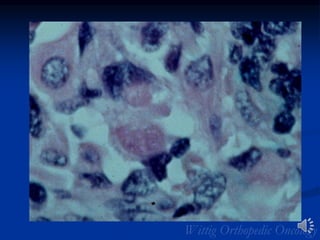
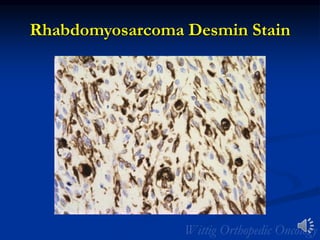
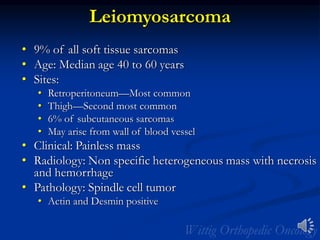
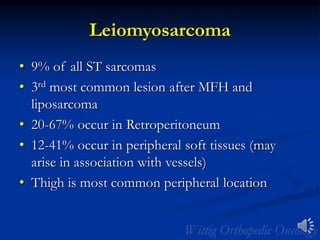
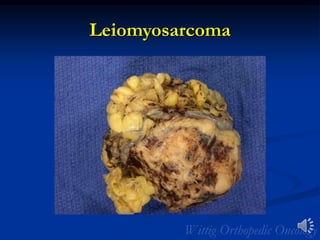
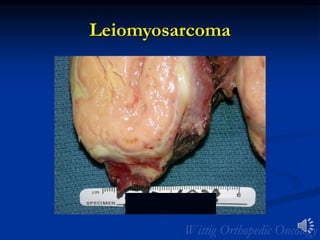
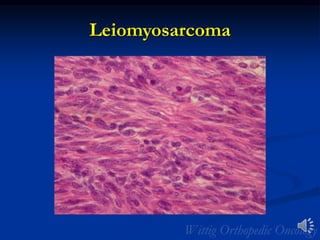
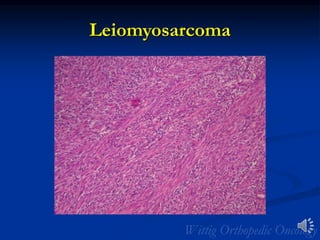
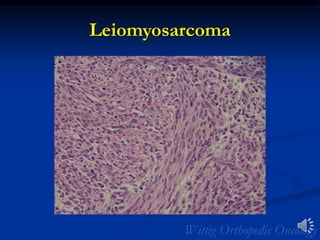
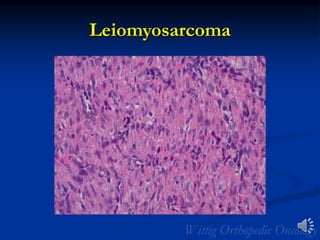
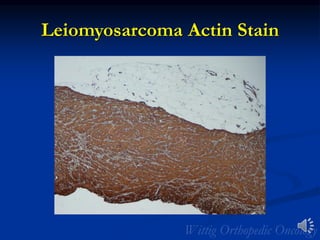
- It discusses the most common types of soft tissue sarcomas including malignant fibrous histiocytoma, liposarcoma, leiomyosarcoma, synovial sarcoma, and rhabdomyosarcoma.
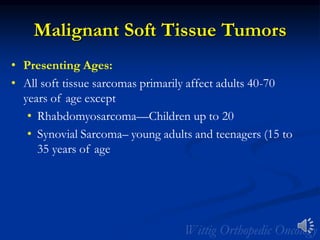
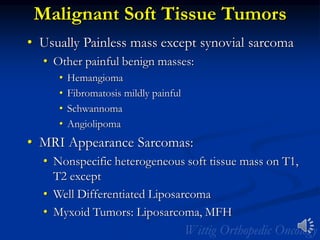
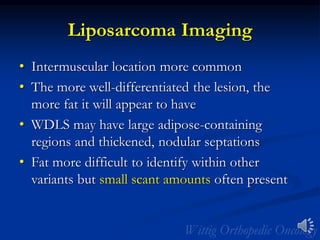
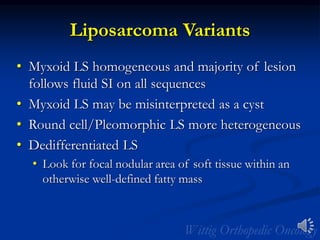
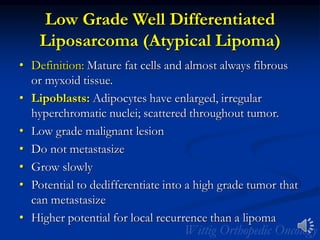
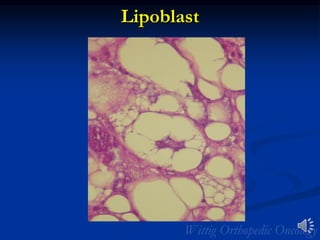
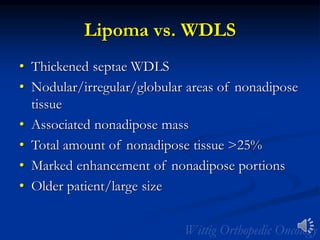
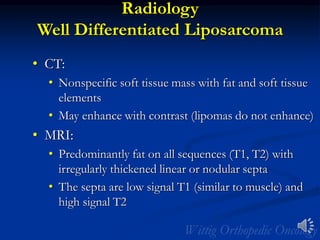
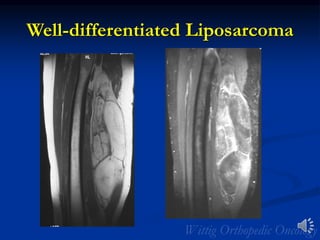
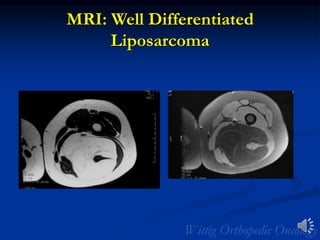
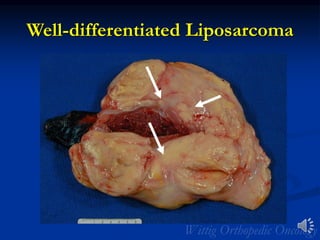
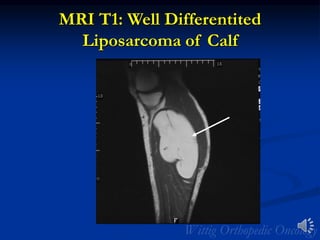
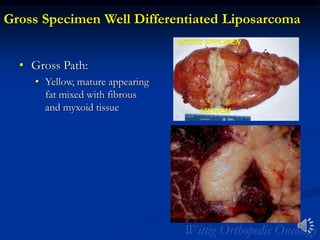
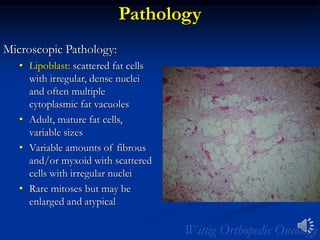
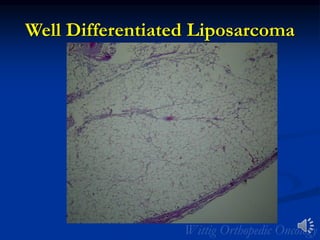
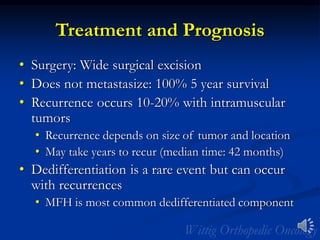
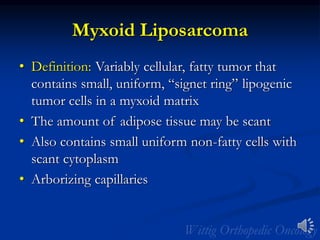
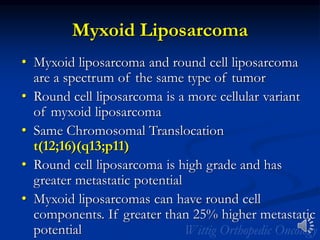
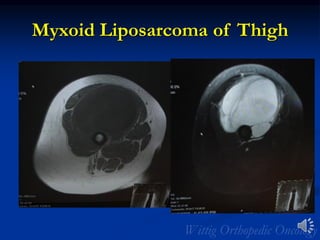
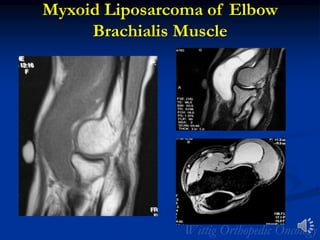
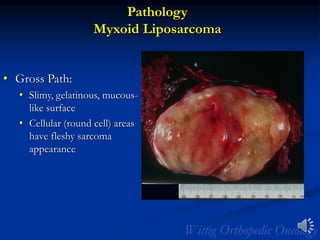
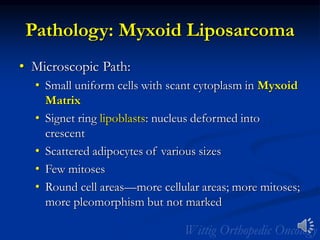
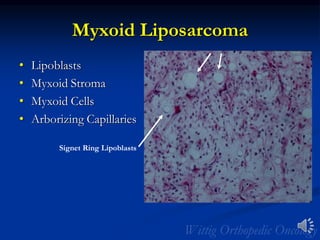
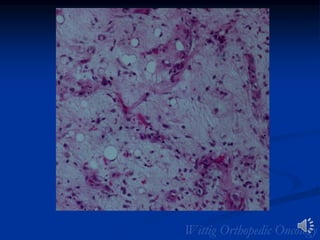
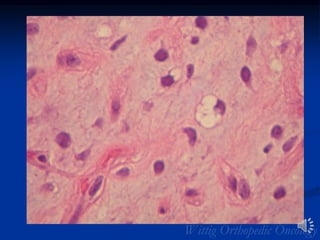
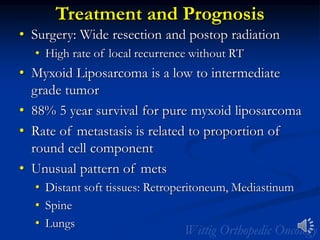
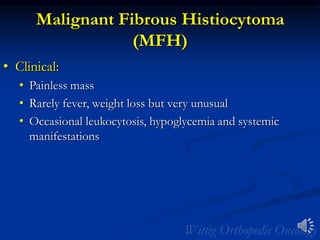
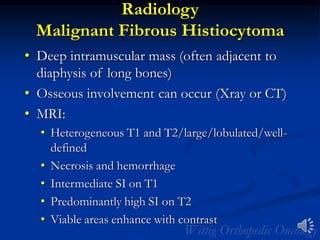
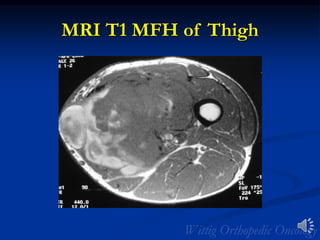
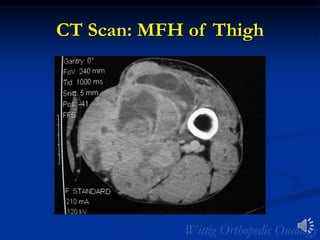
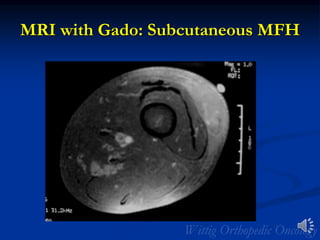
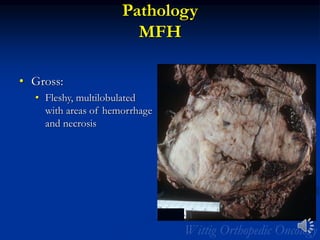
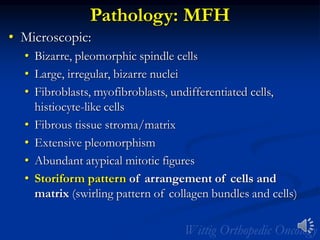
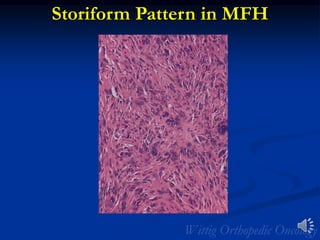
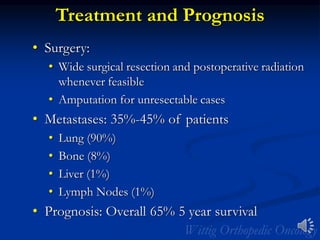
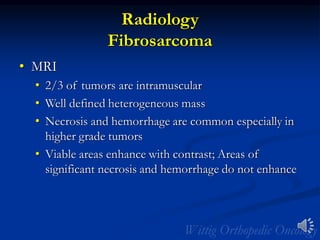
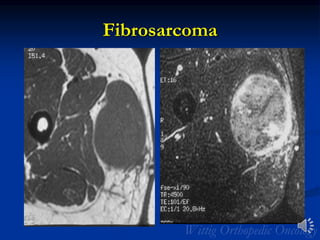
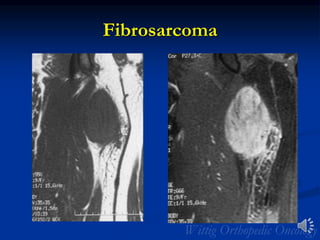
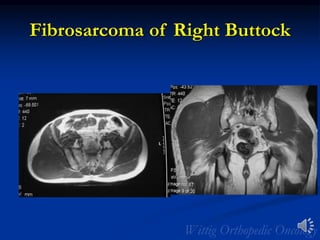
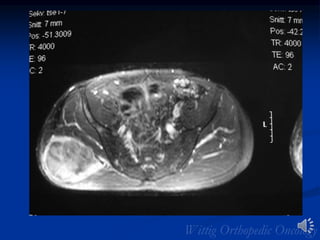
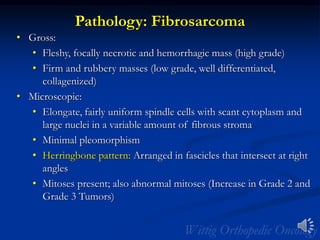
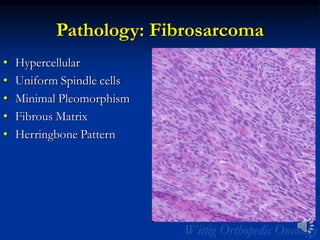
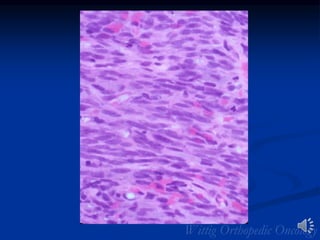
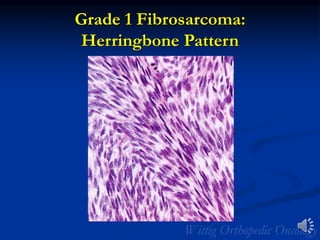
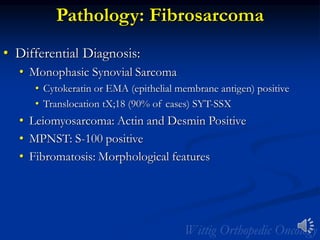
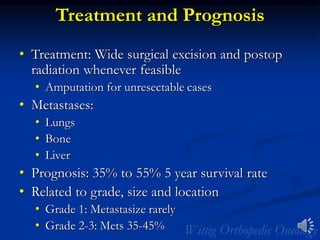
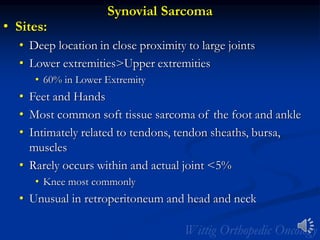
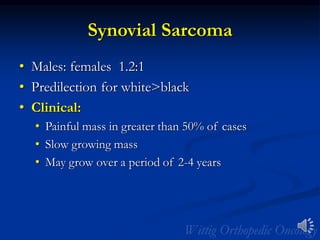
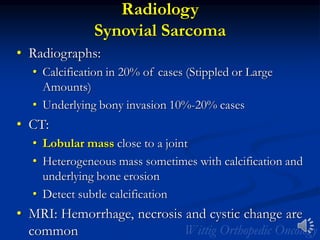
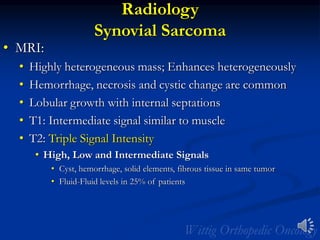
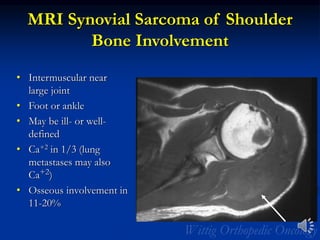
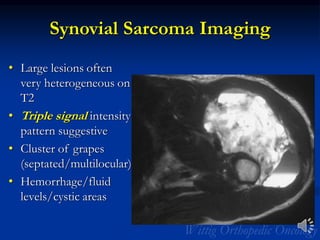
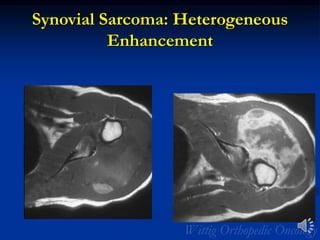
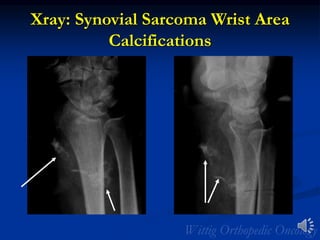
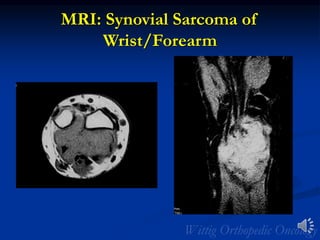
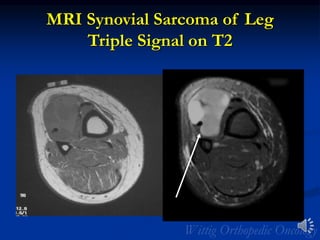
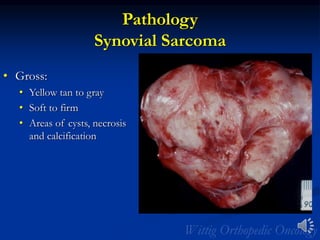
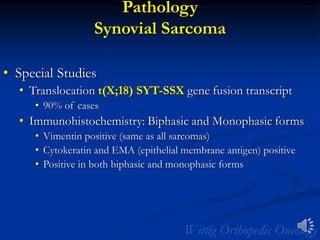
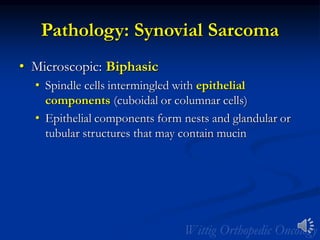
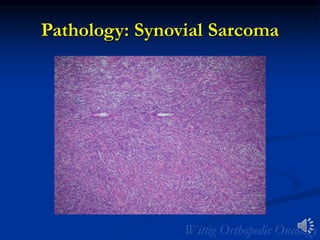
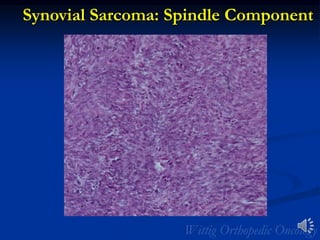
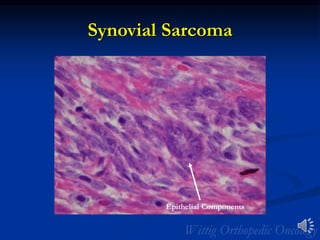
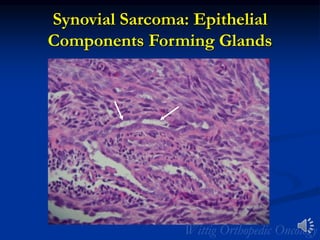
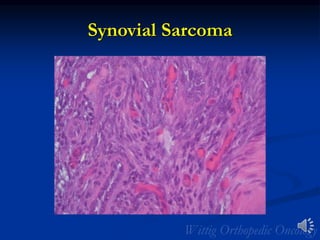
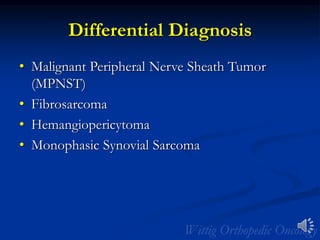
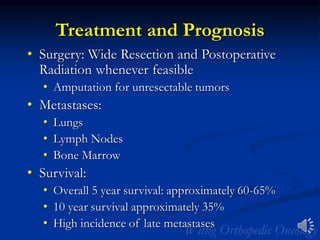
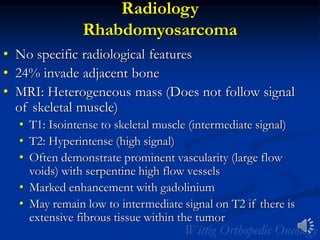
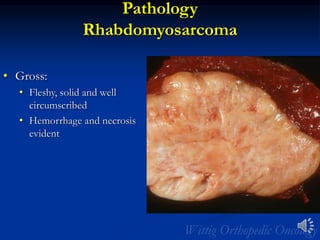
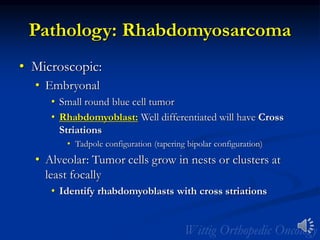
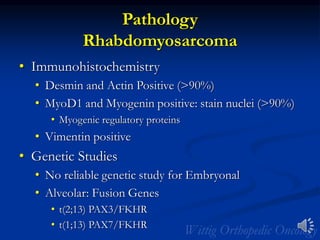
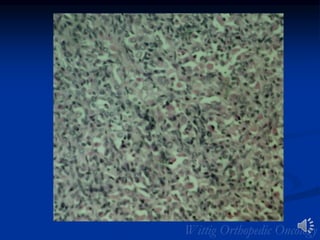
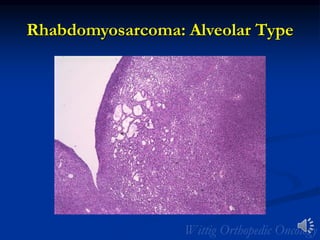
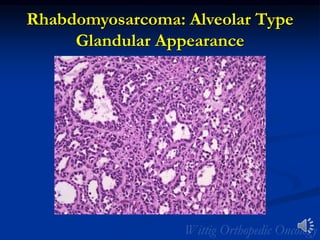
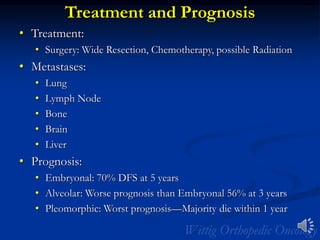
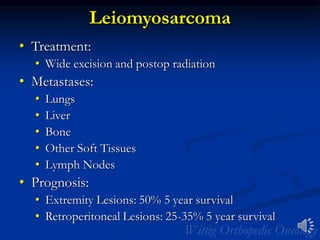
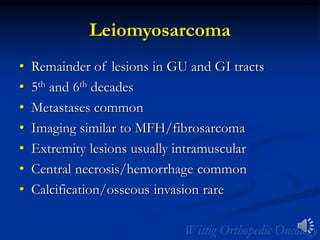
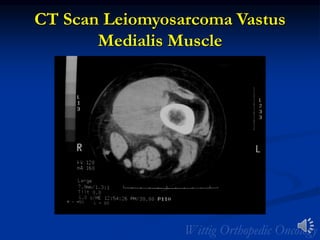
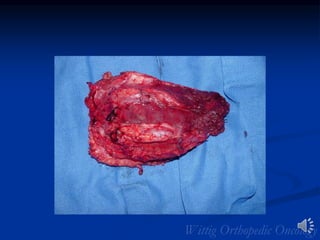
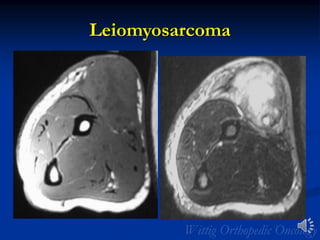
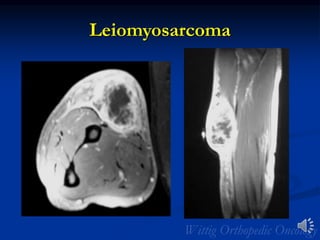
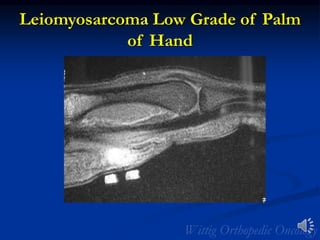
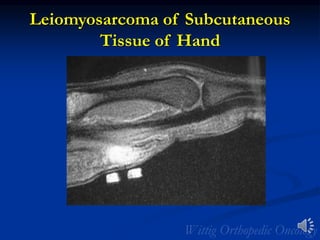
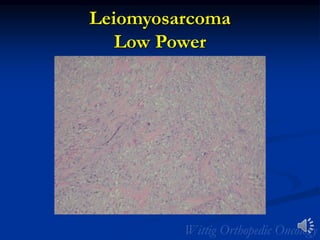
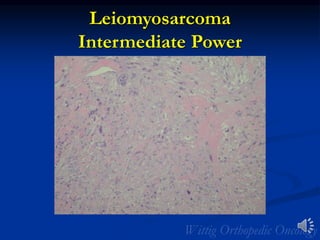
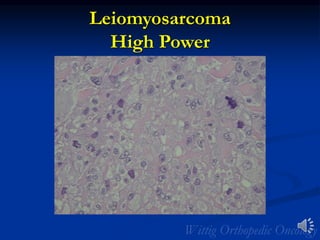
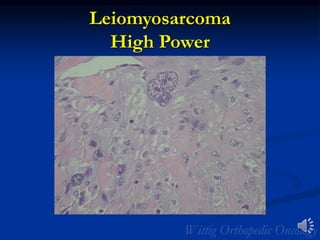
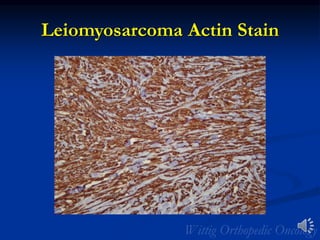
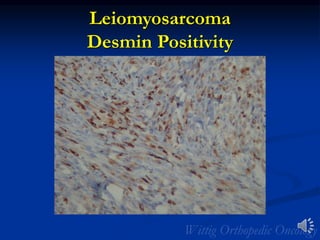
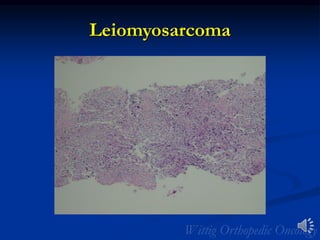
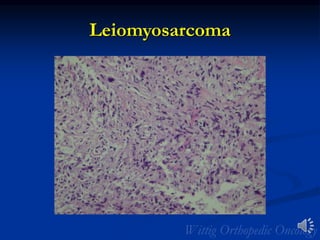
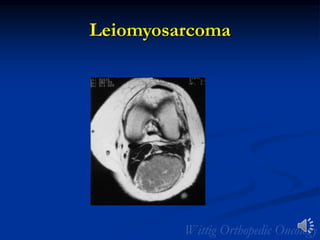
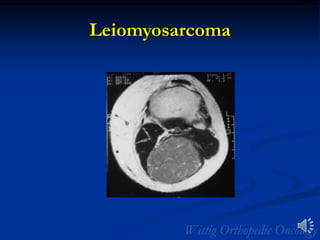
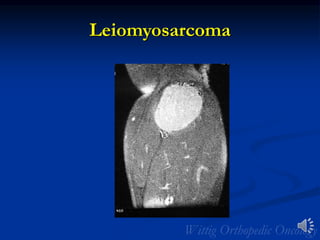
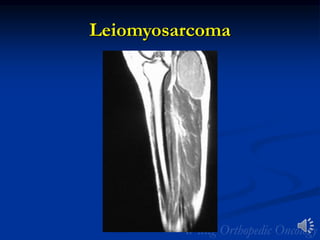
- It provides details on the presentation, imaging appearance, pathology, treatment and prognosis for each type. Common characteristics and differences between subtypes are described.
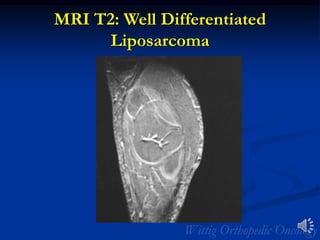
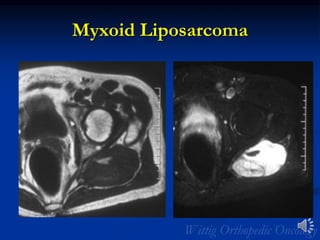
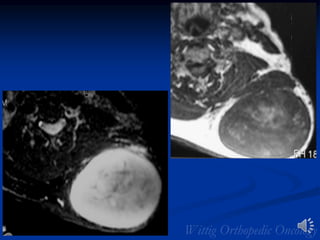
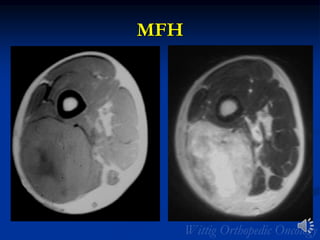
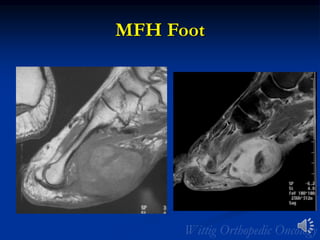
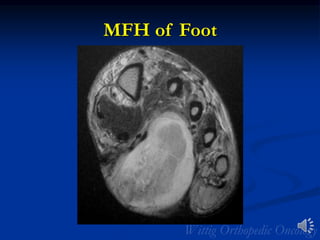
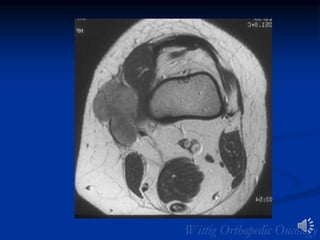
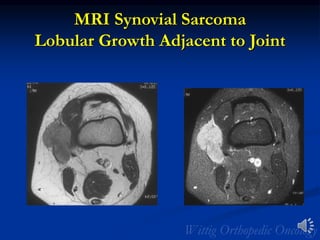
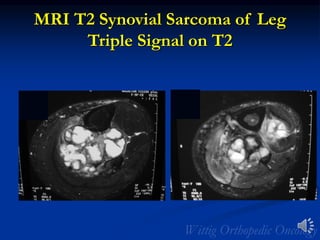
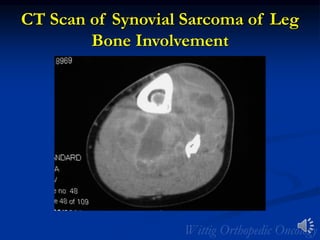
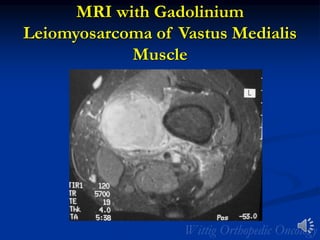
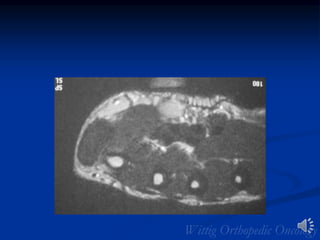
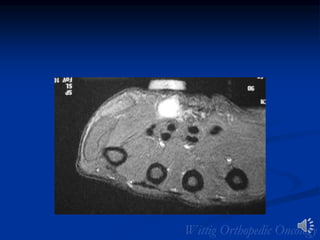
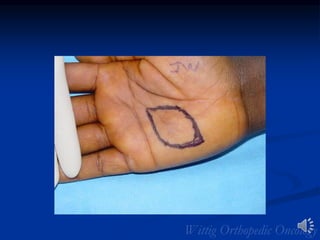
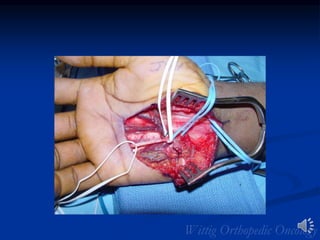
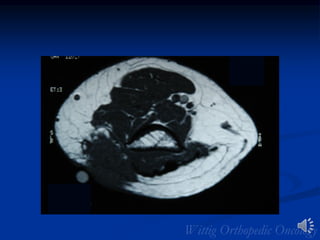
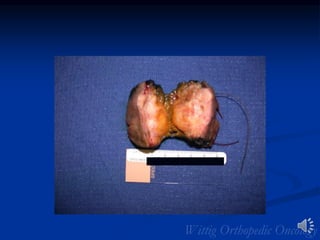
- Radiology images are included to demonstrate the appearance of several soft tissue sarcomas on MRI, CT, and gross pathology specimens.