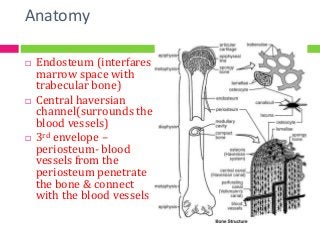
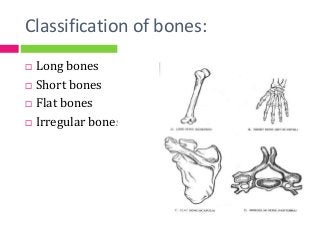
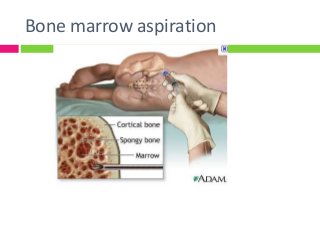
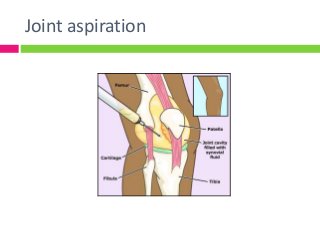
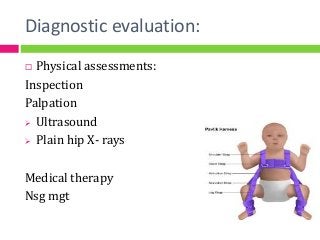
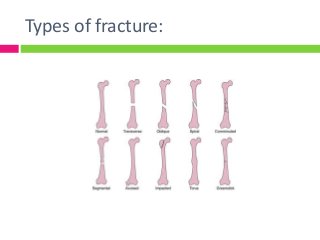
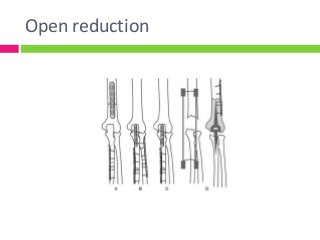
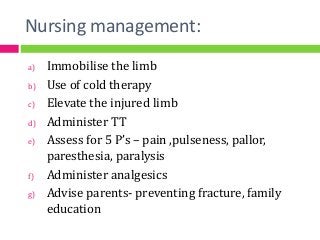
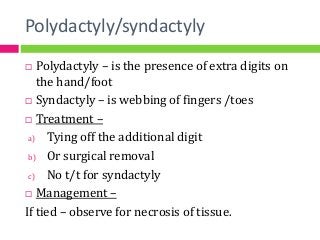
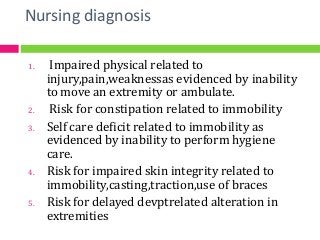
The document summarizes a seminar on the skeletal system presented by Mr. Arvind Joshi. It covers the embryology, anatomy, physiology and classification of bones. It also discusses diagnostic criteria and common medical treatments for skeletal issues like fractures, club foot, congenital hip dysplasia, osteomyelitis, and polydactyly/syndactyly. Nursing management is outlined for various conditions and treatments involving casting, traction, splinting and bracing. Recent advances in treating skeletal issues are also mentioned.