This document provides an introduction and background on alcoholism. It defines alcoholism as a chronic disease influenced by genetic and environmental factors, characterized by impaired control over drinking and denial. It notes alcohol is widely consumed and abuse is a major problem in many countries. Later sections discuss psychological and behavioral explanations for alcoholism, the objectives and need for studying alcohol abuse among caretakers in medical wards, and a review of previous literature on definitions and studies of alcoholism.







![35
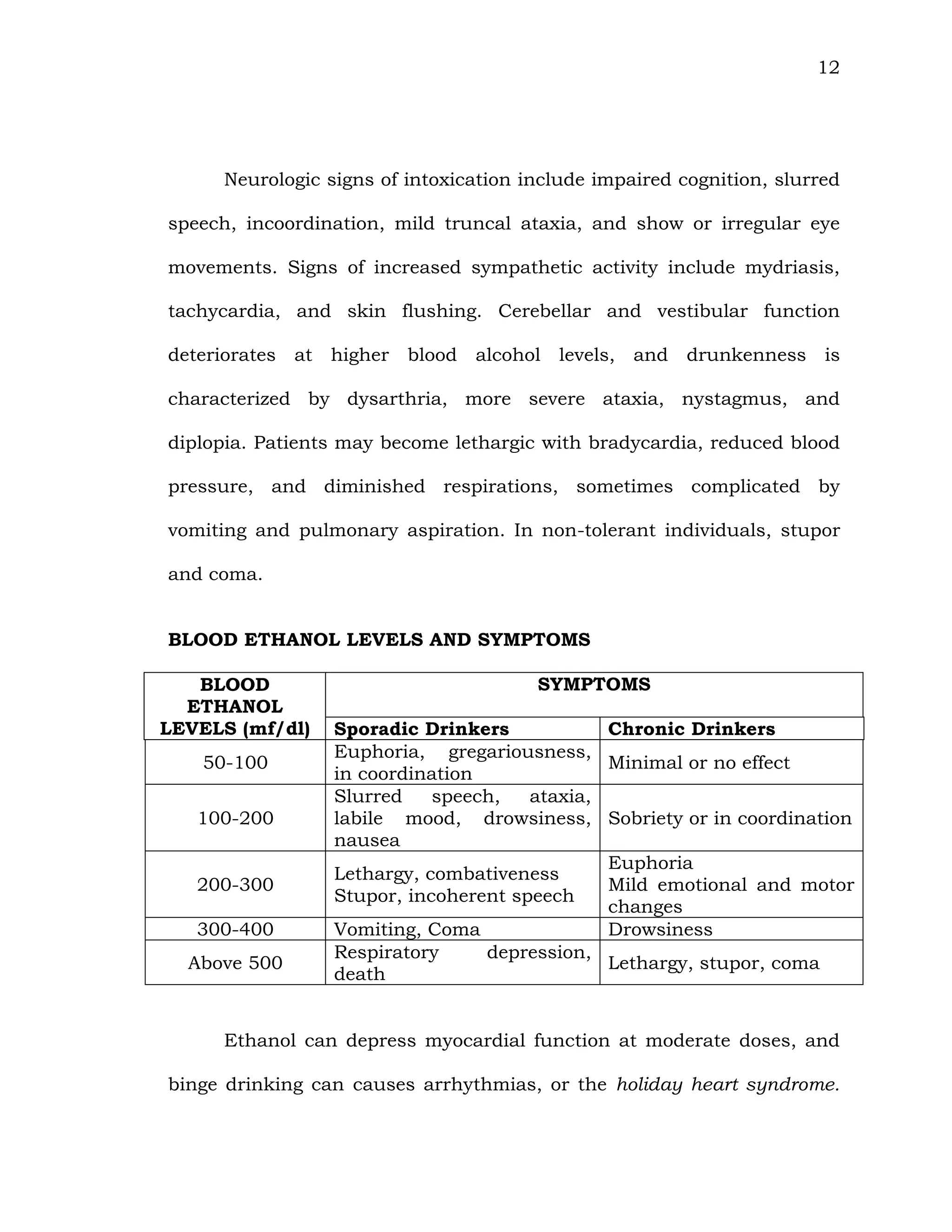
Alcohol and Lymphatic System
There is lower risk of developing lymphoma in alcoholics.
Alcohol consumption may cause pain at site of lymph mode or
extra lymphatic involvement in patients with Hodgkin’s lymphoma.
Psychological
1. Anxiety
2. Depression
3. Personality change
4. Misuse of other durgs
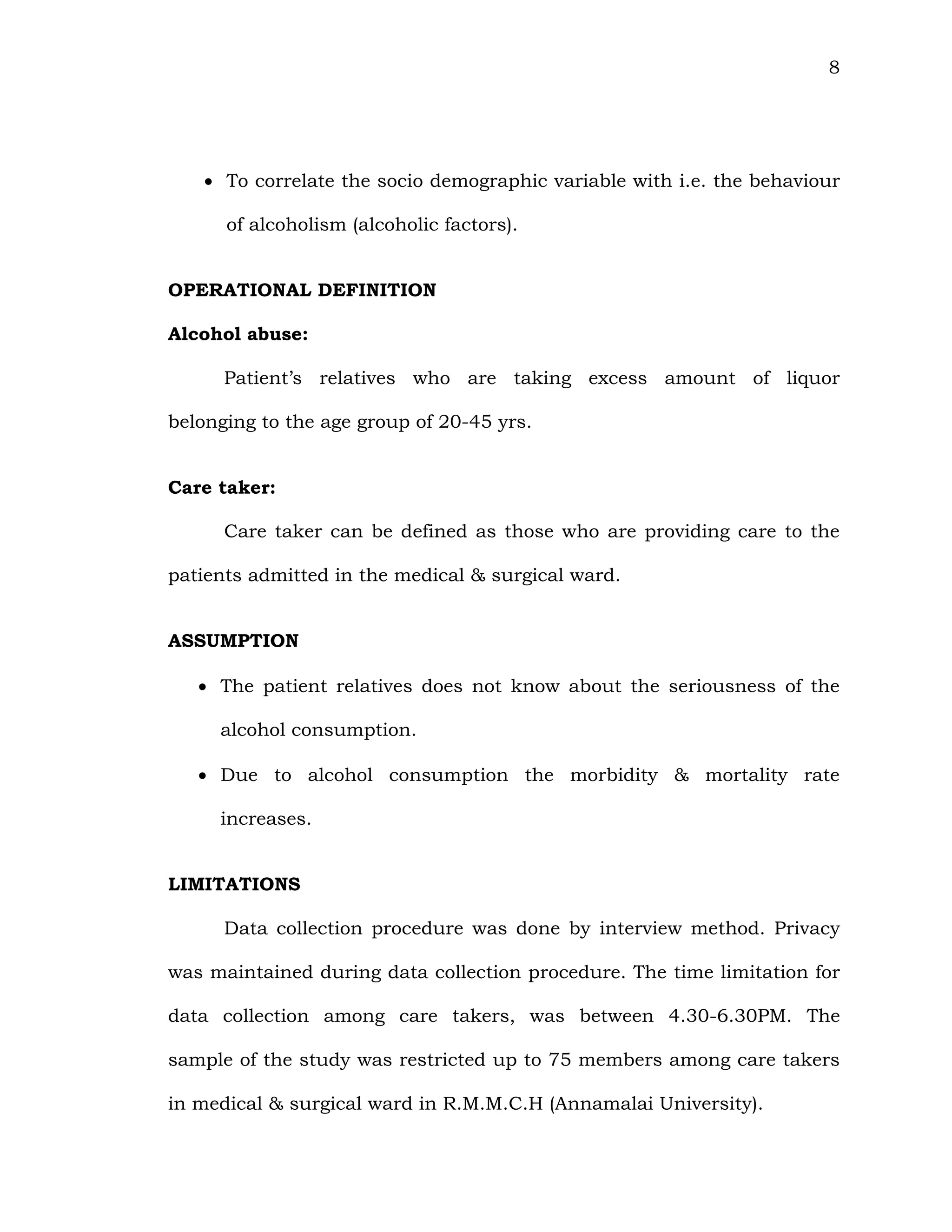
5. Cognitive impairment.
Irene I. Elluns, Matt McGue et al, (2004) conducted a study on The
effect of parental alcohol and drug disorders on adolescent personality.
The relationship of parental alcohol or drug diagnosis to offspring
personality was examined in a population-cased sample of 17- year-old
twins [568 girls and 479 boys] participating in the Minnesota twin family
study. Whether offspring-personality characteristics 1) are specific to the
type of substance use disorder in parents (alcohol versus drug) and 2)
are found in high-risk offspring without substance use disorders was
investigated.](https://image.slidesharecdn.com/sharmiladevib-221128012540-bab11a24/75/Sharmila-Devi-B-Sc-Nursing-doc-35-2048.jpg)


![39
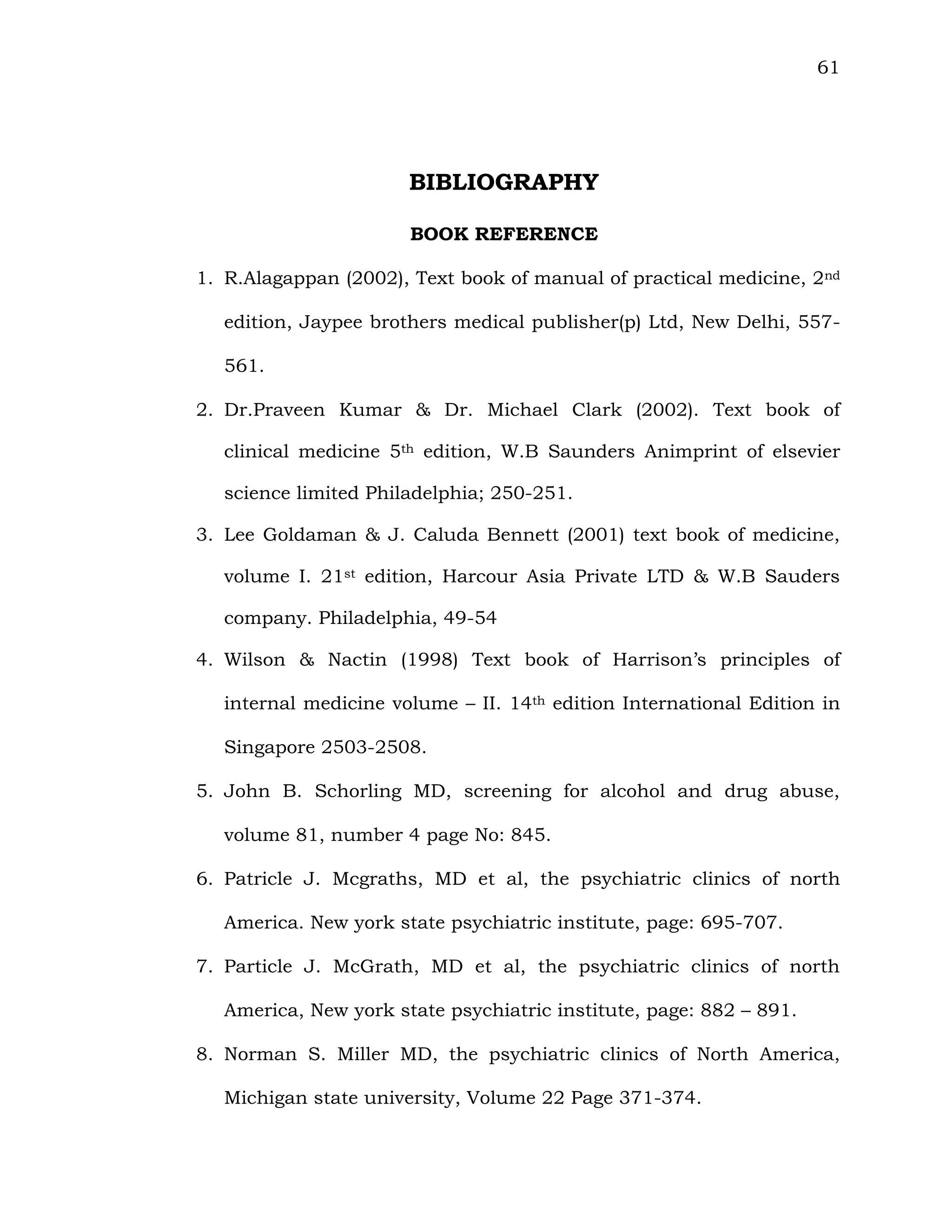
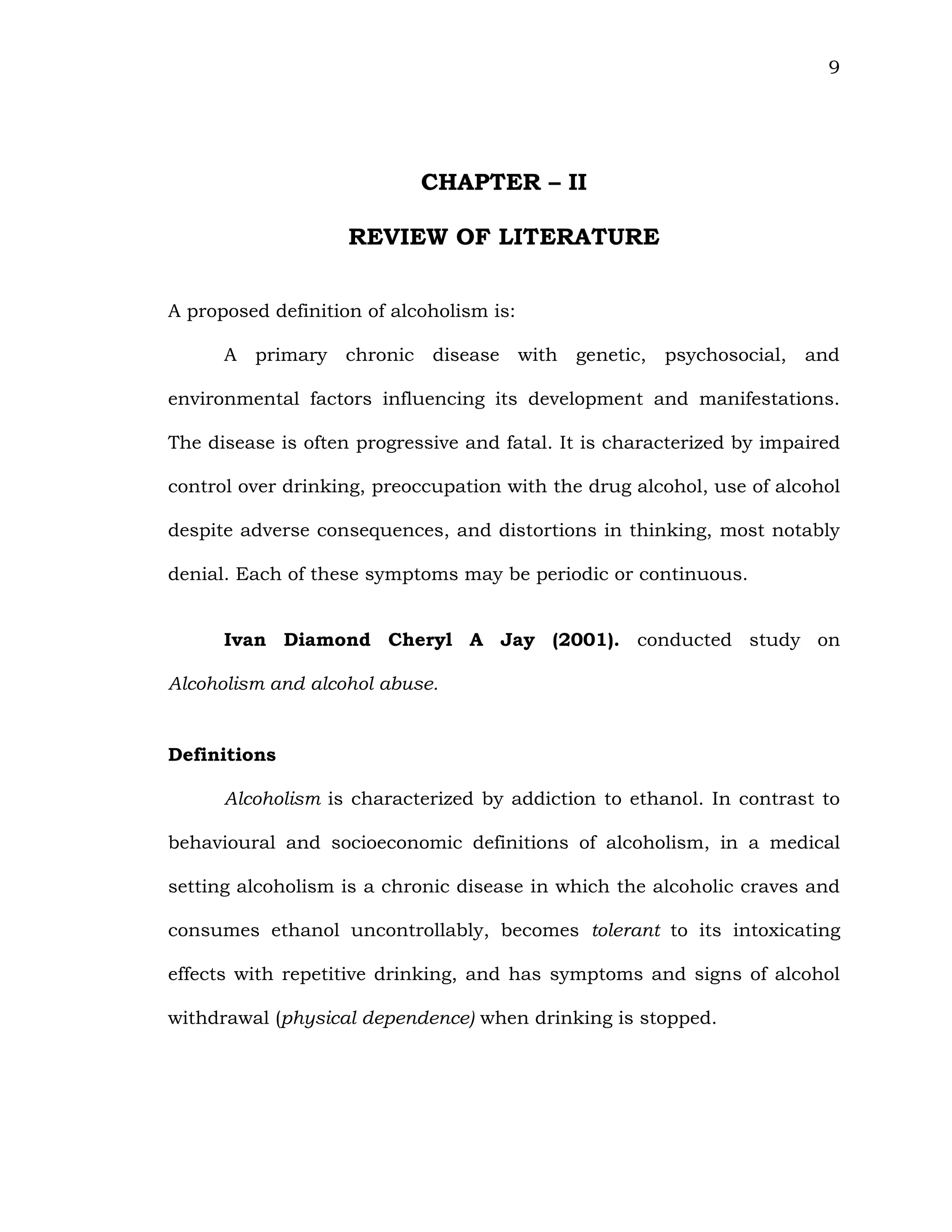
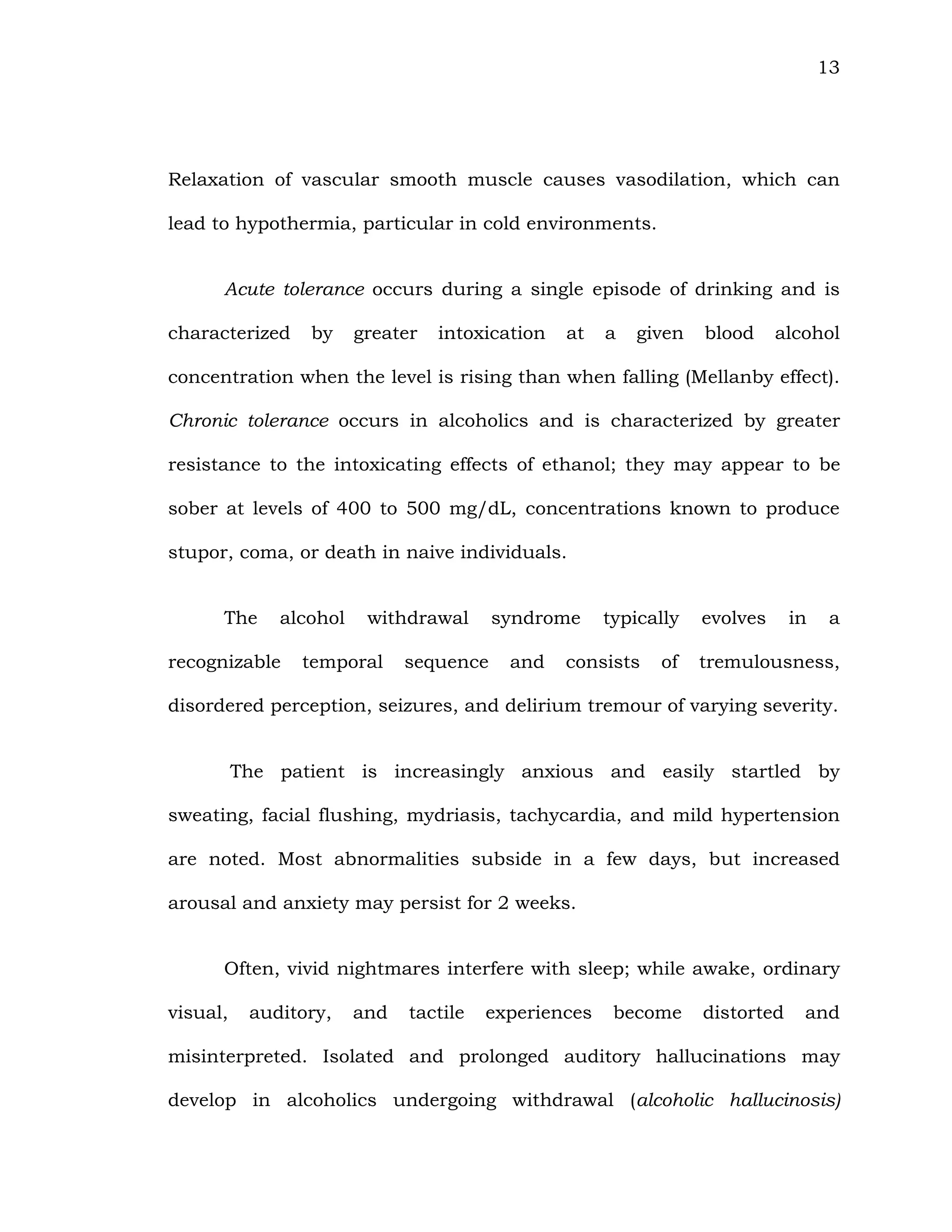
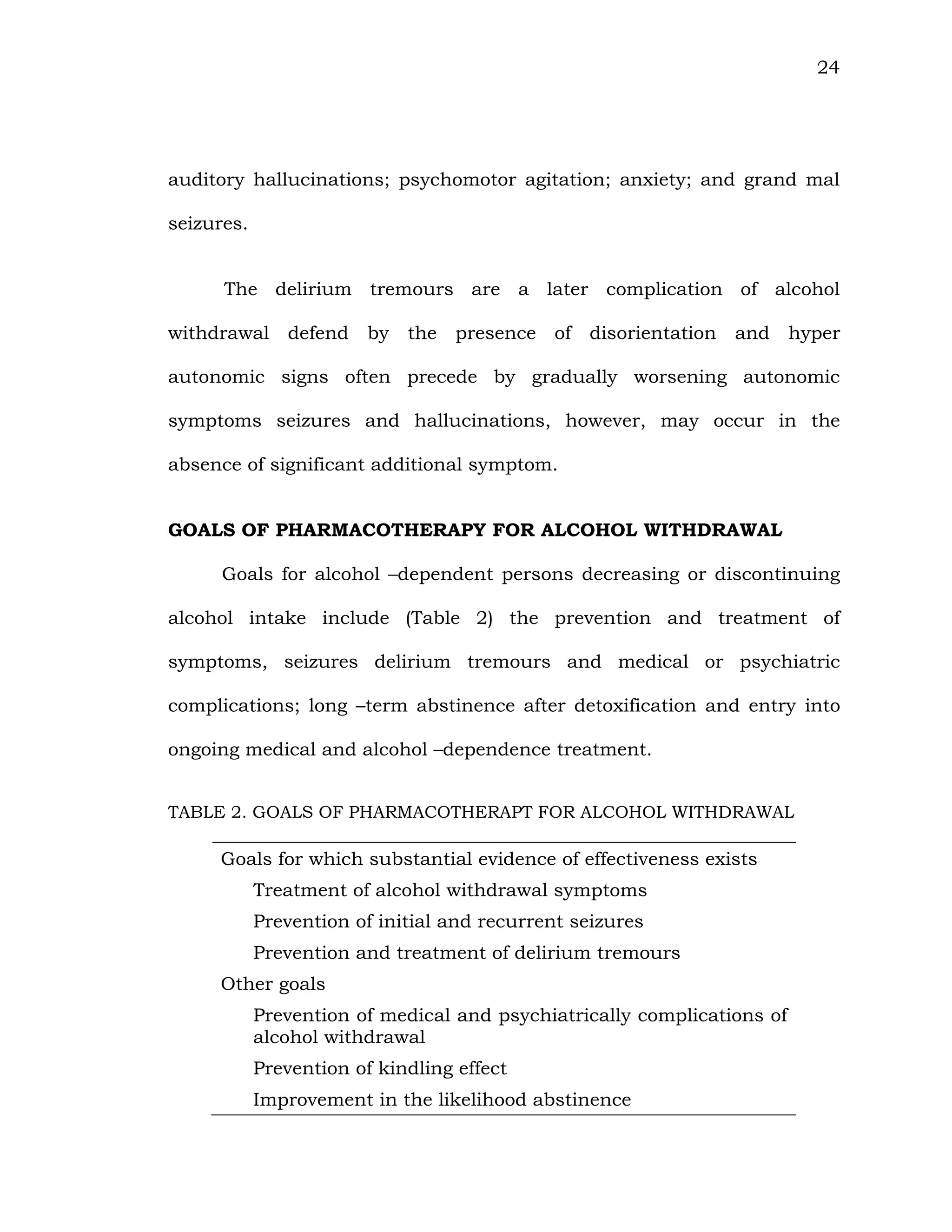
Results: Survey respondents with sleep disturbances because of worry at
the time of the baseline interview had a twofold higher risk for developing
an alcohol-re-lated problem, relative to those without these sleep
disturbances (odds ratio=2.32, 95% confidence interval [C1]=(1.31-4.09),
with adjustment for selected demographic and clinical variables. Sleep
disturbance because of worry predicted the development of alcohol
problems among respondents with lifetime anxiety disorders and lifetime
dysphoria (odds ratio = 3.82, 95% Cl=1.56-9.38, and odd ratio = 2.71,
95% Cl=1.25-5.91, respectively), but not among those without a history
of anxiety disorders or dysphoria.
Conclusions: Sleep disturbances because of worry may increase risk for
alcohol-related problems. Risk is highest for those with sleep disturbance
and co-occurring anxiety disorders or dysphoria.
Marc A. Suhuckit, M.D., Tom L. Smith, Ph.D., et al (1998) in
experimented about the Clinical relevance of the Distinction Between
Alcohol Dependence With and Without a Physiological Component.
Objective: DSM-IV indicates that diagnoses of substance dependence
should be further characterized with regard to the presence of a
physiological component, defined by tolerance or withdrawal. This study
evaluated the possible meaning of this distinction in alcohol-dependent
men and women.](https://image.slidesharecdn.com/sharmiladevib-221128012540-bab11a24/75/Sharmila-Devi-B-Sc-Nursing-doc-39-2048.jpg)