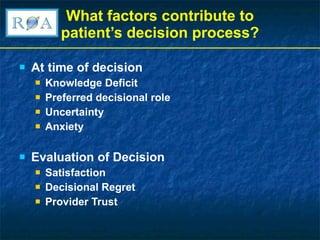
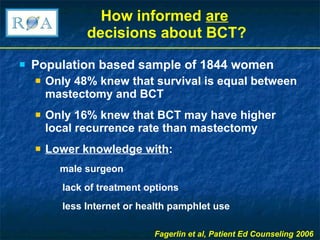
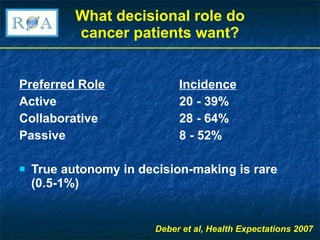
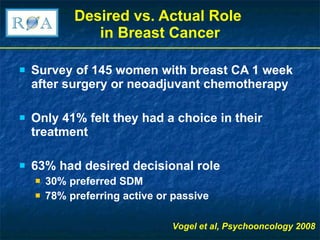
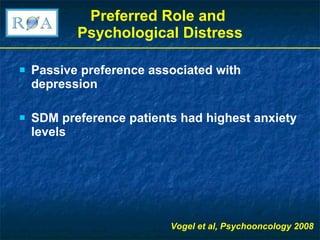
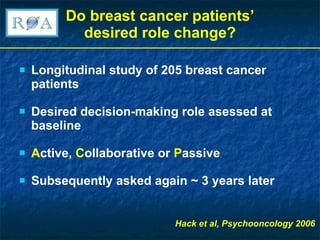
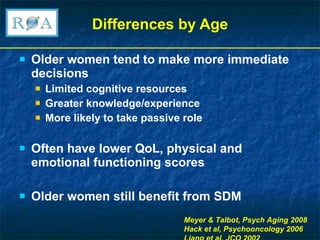
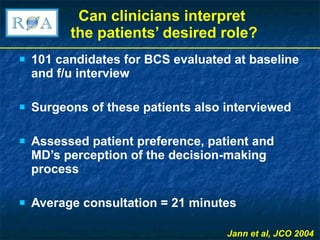
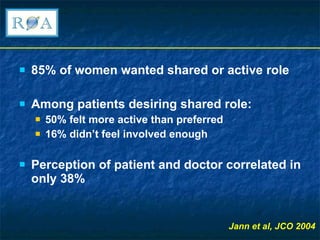
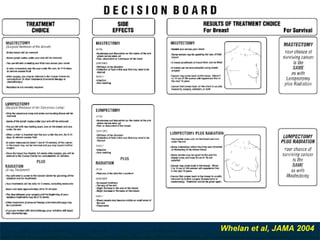
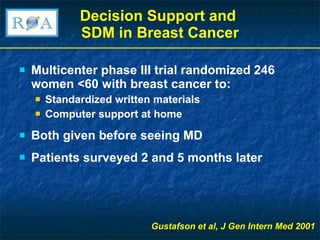
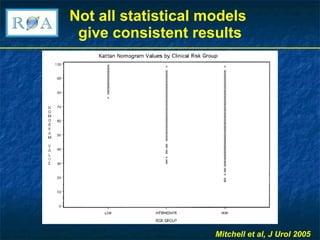
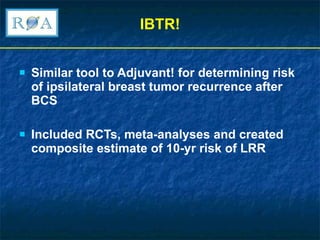
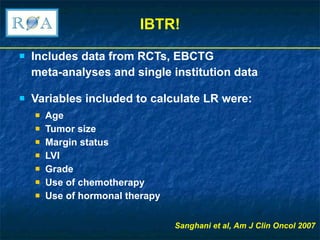
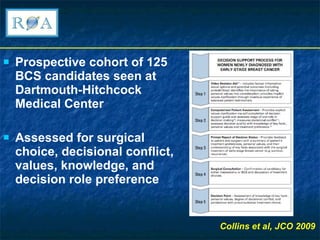
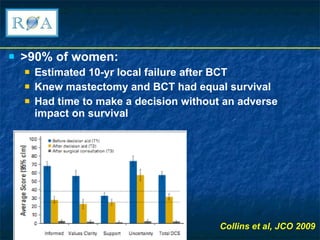
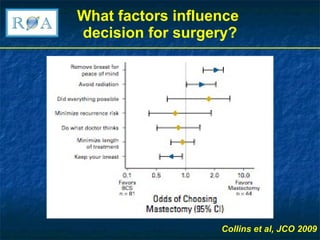
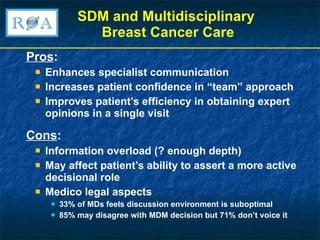
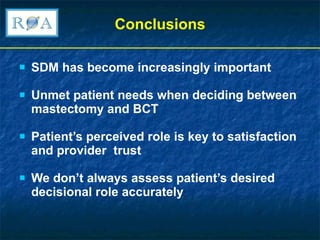
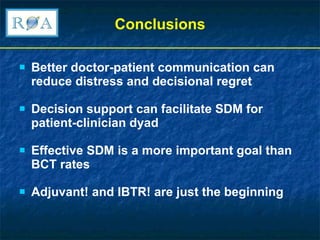
The document discusses the importance of shared decision making (SDM) in breast conserving therapy (BCT) for breast cancer patients, emphasizing the need for patient engagement and informed consent. It explores various factors influencing patient decision-making, such as knowledge deficits and preferences for active or passive roles, along with the role of decision support tools in enhancing patient understanding and satisfaction. The conclusion highlights that effective SDM can improve patient experiences and outcomes, stressing that communication between patients and clinicians is crucial in navigating treatment options.