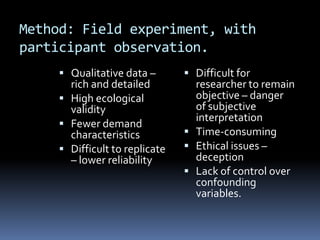
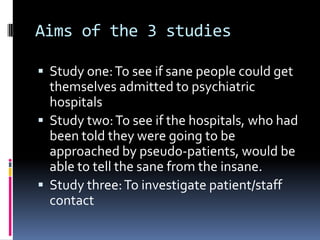
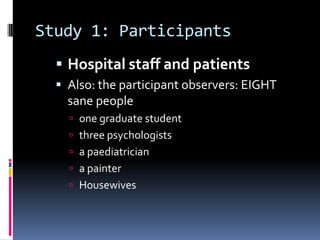
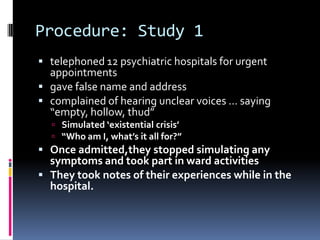
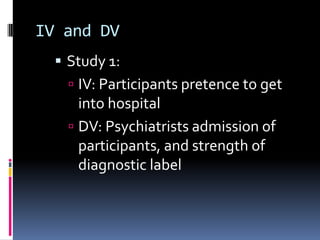
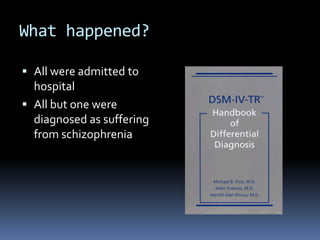
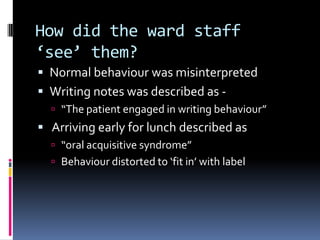
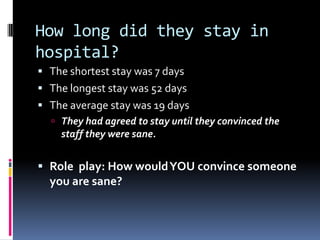
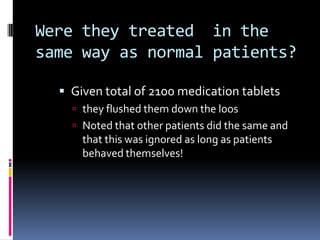
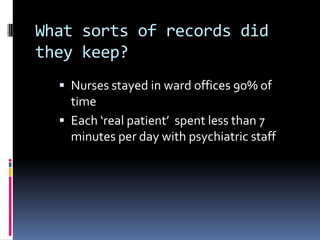
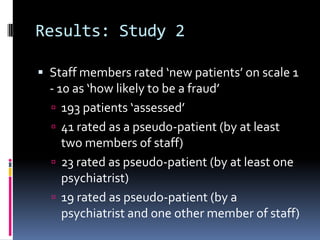
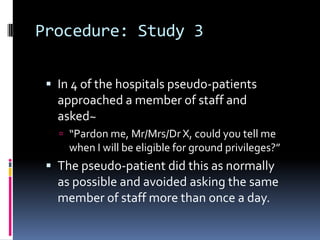
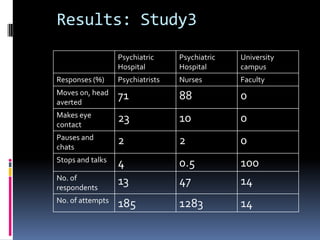
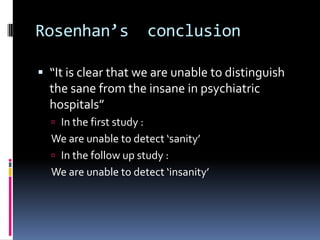
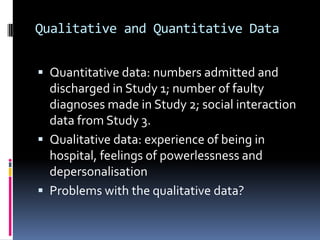
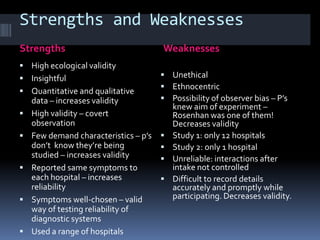
Rosenhan conducted a famous study where sane individuals successfully gained admission to psychiatric hospitals by feigning auditory hallucinations. All were diagnosed with schizophrenia and their normal behavior was misinterpreted by staff. In a follow up study, hospital staff also could not distinguish real patients from those falsely claimed to be admitted. The study highlighted the depersonalization and powerlessness felt by patients when subjected to psychiatric labels and institutionalization rather than community-based care focused on behavior.