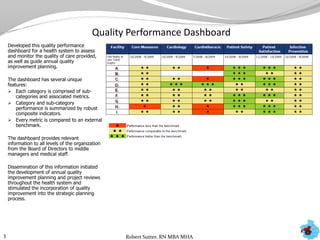
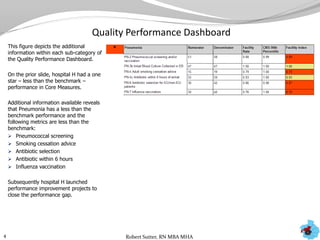
The document outlines statistical analyses and performance dashboards developed by Robert Sutter using patient data to identify opportunities for performance improvement. Key points include:
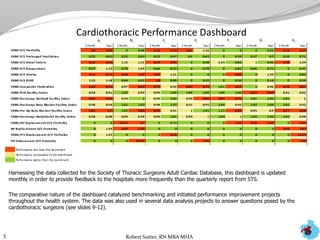
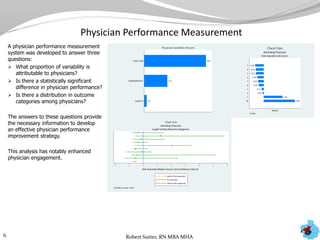
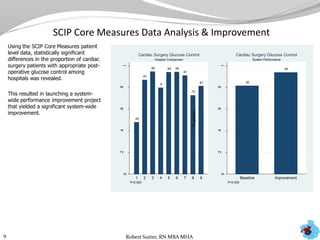
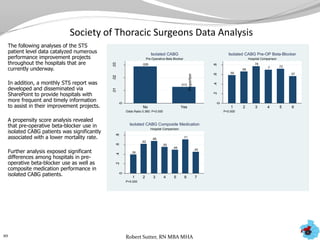
- Dashboards were created to monitor quality performance metrics and catalyze annual improvement planning across multiple health systems.
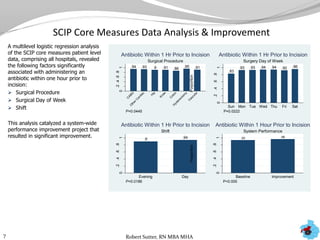
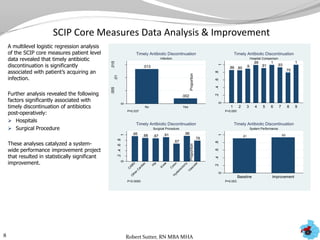
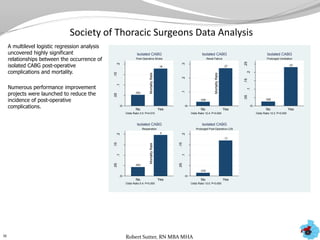
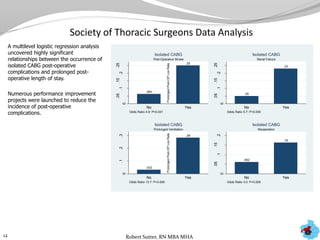
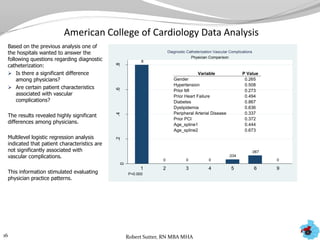
- Additional analyses of SCIP, STS, and ACC data revealed factors associated with outcomes and complications. This stimulated numerous system-wide performance projects.
- Physician and hospital comparisons using the data identified best practices and areas for benchmarking, focusing improvement efforts.