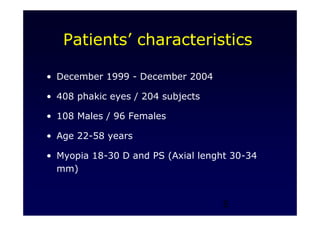
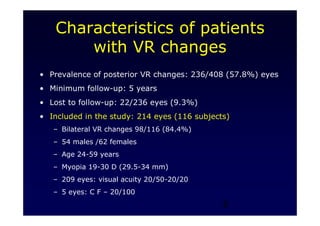
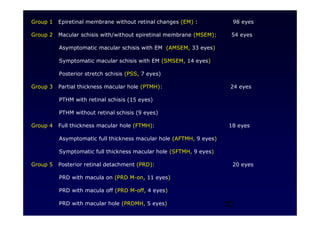
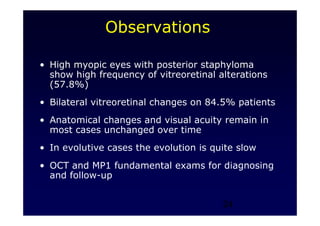
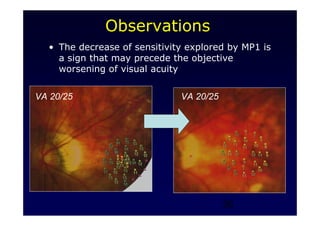
1. The study examines vitreoretinal interface modifications in highly myopic eyes with posterior staphyloma over a 5-year follow up period.
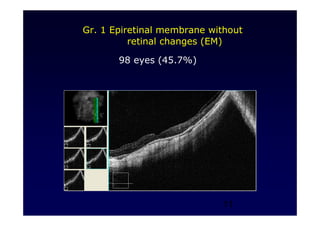
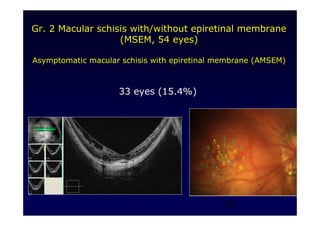
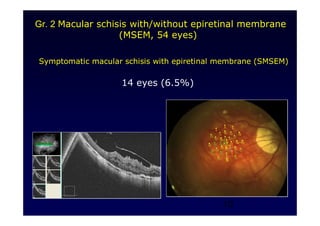
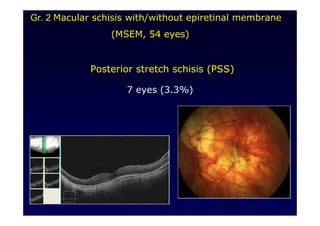
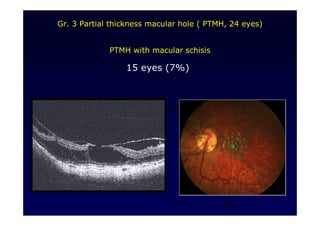
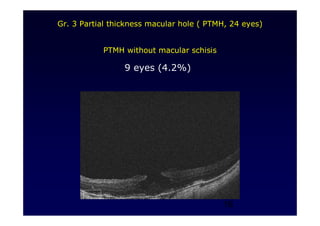
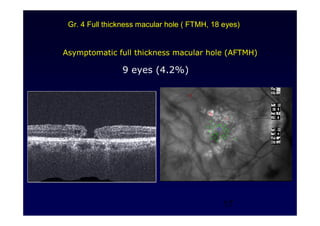
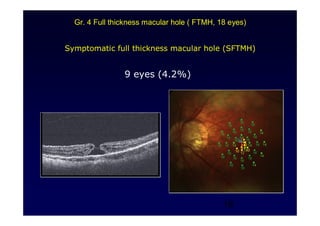
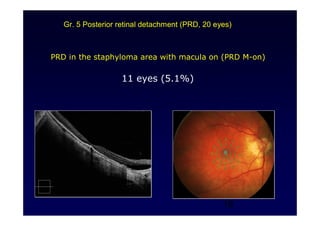
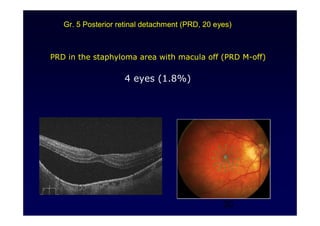
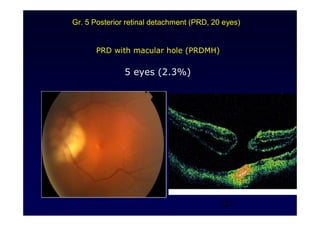
2. 214 eyes were included and classified into 5 groups based on anatomical changes observed. The most common finding was epiretinal membrane without retinal changes (45.7% of eyes).
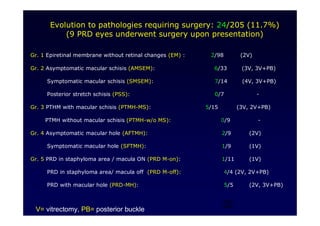
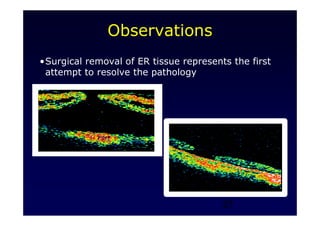
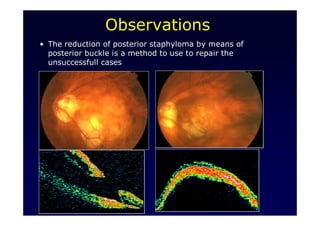
3. Evolution requiring surgery occurred in 11.7% of eyes, with various surgical approaches used depending on the classification group.
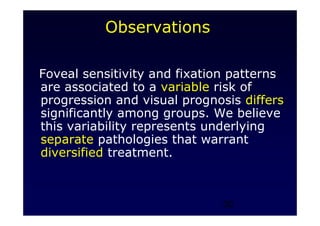
4. Vitreoretinal alterations in highly myopic eyes represent a spectrum of conditions that are not fully classified, and disease progression and surgical timing remain uncertain and need standardization.